PURPOSE:
advertisement

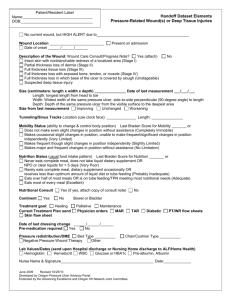
University of Miami Hospital SPONSORED BY: NURSING CHAPTER: PROVISION OF CARE I. POLICY AND PROCEDURE Subject: WOUND CARE POLICY No. Page 1 of 3 Original Date: October 1980 Revised Date(s): May 2009 Review Date(s): May 2011 SCOPE All direct care nursing staff II. PURPOSE Each patient will be assessed and documented on upon admission, at every shift, and upon discharge for potential and actual impaired skin integrity. All patients with community-acquired and /or nosocomial wounds will have the wound(s) isolated and photographed to establish a baseline measure of the appearance and location of the wound, and to document the progression of the wound. Photographs of all skin alterations will be taken on admission, every Wednesday, upon change in appearance, transfer to secondary care unit and on day of discharge. Patients considered "at risk for impaired skin integrity" will have a plan of care initiated that addresses preventative measures. All pressure ulcers, both community-acquired and nosocomial will be managed utilizing the principles of moist wound healing. An incident report must be filed for all community-acquired pressure ulcers on admission. All communityacquired pressure ulcers stage III must be reported via incident reporting system and escalated to Nursing Administration for reporting to abuse hotline. An incident report must be filed for all hospital-acquired pressure ulcers upon discovery. III. PROCEDURE Assessment: 1. The Braden Risk Assessment scale is a scientific tool that helps to identify patients at risk for pressure ulcer development. It includes 6 categories: Sensory Perception, Moisture, Activity, Mobility, Nutrition and Friction/Shear. Based upon assessment of the patient, he/she is assigned a subscale number in each category. The subscale numbers are added up to obtain the final Braden Risk Assessment score. The maximum score is 23; the minimum score is 11. Any patient with a score of 16 or less is considered to be at risk for pressure ulcer development. 2. Risk Scores: >23 = No Risk 17 - 23 = Low Risk 12 - 16 = Moderate Risk 0 - 11 = High Risk 3. Each patient will have a Braden Assessment score documented in meditech every 12 hours. 4. The "impaired skin integrity" plan of care will be initiated on all patients with Braden Risk Scores of 16, or less as they are at risk for pressure ulcer development. University of Miami Hospital SPONSORED BY: NURSING CHAPTER: PROVISION OF CARE POLICY AND PROCEDURE Subject: WOUND CARE POLICY No. Page 2 of 3 Original Date: October 1980 Revised Date(s): May 2009 Review Date(s): May 2011 5. Wound will be measured on admission, every Wednesday, upon change in appearance, transfer to secondary care unit and on day of discharge using the clock method. 6. Nurse will request to dietitian consult for Braden score of 16 or less and will follow-up with Medical Doctor for Dietitian recommendation. Prevention: 1. Perform skin assessment on admission, every shift, and at time of discharge. 2. If a patient is assessed with decubiti/wound, initiate Wound Flow Sheet at bedside and document every shift. 3. Perform Braden Risk Assessment upon admission and on every shift. 4. If patient has a Braden score less than 16 or is assessed with decubiti/wound, initiate the following: a) Assess for Nutritional Deficits and consult Dietitian for complete nutritional assessment and recommendations. b) Assess for incontinence, moisture problems, if present, and then protect the skin from fecal, urine, or wound drainage, as follows: Bathe with body wash; avoid hot water, soap, and excessive friction. Apply skin prep barrier and moisture barrier ointment to intact skin. If excoriation is present, apply an extra protective zinc based cream (sensicare, EPC cream). c) Apply moisturizing lotion to dry skin areas. d) Avoid diapers. e) Request appropriate specialty bed. Do not use additional padding on specialty beds. 5. Assess mobility and activity deficits and sensory perceptions. 6. Protect skin from effects of pressure/shear if patient is bed-bound, chair bound, or unable to reposition self and initiate the following as applicable: a) Turn patient every two (2) hours and document time along with position: R = Right B = Back L = Left P = Prone University of Miami Hospital SPONSORED BY: NURSING CHAPTER: PROVISION OF CARE POLICY AND PROCEDURE Subject: WOUND CARE POLICY No. Page 3 of 3 Original Date: October 1980 Revised Date(s): May 2009 Review Date(s): May 2011 S = Self b) Position in a 30-degree side/lying position. c) Provide pillows or foam wedges to keep bony prominences from direct contact with each other. d) Avoid positioning directly on trochanters when using the side/lying position. e) Avoid massages over bony prominences. f) Use pull sheet to move patient up in the bed. g) Float heels off of bed by placing a pillow longitudinally under calf at all times. h) Patients in intensive care areas will have preventive sacral border dressing place on patient with Braden Score of 16 or less.