RACE, INCOME, AND Introduction OPERATIVE TIME
advertisement

RACE, INCOME, AND
OPERATIVE TIME
Jeffrey H. Silber, M.D., Ph.D.
Paul R. Rosenbaum, Ph.D.
Xuemei Zhang, M.S.
Orit Even-Shoshan, M.S.
The Center for Outcomes Research, The
Children’s Hospital of Philadelphia
The Department of Pediatrics, Anesthesiology
and Critical Care Medicine, PENN
The Department of Statistics, The Wharton
School, PENN
The Leonard Davis Institute of Health Economics
Measuring Operative Time
• Until now, studies analyzing operative time
in the Medicare population have been
limited to single (or very few) institutions.
• Operative time is usually defined as:
– Surgical Time: Incision to closure
– Anesthesia Time: Induction to Recovery Room
Goals of this Talk
• To examine the accuracy of using Anesthesia
Time Units from Medicare bills to estimate
operative time
• To examine models that predict procedure
length based on:
– Patient comorbidities
– Race
– Income
• To explore the relationship between race and
operative time at individual hospitals
• To discuss the implications of disparities in
operative time
Introduction
• Operative time is a common measure of
surgical quality
– Longer procedures are associated with higher
infection rates
– Longer procedures are associated with
physicians-in-training
Measuring Operative Time in
Medicare Patients
• In 1994, billing for Anesthetist and
anesthesiologist services changed to a
“by the minute” system
• Anesthetist bills (anesthesiologists, nurse
anesthetists) from Medicare have never
been utilized to examine procedure time
on a large scale
• Race and Income have not been studied
with respect to procedure time
Data
• Medicare Claims on the 20 most common
General Surgical procedures and the 20
most common Orthopedic procedures in
Pennsylvania in 1995 and 1996, N = 77,638
• Chart Abstractions on a subset of 1931
Pennsylvania General Surgical and
Orthopedic patients as part of the Surgical
Outcomes Study
1
The Anesthesia Claim
Time Abstraction
• The Anesthesia Claim consists of two parts:
– Base Units
– Time Units
• Time units are in 15 minute intervals. The
first digit of the time unit is a decimal tenths
digit
– For example: “25” for units = 15 x 25/10
minutes or 37.5 minutes
• We chose the single longest anesthesia bill
associated with the same day as the
principle procedure
• We defined four specific times for
abstraction on 1931 charts in the SOS
study:
– Start induction
– Start incision
– Closure
– To recovery room or ICU (if going directly to
ICU)
Bill Time - Chart Time. N = 1931 patients from the Surgical Outcomes Study
Chart Time as a Function of Claim
Time, N = 1931
Variables
Int.
Slope
P
R2
Median
Absolute
Residual
(minute)
I: Unadjusted
m-Estimation
-1.21
0.97
.0001
.89
5.49
N/A
II: Comorbidities,
Procedures
and Hospitals
2.47
0.98
.0001
.89
5.37
<.0001
P
(Wald)
Shapiro-Wilk Test P < 0.0001
The independent variable is anesthesia claim minutes, and
the dependent variable is anesthesia chart minutes.
N = 1931, ρ = 0.94.
Estimated Anesthesia Time (Minutes) for Each General Surgical
Principle Procedure
N
25th %ile
Median
75TH %ile
422
210
260
320
Anterior Rectal Resection
685
165
251
255
Left Hemicolectomy
1307
155
195
242
Part Lg Bowel Excis Nec
507
150
191
251
Sigmoidectomy
2922
140
176
221
Lg Bowel Stoma Closure
326
116
164
221
Part Sm Bowel Resection
1253
120
155
209
Right Hemicolectomy
34350
120
155
195
Unilat Thyroid Lobectomy
370
120
135
176
Cholecystectomy-Open
3883
105
135
176
Peritoneal Adhesiolysis
1268
94
125
173
Procedure
Abd-Perineal Rect Resect
These times include principle procedures that were also accompanied with other
secondary procedures billed on the same day.
2
Estimated Anesthesia Time (minutes) for Each General Surgical
Principle Procedure (when only one procedure performed)
Estimated Anesthesia Time (Minutes) for Each Orthopedic
Principle Procedure
Procedure
N
25th %ile
Median
75TH %ile
N
25th %ile
Median
75TH %ile
Abd-Perineal Rect Resect
84
206
240
285
Lumbar/Lum-sac Fus Post
273
236
299
380
Anterior Rectal Resection
222
146
176
218
Other Cervical Fus Ant
152
182
240
343
Left Hemicolectomy
262
143
180
221
Revise Hip Replacement
971
180
234
311
Part Lg Bowel Excis Nec
77
131
158
206
Spinal Canal Explor
3166
138
180
240
Sigmoidectomy
678
125
155
195
Revise Knee Replacement
1110
143
180
230
Lg Bowel Stoma Closure
159
101
125
180
Excision Intervert Disc
2565
131
165
221
Part Sm Bowel Resection
112
105
131
170
Total Hip Replacement
6215
140
165
197
Right Hemicolectomy
940
110
135
170
Total Knee Replacement
12718
131
150
180
Unilat Thyroid Lobectomy
286
108
135
167
Open Red-Int Fix Hum
690
107
142
191
Cholecystectomy-Open
978
90
116
146
Partial Hip Replacement
4735
105
129
155
Peritoneal Adhesiolysis
316
80
101
125
Shoulder Arthroplasty
909
105
124
158
These times only include principle procedures that did not have other secondary
procedures billed on the same day.
