An Introduction into Techniques for Prevention of Stage One Pressure... in the Pediatric Population
advertisement

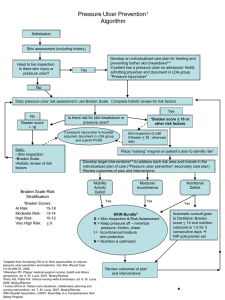
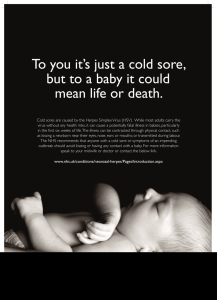
An Introduction into Techniques for Prevention of Stage One Pressure Sores in the Pediatric Population Philip Gates MD, Justina Shipley, CO, MEd, FAAOP Shriners Hospital for Children, Shreveport, Louisiana OBJECTIVE: Introduce methods of prosthetic and orthotic device fabrication, fitting criteria, use of the Braden Scale, and parental education techniques to help the prevention of stage one pressure sores in the pediatric population. DISCUSSION: Pressure Sores, Pressure Ulcers or Decubitus Ulcers Pressure sores must be taken seriously; if left unchecked, a pressure sore can lead to amputation or in the worst case death. Even when well cared for, a pressure sore can still become infected such as was the case with Christopher Reeve in October 2004. Christopher had the best care and was looked after by dedicated staff at Northern Westchester Hospital, but still his sore became severely infected, resulting in a serious systemic infection. This in turn led to a heart attack and coma from which he did not recover. Check yourself for red marks and sores daily, it should be a routine which is as second nature as brushing your teeth. History of the Braden Scale The Braden Scale for Predicting Pressure Sore Risk was developed during a Robert Wood Johnson Teaching Nursing Home project and while writing an NIH proposal to study pressure ulcer risk factors. The Braden Scale was initially tested for reliability and validity and these results were published in Nursing Research in 1987. A larger multi-site study was conducted to determine the reliability and validity of the tool in a variety of settings resulting in revisions in the recommendations for the critical cutoff score and the timing of assessment. Results were published in Nursing Research in 1998. A follow-up report in Nursing Research in 2002 demonstrated that the tool could be used in Black and White subjects with similar validity. This tool is in use on all continents and has been translated into many languages, including Japanese, Chinese, Korean, Indonesian, Italian, German, Portuguese, Polish, Arabic, Finnish, Norwegian, Icelandic, Flemish, Croatian, Dutch and French. Stage One Pressure Sore How to recognize: Skin is not broken but is red or discolored. The redness or change in color does not fade within 30 minutes after pressure is removed. Wound Definition Stage 1 pressure ulcers are non-blanchable erythermal intact skin, the heralding lesion of skin ulceration. In individuals with darker skin, discoloration of the skin, warmth, edema, indurations or hardness may also be indicators. The Braden Scale has been disseminated widely, translated into many languages, and is used to some extent around the world-wide. A recent systematic review by Pancorbo-Hildalgo and colleagues (2006) examined studies of various risk assessment tools published in Spanish, English, French and Portuguese and performed a meta-analysis to determine which of the many risk assessment tools available demonstrated the best reliability and validity. They compared the Braden Scale, Norton Scale, and the Waterlow Scale. They concluded that the Braden Scale had been tested in the largest number of studies, had demonstrated the best reliability and validity indicators in a variety of settings, and was a better predictor of pressure ulcers than nursing judgment. Visual Signs Pediatric patient example of Stage 1 pressure ulcer due to sheer force. Note the tell-tale redness and swelling of the epidermis. Circumferal flaring and use of ShearBan ® were incorporated to treat this patient Techniques For Pediatric Bracing: Pressure sores are also be referred to as pressure ulcers or decubitus ulcers. The damage from a pressure sore will range from slight discoloration of the skin (stage 1) to open sores that go all the way to the bone (severe). The affected area may