Development of the Medicare Patient Safety Monitoring System
advertisement

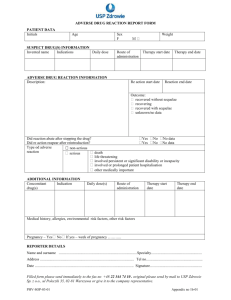
Development of the Medicare Patient Safety Monitoring System Susan L. Abend, MD, FACP David R. Hunt, MD, FACS Gaston Mbateng, Ph.D. Nancy Safer, RN, MSN Janet P. Tate, MPH Nancy R. Verzier, RN, MSN, CPHQ Background and Development Team • DHHS Patient Safety Task Force • CMS – David R. Hunt, MD, FACS • Qualidigm – Connecticut Quality Improvement Organization • Active Collaborators – Federal Agency Work Group • AHRQ, CDC, FDA, VA – Technical Expert Panel – Computer Science Corporation (Central Data Abstraction Center) Goal To determine the incidence of specific, clearly defined, hospital-acquired adverse events within the Medicare population Purpose • Baseline data for CMS national quality improvement initiatives – Surgical Care Improvement Project • Annual data to the National Healthcare Quality Report • A method for repeated assessment of events (tracking and trending) for safety improvement activities within healthcare organizations Design • Retrospective Cohort Study • 25,000- 40,000 randomly-selected discharges/year from the Hospital Payment Monitoring Program – Data obtained from medical charts and Medicare Part A claims database • HPMP cases – randomly selected cases from 50 states, D.C., Puerto Rico, U.S. Virgin Islands – sent to CDAC’s to check coding accuracy MPSMS Definition of Adverse Event “An unintended patient harm, injury, or loss more likely associated with an interaction with the health care delivery system than from an attendant disease process.” • Patient centered – Focuses on patient experience – Does not presume to assign severity • Detects an untoward outcome • Requires defined healthcare exposure • Not dependent on cause – Process malfunction (error, negligence) – Imperfect technology Measure Development Process • Event and exposure defined • Boolean algorithm developed to detect exposure-related event • Alpha test • Beta test • Clinical review • Production Measure Selection Criteria • Findable/Feasible • Adverse event(s) very likely to be associated with exposure • Common (burden on Medicare population) • Responsible for serious morbidity and mortality • Preventable Adverse Event Rates ’02 and ‘03 Medicare Inpatients Rate (%) + 95%CI Post-Operative Pneumonia 2.5 + 0.3 Post-Operative Venous Thromboemboli 0.6 + 0.1 Post-Operative Urinary Tract Infection 3.7 + 0.3 Knee Replacement Adverse Events 7.2 + 1.3 Hip Replacement Adverse Events 11.4 + 1.8 Adverse Event Rates ’02 and ‘03 Medicare Inpatients Rate (%) + 95% CI Ventilator Associated Pneumonia Hospital-Acquired Bloodstream Infection 11.9 + 1.8 0.30 + 0.05 CVC-Associated Bloodstream Infection 1.4 + 0.3 CVC-Associated Insertion Site Infection 2.6 + 0.4 CVC-Associated Mechanical Adverse Events 2.3 + 0.3 Average Length of Stay ’02, ‘03 Medicare Patients With Invasive Surgical Procedures 30 with event 25 no event DAYS 20 15 10 5 0 Post Op Pneumonia Error bars indicate 95% CI Post Op VTE Post Op UTI Inpatient Mortality Rate ’02, ‘03 Medicare Patients With Invasive Surgical Procedures 25 with event no event 20 % 15 10 5 0 Post Op Pneumonia Error bars indicate 95% CI Post Op VTE Post Op UTI Phase II Measures One Year of Data Pending • Postoperative Cardiac Events • Adverse Drug Events – Anticoagulant-related hemorrhagic events – Insulin/oral hypoglycemic agent-related hypoglycemic events – Antibiotic-associated C. Difficile infection • Pressure Ulcers Phase III Measures In Development • In- Hospital Falls • Angiography-Related Adverse Events – Contrast nephropathy – Adverse events related to femoral artery puncture • Urinary Tract Infections Associated with Bladder Catheterization Reliability Agreement Rate of Reported MPSMS Variables 100 90 dichotomous 80 categorical 70 %t 60 50 40 30 20 10 0 >=95% >=90% and < 95% >=80% and < 90% Kappa Statistic for Reported MPSMS Variables > 0.8 0.61 - 0.8 <= 0.6 15% 55% 30% Limitations • Validation – No true gold standard yet defined for determining sensitivity and specificity • Data source issues – Retrospective – Depends on consistent documentation of exposures and events in medical record • Events are relatively infrequent • Limited capability for risk adjustment Policy Implications • Complements reporting efforts – Able to detect denominator – No reporting bias • Complements indicators derived from administrative data alone – Potential for improved sensitivity – Richer database of variables Policy Implications cont’d • Standard definitions – trackable over time • Allows hospitals to use common, standard benchmarks • Potential for post-discharge surveillance of events • Usable in paper or electronic health records – Potential for concurrent or prospective use in error trapping or event avoidance. Summary • The MPSMS is a reliable tool for measuring adverse events in hospitalized patients • Can measure the outcome of errors, suboptimal systems and/or technologies • Uses standardized, patient-oriented definitions of adverse events • Development is transparent and consensus-driven – strong collaboration between public and private stakeholders Conclusion The MPSMS is a valuable tool for hospitals and health care organizations to use in making transformational changes to create a safe healthcare environment. This material was prepared by Qualidigm, the Medicare Quality Improvement Organization for Connecticut, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. Pub. # QUALCT-PSMS-200501