Procedure
These times include principle procedures that were also accompanied with other
secondary procedures billed on the same day.
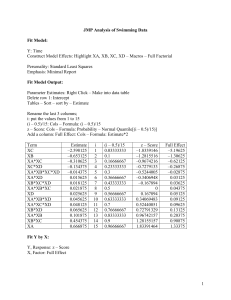
Estimating Anesthesia Time (Y = Mins. from bill)
Estimated Anesthesia Time (minutes) for Each Orthopedic
Principle Procedure (when only one procedure performed)
Parameter
Minutes
P-value
Multiple procedures
18.3
.0001
Admit from ER
.10
.90
Procedure
N
25th %ile
Median
75TH %ile
Lumbar/Lum-sac Fus Post
41
200
240
294
Transfer In
6.6
.0003
Other Cervical Fus Ant
30
155
195
245
Hx Coagulopathy
5.0
.0001
Revise Hip Replacement
639
180
225
300
Spinal Canal Explor
1478
131
170
218
Hx Diabetes
2.5
.0001
Revise Knee Replacement
792
140
179
227
Hx Paraplegia
4.7
.0004
Excision Intervert Disc
1529
122
155
196
Black Race Vs White
5.2
.0001
Total Hip Replacement
4770
140
165
195
Severity Score 1
1.5
.04
Total Knee Replacement
10551
131
150
180
Severity Score 2
.40
.59
Open Red-Int Fix Hum
459
101
131
170
Partial Hip Replacement
4102
105
125
150
Severity Score 3 & 4
2.2
.03
Shoulder Arthroplasty
129
101
131
176
Severity Score 0
Ref
N/A
N=77,638 patients, controlling for 39 (=n-1) surgical procedures and 182 (=n-1)
hospitals and 34 patient covariates of which 8 are displayed above. The model
was fit using m-estimation, rank R2 of 40%.
These times only include principle procedures that did not have other secondary
procedures billed on the same day.
Race, Income, and Procedure Time
Race, Income, and Procedure Time
WL
(n = 9,324)
BM
(n = 513)
WM
(n = 25,060)
BH
(n = 547)
WH
(n = 27,473)
BL (n = 2002)
BL adjusted by
183 hosp.
29 (<.0001)
9 (<.0001)
15 (<.0001)
3 (0.159)
30 (<.0001)
7 (<.0001)
15 (<.0001)
8 (<.0001)
27 (<.0001)
8 (<.0001)
-2 (<.0001)
WL (n = 9,324)
WL adjusted by
183 hosp.
---
-14 <.0001)
-4 (.036)
1 (<.0001)
0 (.578)
-14 (<.0001)
-5 (.486)
-2 (<.0001)
1 (.069)
0 (.8939)
12 (<.0001)
BM (n = 513)
BM adjusted by
183 hosp.
14 (<.0001)
4 (.036)
0 (.8939)
5 (.052)
12 (<.0001)
4 (.014)
-15 (<.0001)
-3 (<.0001)
WM (n = 25,060)
WM adjusted by
183 hosp.
---
-15 (<.0001)
1 (.570)
-3 (<.0001)
1 (.126)
---
12 (<.0001)
BH (n = 547)
BH adjusted by
183 hosp.
---
12 (<.0001)
0 (.848)
WL
(n = 9,324)
BM
(n = 513)
WM
(n = 25,060)
BH
(n = 547)
WH
(n = 27,473)
BL (n = 2002)
29 (<.0001)
15 (<.0001)
30 (<.0001)
15 (<.0001)
27 (<.0001)
WL (n = 9,324)
---
-14 <.0001)
1 (<.0001)
-14 (<.0001)
14 (<.0001)
---
BM (n = 513)
WM (n = 25,060)
BH (n = 547)
---
---
3
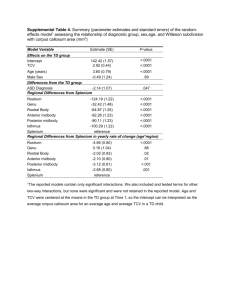
Adjusted Differences Between Black and White Procedure Times in
Pennsylvania Hospitals With the Largest Black Populations
Hospital
No.
Black
No.
White
Teaching Type
Excess Mins.