feel warmer than the surrounding tissue. In light-skinned people, the discoloration may appear as dark purple or red. In darkerskinned people, the discoloration will appear darker than the surrounding tissue. Brace Modification: Plastic deformation Friction Mitigating Mediums: (ShearBan), soft shear gel sheeting or pressure relief padding Device Modification: Skeletal alignment, joint positional nuetrality A pressure sore is an injury to the skin and the tissue under it. A pressure sore develops when the blood supplying the tissue with oxygen and nutrients is cut off, and the tissue no longer receiving oxygen and nutrients dies. The oxygen and nutrients are essential to maintain healthy tissue. Sitting in the same position for a prolonged period of time can start the process of tissue breakdown. Anatomical Structural Support R eprinted by P erm ission Even pediatric patients are at risk for pressure sores. Children are active and may not pay attention to a developing sore especially if they have neurological deficits. Therefore it is essential to check the skin consistently for any pressure areas. Pediatric patients are at risk because of rapid growth and activity levels. Children may not even be aware of the level of potential damage the skin is in. Using an assessment tool such as the Braden scale when a patient is fit with a device can prove beneficial to both practitioners and parents. The results of the prediction can help develop a solid and effective plan of care that will both protect the patient and the practitioner. The Braden Scale for Predicting Pressure Sore Risk I nstructions: Use the Braden Scale to asses the patient's level of risk for development of pressure ulcers. The evaluation is based on six indicators: sensory perception, moisture, activity, mobility, nutrition, and friction or shear. Scoring: R eprinted by P erm ission The Braden Scale is a summated rating scale made up of six subscales scored from 1-3 or 4, for total sores that range 6-23. A lower Braden Scale Score indicates a lower level of functioning and, therefore, a higher level of risk for pressure ulcer development. A score of 19 or higher, for instance, would indicate that the patient is at low risk, with no need for treatment at the time. The assessment can also be used to evaluate the course of a particular treatment. Pressure Mitigating Mediums: (Moleskin), porous foams with adhesive backing Works Cited Johnson, & V Fay. (2004). HOW TO IDENTIFY AND PREVENT PRESSURE ULCERS. The Gerontologist: PROGRAM ABSTRACTS: 57th Annual Scientific Meeting..., 44(1), 70. Retrieved February 7, 2011, from ProQuest Medical Library. (Document ID: 920577101). Stopping pressure ulcers-Before they start. (2004, May). Nursing Homes, 53(5), 30-38. Retrieved February 7, 2011, from ABI/INFORM Global. (Document ID: 649424751). David R Thomas. (2001). Issues and dilemmas in the prevention and treatment of pressure ulcers: A review. The Journals of Gerontology: Series A Biological sciences and medical sciences, 56A(6), M32840. Retrieved February 7, 2011, from ProQuest Medical Library. (Document ID: 74000289). Susan Hook. (1998). Guidelines to help manage pressure ulcers. Australian Nursing Journal, 6(6), 27. Retrieved February 7, 2011, from ProQuest Medical Library. (Document ID: 36781691). Cathy Thomas Hess. (1998, July). Preventing skin breakdown. Nursing, 28(7), 28-9. Retrieved February 7, 2011, from ProQuest Medical Library. (Document ID: 31776535). Gates, Judy L. (1996). TQM: Pressure ulcer prevention. Nursing Management, 27(4), 48E. Retrieved February 7, 2011, from ABI/INFORM Global. (Document ID: 9602622). Carlson, M. (2009). The role of friction management in keeping our patients walking in comfort. Retrieved from http://www.tamarackhti.com/friction_management/shearban.asp Braden, B (1998). The braden scale. Retrieved from http://www.bradenscale.com/ Hanson, D., Langemo, D. K., Anderson, J., Thompson, P., & Hunter, S. (2010). Advances in Skin & Wound Care, 23(1), 21-24.doi:10.1097/01.ASW.0000363489.38996.13