Intensity of Imaging for Low Back Pain in Elderly Patients

Intensity of Imaging for
Low Back Pain in
Elderly Patients
HH Pham, MD, MPH, D Schrag, MD, MPH
C Corey, MS, J Reschovsky, PhD
HR Rubin, MD, PhD, BE Landon, MD, MBA
AcademyHealth Annual Meeting
June 2007
Background
Medicare spending on imaging services has increased dramatically since 2000 with unclear clinical benefits for beneficiaries
Guidelines allow discretion for imaging of elderly patients with acute low back pain
Little representative data on non-clinical factors associated with intensity of imaging
Research questions
What physician, practice, market, and nonclinical patient factors are associated with more intensive imaging for acute low back pain?
Does the economic environment in which physicians practice influence discretionary use of imaging?
Data sources (1)
2000-2001 Community Tracking Study Physician Survey
•
•
•
•
Nationally representative, clustered in 60 communities
Non-federal, completed training, 20+ hrs of clinical care/week
12,406 respondents, ~50% PCPs
59% response rate
Questions
• Specialty, board certification, FMG status
•
•
•
•
•
Practice type, revenue sources (Medicaid, Medicare), capitation
Ability to obtain specialist and imaging referrals
Overall effect of financial incentives (increase/decrease services)
Compensation based on quality, profiling, patient satisfaction
Practice ownership
Data sources (2)
Complete 2000-2002 Medicare claims for 1.09 million beneficiaries seen by CTS physicians in year 2000
Geographic data from Area Resources File on number of patient care radiologists per capita, household income, and education levels
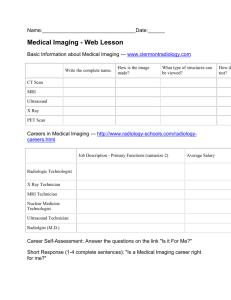
Design and Analysis
Back pain diagnosis identified for year 2001
Followed for 6 months after back pain diagnosis
Modeled “intensity” of imaging
• never imaged imaged 29 -180 days imaged within 28 days
• “Intensity” measured for:
(a) any imaging modality; and (b) only CT/MRI
Excluded patients diagnosed by a radiologist
Adjusted for comorbidities during year 2000, physician, practice, and area factors (site fixed effects)
Repeated analyses, excluding patients with visits to other physicians between diagnosis and imaging dates
Study population
63,075 (15%) patients of 318,148 linked to a CTS PCP and had a diagnosis of acute low back pain in 2001
24,515 (39%) meeting clinical inclusion criteria (no potential indications for imaging 6 months prior to LBP diagnosis or between diagnosis and imaging dates
21,992 (89%) meeting inclusion criteria and not diagnosed by a radiologist
5,964 (28%) imaged within 28 days
5,330 (90%) by XR
725 (12%) by CT/MRI
1,017 (4%) imaged between
29-180 days
734 (73%) by XR
314 (31%) by CT/MRI
15,011 (67%) never imaged
Clinical exclusions
Modified NCQA’s measure of inappropriate imaging for acute LBP
Cancers*
Neurologic deficits*
Trauma,* falls, injury
Infections – endocarditis, osteomyelitis, TB, etc.