(b-w)
Policy Implications
P-Value
1
153
352
Major
3.3
.449
2
147
322
V Major
7.0
.115
3
130
326
V Major
0.8
.870
4
125
108
V Major
12.2
.039
5
118
1319
Major
14.3
.001
6
112
437
Major
12.1
.011
7
112
43
Major
-4.6
.562
8
111
1006
Not Teaching
4.0
.366
9
109
71
V Major
6.9
.308
10
107
505
Major
9.3
.050
11
105
178
V Major
15.9
.004
12
100
1007
V Major
-5.1
.274
The overall Wald test for equality was 0.029, suggesting there is variability in
disparity across hospitals. General Surgical and Orthopedic Procedures
Why might there be a disparity in
operative time inside a hospital?
Why do we care about 15 minutes?
• Reasons consistent with fairness
– Unobserved severity
– Admission from ER
– Emergency Surgery
• Reasons based on injustice
– Different Surgeon/Physician-in-Training for
less empowered
– Risk of Litigation
– Racism (Conscious or Unconscious)
Identifying the Provider: Who is
holding the retractor?
• In teaching hospitals it is not always clear
from the chart or the claim who is
performing surgery.
• Is the resident doing the dissection or
holding the retractor?
• Differential times between the resident and
the attending may help in identifying the
two providers.
For a typical procedure like Colectomy, which was described in Khuri et al. (Annals
Surgery 2001), we can estimate the relative speed of the resident and attending,
assuming the hospital location does not influence this time.
VA
Location
N
Complexit
y
% of
Cases by
Residents
Hours of
Surgery
Mean
Time
Combined
3.085
Teaching
8,038
3.00
93.64
3.17
NonTeach
1,201
2.95
1.42
2.54
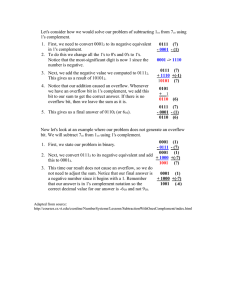
From this table we can solve for the time a resident takes to perform the
colectomy (TR) and the time an attending takes to perform the surgery (TA). We
have two equations and two unknowns:
(0.9346)TR + (0.0636)TA = 3.17
(0.0142)TR + (0.9808)TA = 2.52
Solving, we get TA = 2.523 and TR = 3.213 hours. This is very close to those in
table 8 above, as almost all the surgery in the teaching hospital was with
residents and almost all the surgery in the non-teaching hospital was with
attendings.
4
The Relative Risk of Getting a Resident in Black Versus White Patients
TB = TR * PB,R + TA * PB,A
From
Regression
Data
[TB − TW ]
PRB
=
+
1
PRW
( PRW ) [TR − TA ]
TW = TR * PW,R + TA * PW,A
Or, since PB,R + PB,A = 1and PW,R + PW,A = 1, we can write:
TB = TR * PB,R + TA * (1 - PB,R ) and
TW = TR * PW,R + TA * (1 - PW,R ).
Hence,
TB-TW = PB,R * [TR - TA] - PW,R*[TR - TA] and:
[TB - TW]/[TR-TA] = PB,R - PW,R Or:
From External
Data or
Matching
Studies
[TB - TW]/ [PW,R][TR-TA] = [PB,R / PW,R]-1 and finally:
1+ {[TB - TW] / {[PW,R][TR-TA]}} = [PB,R / PW,R]
Assuming:
Relative Risk of Obtaining a
Resident if a Black Patient Versus
a White Patient
TR-TA = 30 mins
TB – TW = 15 mins
Relative Risk for Blacks
7.0
6.0
5.0
4.0
3.0
2.0
1.0
0.0
0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1
Percent of Cases Performed by a
Resident if Patient is White
Advantages of using Procedure
Time as a Measure of Disparity
• Bills available for literally all procedures
performed in the OR for Medicare patients
• Procedure length is highly dependent on
the surgeon, not patient compliance
• Procedure length is less dependent on the
past history of the patient—insensitive to
unobserved severity
• Time is not game-able, especially since it
has not been used to measure disparity in
the past
Conclusions
Acknowledgements
• Procedure time can be well estimated with
Medicare claims data
• Procedure time is a function of race and
income and the specific hospital, after
adjustment for other patient factors
• There is a significant procedure length
racial disparity inside of hospitals
• Mechanisms for this procedure length
disparity need to be better understood
• This work was funded through a grant
from the Leonard Davis Institute of Health
Economics at PENN and supported in part
from AHRQ Grant Number HS-09460
5
Additional Slides for Potential
Questions
The End
TEACHING
N=480
Patients
Sometimes
NON-TEACHING
N=96 Surgeons
N=480
Patients
Sometimes
TEACHING
Sometimes
NON-TEACHING
P = 0.214
109 minutes
Sometimes
103 minutes
P = 0.657
P = 0.002
P = 0.393
P = 0.0001
N=480
Patients
ALWAYS
N=480
Patients
ALWAYS
ALWAYS
121 minutes
P = 0.002
ALWAYS
106 minutes
6