Medicare Fees and the Volume of Physicians’ Services by Jack Hadley, Jim Reschovsky,
advertisement

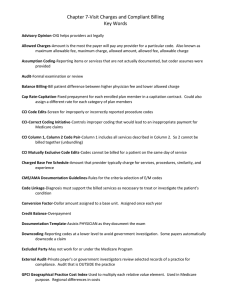
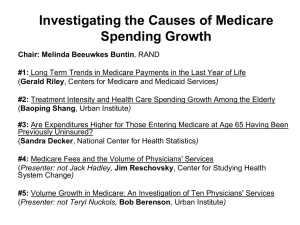
Medicare Fees and the Volume of Physicians’ Services by Jack Hadley, Jim Reschovsky, Catherine Corey, and Stephen Zuckerman Academy Health June 28, 2009 Study Questions 1. Do physicians provide more or fewer services to Medicare patients in response to a fee reduction? 2. Is the magnitude and/or direction of the response the same for all services? 3. Do physicians’ financial incentives in their practice influence the volume of services provided? 4. What are the implications for Medicare’s physician payment system? • Changes to the SGR • Volume offset assumptions Study Design Estimate physicians provision of specific services to Medicare patients as function of Medicare fee differences (+ other factors) We use exogenous geographic and over-time payment variations to measure differences in fees Data: • 2000-01 and 2004-05 CTS Physician Survey (N=13,707) • Linked with 2000 & 2005 Medicare claims of their FFS pts. Estimate 2-part models: • Probability of providing service • Volume of service provided, given any Calculation of Medicare Fee Differences We measure slope of MC curve for physicians providing specific services to Medicare patients Actual payments do not perfectly correspond to payment neutrality, as envisioned under RBRVS due to data limitations and policy decisions. Key measure is “Medicare fee difference” (MFD): • MFDijt = Paymtijt- Paymtijt* • Where: Paymtijt = actual Medicare payment Paymtijt* = payment based on closer approx. of pure RBRVS-based payment Payment Formula Adjustments To Reflect RBRVS Ideal More Accurately (Paymtijt* ) Greater geographic detail in calculating GPCIs: • Counties/metro areas rather than larger Medicare payment areas More accurate Practice Expense RVU assignment in 2000 Eliminated “other policy goals” aspects of MFS • ¼ to full work GPCI adjustment • Work GPCI floor • Medicare incentive program bonus payments Accounted for decline in real fees, 2000-2005 • Annual updates < input price increases (MEI) Figure 1. Physician Supply in a multi-market model Price Pprv MR MC AC B Pmcr-hi C Pmcr Pmcr-lo E A D Dprv = AR Qp-hiQpQp-lo Qlo Qtot Qhi Quantity of service provided Key Independent Variables (hypothesized sign) Medicare Fee Difference (+) Physician’s compensation incentives (+) • strong/moderate (e.g., owners) vs. weak (e.g., straight salary with no bonuses), etc.) Generic cross-price variables (?) Demand-shift variables (+) • Whether the practice accepts all/most new private patients • Whether the practice treats Medicaid patients • Percentage of Medicare patients with supplementary insurance • Perception of a very competitive market environment Also, physician specialty and other characteristics, site & time dummies Supply response to 10% reduction in fees a MFD coefficient statistically significant (p≤.10) in prob . of any provision equation; coefficient statistically significant (p≤.10) in the conditional volume equation. b MFD Financial Incentives: Simulated Impact on Volume if all Physicians on Fixed Salaries Service CPT code/ Test % Change in Volume Office Visits 99213 -26a 99214 -42a 99232 -42a 99233 -44a 99243 -13b 99244 -28b EKG -26a Echo -7 Hospital Visits Consultations Diagnostic Tests a Financial incentive coefficient significant in both equations; b Financial incentive variable significant only in first equation (probability of any provision). Policy Implications 1: Medicare Fee Schedule Fee schedule can be used to control costs • No evidence of volume offset response Uniform fee updates (SGR) distort practice patterns • Volume response differs across services Large payment areas distort practice patterns • Create unintended differences between actual fee and ideal RBRVS-based fee Need better data on underlying costs if goal is to maintain incentive neutrality Policy Implications 2: Move Away From Goal of Payment Neutrality Results imply altering fees in response to value of service: • Pay more for services that should be encouraged • Pay less for services thought to be ineffective Target services with rapid volume growth not explained by new technology • For more detailed cost assessment to adjust RVUs • For comparative effectiveness review Better yet, move away from FFS as payment model • Capitation, bundling, episode-based payment, etc. So Why Has Service Volume Grown While Real Fees Fell? Many fees still too high • Costs may be falling faster than fees Physicians’ profit-seeking behavior manifested through new practice arrangements, • For instance, greater capture of profits through equipment/facility ownership (e.g., imaging) Medicare does not exist in a vacuum • Utilization controls weaker in Medicare than commercial plans • Greater patient cost sharing in private insurance, e.g., HSAs and high-deductible plans • Increasing uninsurance