IV drug use*
Anemia – not hereditary, Fe deficiency, or blood loss
Constitutional symptoms – weight loss, fever, night sweats, fatigue/malaise, loss of appetite
Care relationships between acute LBP patients and their plurality PCP
63 (47-80) Median (IQR) % of E&M visits with PCP
Had a visit with their CTS PCP within 6 months of LBP diagnosis
Diagnosed by their CTS PCP
Diagnosed in their CTS PCP’s practice
Diagnosed by any PCP
Specialties of other diagnosing clinicians
(outside of their CTS PCP’s practice)
Orthopedic surgeon
Chiropractor
81%
52%
60%
62%
9%
15%
Site of imaging studies performed within 28 days of diagnosis
Modality
Any
X-Ray
CT or MRI
Total imaged
N
6,981
6,064
1,039
Patients imaged in
PCP’s practice
N (%)
2,439 (37.5)
2,192 (38.9)
280 (27.1)
Timing of imaging after LBP diagnosis
Imaging procedure
Any modality
CT
MRI
Patients, N
Number of days between diagnosis and imaging,
Median (IQR)
6,981
165
879
0 (0-7)
9 (3-35)
13 (4-36)
Predictors of intensity of imaging
Patient factors and radiologist supply
Characteristic
Female
Medicaid eligible
Race (vs. white)
Black
Other
Radiologists/1000 (vs. lowest quartile)
Highest quartile
Any modality
Adjusted OR (95% CI)
1.01 (0.92-1.11)
0.81 (0.70-0.94)*
CT or MRI
Adjusted OR (95% CI)
0.81 (0.67-0.96)*
0.94 (0.71-1.25)
0.83 (0.77-0.96)*
0.95 (0.71-1.26)
1.10 (0.97-1.25)
0.67 (0.46-0.99)*
0.91 (0.58-1.42)
1.31 (1.02-1.69)*
No effect for median household income in the patient zip code; % adults with
12+ yrs of education in the county; or Klabunde or Charlson scores
Predictors of intensity of imaging
Physician factors
Characteristic
FP/GP specialty (vs. IM)
Effect of incentives
(vs. increase services)
To reduce services
No effect on services
Any modality
Adjusted OR (95% CI)
CT or MRI
Adjusted OR (95% CI)
0.95 (0.87-1.03)
0.83 (0.68-1.01)
1.03 (0.94-1.12)
0.83 (0.67-1.02)
0.73 (0.51-1.00)*
1.00 (0.80-1.25)
No effect for years in practice; board certification; IMG status; compensation based on productivity, quality, profiling or patient satisfaction measures , or practice ownership
Predictors of intensity of imaging
Practice factors
Characteristic
Any modality
Adjusted OR (95% CI)
CT or MRI
Adjusted OR (95% CI)
% Revenue from capitation (vs. none)
1-10%
11-25%
>25%
1.05 (0.94-1.17)
0.98 (0.85-1.13)
0.94 (0.79-1.12)
0.84 (0.68-1.03)
0.74 (0.54-1.00)*
0.67 (0.50-0.90)**
Practice type (vs. solo/2)
Small group (3-10)
Medium group (11-50)
1.19 (1.03-1.37)*
1.49 (1.21-1.84)***
1.10 (0.79-1.52)
0.94 (0.58-1.50)
Large group (>50) 1.22 (1.00-1.49)* 1.29 (0.85-1.96)
Medical school 0.84 (0.62-1.14) 0.64 (0.29-1.43)
No consistent effect for revenue from managed care, Medicare, or Medicaid
Limitations
No certainty regarding appropriateness of imaging
• Not benchmarking – only comparing relative performance
• Unlikely systematic under-coding of exclusions by physician or practice characteristics, or by white patient race and higher SES
• Uncertainty is comparable to claims-based measures of underuse
Lack data on presence of imaging equipment in practices
Cannot identify physician(s) responsible for referrals
•
• For imaging or to specialists
But consistent relationships between characteristics of the CTS
PCP and intensity of imaging
Conclusions
Substantial minority of elderly patients with uncomplicated
LBP are imaged early, often in their physician’s practice
• Most cases of rapid imaging use XR’s, not CT/MRI
Overall financial incentives matter, but no association with specific types of performance-based compensation
Subgroups of patients who tend to receive fewer services may sometimes benefit
Incentives to increase or decrease services may have mixed effects on quality that may go undetected if the majority of performance metrics reflect underuse
Geographic variation in percent of patients imaged within 28 days
Before exclusions
After clinical exclusions
Any Modality
After clinical exclusions
CT/MRI
CTS Market Unadjusted % Unadjusted % Adjusted % Unadjusted % Adjusted %
Seattle 22.6
20.7
29.2
2.6
4.7
Phoenix
Miami
24.6
34.0
23.9
26.3
28.9
21.5
2.9
5.9
4.6
3.5
Newark
Cleveland
Indianapolis
Lansing
Greenville
Little Rock
Orange Cty
Boston
Syracuse
32.3
29.7
29.5
27.3
30.0
29.0
28.1
29.5
31.6
27.4
27.5
28.5
28.5
29.8
30.4
30.9
31.8
33.3
27.5
29.3
28.3
28.9
28.4
29.3
26.6
29.4
30.5
7.6
4.5
5.8
3.3
4.6
6.6
5.0
11.1
4.9
4.9
5.0
4.9
5.1
4.6
5.2
4.7
5.8
5.3