The Incidence of Medicare Payment Reduction: Evidence from the BBA of 97
advertisement
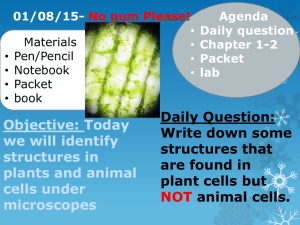
The Incidence of Medicare Payment Reduction: Evidence from the BBA of 97 Vivian Y. Wu University of Southern California AcademyHealth Annual Research Meeting, June 5, 2007 Responses to Medicare Payment Cuts 1. Charge private payer higher prices 2. Improve efficiency: shorter length of stay, less cares, …. etc, without hurting quality 3. Lower quality of care Research question Who bears the burden of 1997 BBA Medicare reimbursement cuts? Source: Dobson, A. et al., Health Affairs, Vol 25(1), 22-33 Prior Research 1980’s: mixed Early 1990’s: cost-shifting diminishing Around BBA 97: – Bernard, 2000 studied cross-subsidization between 1994-1998, elasticity was -0.5. – Zwanziger and Bamezai, 2006, found cost-shifting between 1993-2001 in CA was -0.17. Research Questions Central questions: – Do and can hospitals raise prices to private payers? – Does the behavior differ by ownership type? – Does market environment (ownership composition and managed care) have any impact on this behavior? Method Main Model: – Long-difference model at hospital level: Δ private price = Δ Medicare loss + control Method Key identifying variable: BBA “bite” variable 1.12 1.1 1.08 Market basket increase 1.06 1.04 1.02 1 0.98 0.96 0.94 Bite BBA reduction 1996 1997 1998 1999 2000 Method Dependent variable: – Private “price”: Private revenue / private discharges Private revenue / private days – Private LOS Method: Formal Model P(i, t, t-1) = i + Bite(i, t, t-1) + Bite(i, t, t-1) * ownership(i, t-1) + δ Bite(i, t, t-1) * HMO IV(i, t-1) + η Bite(i, t, t-1) * FP Share(i, t-1) + λ X(i, t, t-1) + X(i, t-1) + (i, t) Method Key independent variable: – Ownership type: Teaching, NFP, Public – FP market effect: % FP discharges in MSA – HMO effect: Instrument for HMO penetration (% in large firms, % white collar) Other controls: – Δ case mix, size (beds), SNF, HH, and market dummies (HRR) Results Δ Private Rev per Private Admission Δ Private Rev per Private Day Δ Private LOS -.76** [.14] -.53** [.12] -.0008** [.00008] SNF Bite .11 [.10] -.01 [.02] -.00001 [.00008] HH Bite .03 [.04] -.0003 [.009] .000007 [.00003] Δ case mix 482 [556] 44 [124] .29 [.41] Teach 198 [228] -28 [47] .18 [.16] -381** [150] -36 [33] -.05 [.11] Public -154 [188] -12 [41] -.13 [.14] HMO IV 2.69 [6.31] 0.91 [1.34] -.01** [.0005] IP Bite NFP Results Δ Private Rev per Private Admission Δ Private Rev per Private Admission IP Bite -1.06 [.25] -.36* [.19] SNF Bite -.10 [.10] -.09 [.10] HH Bite .03 [.04] .03 [.04] Δ case mix 486 [557] 413 [556] HMO IV -2.45 [7.39] 2.73 [6.31] FP Share 1.70 [5.03] 10.12* [5.82] Bite * HMO IV .008 [.006] -- Bite * FP share -- -.015** [.005] Key Findings Overall cost-shifting: Yes, 76%. Ownership: not by individual status Market effect: – ownership composition: Yes, More FP enables more cost-shifting – HMO penetration (IV): No effect Interpretations Large degree of cost-shifting comes from higher prices. -> managed care may not be effective in price bargaining in late 1990’s. Price increases more when there’s more FP in the market -> there is NFP-FP difference -> cost-shifting depends on some joint cost/quality function, which is determined by market composition Policy Implications The majority of “savings” from Medicare BBA cuts are financed through a hidden “tax” on privately insured. Injecting “competition” (through managed care) may not prevent hospital cost-shifting