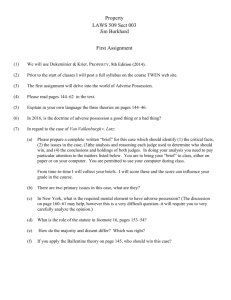
Background and Development Team Development of the Medicare Patient Safety Monitoring
advertisement

Background and Development Team Development of the Medicare Patient Safety Monitoring System • DHHS Patient Safety Task Force • CMS – David R. Hunt, MD, FACS • Qualidigm Susan L. Abend, MD, FACP David R. Hunt, MD, FACS Gaston Mbateng, Ph.D. Nancy Safer, RN, MSN Janet P. Tate, MPH Nancy R. Verzier, RN, MSN, CPHQ – Connecticut Quality Improvement Organization • Active Collaborators – Federal Agency Work Group • AHRQ, CDC, FDA, VA – Technical Expert Panel – Computer Science Corporation (Central Data Abstraction Center) Goal To determine the incidence of specific, clearly defined, hospitalhospital-acquired adverse events within the Medicare population Design • Retrospective Cohort Study • 25,000- 40,000 randomly-selected discharges/year from the Hospital Payment Monitoring Program – Data obtained from medical charts and Medicare Part A claims database • HPMP cases – randomly selected cases from 50 states, D.C., Puerto Rico, U.S. Virgin Islands – sent to CDAC’s to check coding accuracy Purpose • Baseline data for CMS national quality improvement initiatives – Surgical Care Improvement Project • Annual data to the National Healthcare Quality Report • A method for repeated assessment of events (tracking and trending) for safety improvement activities within healthcare organizations MPSMS Definition of Adverse Event “An unintended patient harm, injury, or loss more likely associated with an interaction with the health care delivery system than from an attendant disease process.” • Patient centered – Focuses on patient experience – Does not presume to assign severity • Detects an untoward outcome • Requires defined healthcare exposure • Not dependent on cause – Process malfunction (error, negligence) – Imperfect technology 1 Measure Selection Criteria Measure Development Process • Event and exposure defined • Boolean algorithm developed to detect exposure-related event • Alpha test • Beta test • Clinical review • Production • Findable/Feasible • Adverse event(s) event(s) very likely to be associated with exposure • Common (burden on Medicare population) • Responsible for serious morbidity and mortality • Preventable Adverse Event Rates Adverse Event Rates ’02 and ‘03 Medicare Inpatients ’02 and ‘03 Medicare Inpatients Rate (%) + 95%CI Rate (%) + 95% CI Post-Operative Pneumonia 2.5 + 0.3 Ventilator Associated Pneumonia Post-Operative Venous Thromboemboli 0.6 + 0.1 Hospital-Acquired Bloodstream Infection Post-Operative Urinary Tract Infection 3.7 + 0.3 CVC-Associated Bloodstream Infection 1.4 + 0.3 Knee Replacement Adverse Events 7.2 + 1.3 CVC-Associated Insertion Site Infection 2.6 + 0.4 CVC-Associated Mechanical Adverse Events 2.3 + 0.3 Hip Replacement Adverse Events 11.4 + 1.8 11.9 + 1.8 0.30 + 0.05 Average Length of Stay Inpatient Mortality Rate ’02, ‘03 Medicare Patients With Invasive Surgical Procedures ’02, ‘03 Medicare Patients With Invasive Surgical Procedures 30 25 with event with event 25 no event no event 20 15 % DAYS 20 15 10 10 5 5 0 0 Post Op Pneumonia Post Op VTE Post Op UTI Post Op Pneumonia Post Op VTE Post Op UTI Error bars indicate 95% CI Error bars indicate 95% CI 2 Phase III Measures Phase II Measures In Development One Year of Data Pending • In- Hospital Falls • Postoperative Cardiac Events • Angiography-Related Adverse Events • Adverse Drug Events – AnticoagulantAnticoagulant-related hemorrhagic events – Insulin/oral hypoglycemic agentagent-related hypoglycemic events – Antibioticassociated C. Difficile infection Antibiotic – Contrast nephropathy – Adverse events related to femoral artery puncture • Urinary Tract Infections Associated with Bladder Catheterization • Pressure Ulcers Reliability Agreement Rate of Reported MPSMS Variables Kappa Statistic for Reported MPSMS Variables 100 90 > 0.8 0.61 - 0.8 <= 0.6 15% dichotomous 80 categorical 70 %t 60 50 40 55% 30 30% 20 10 0 >=95% >=90%and < 95% >=80%and < 90% Limitations • Validation – No true gold standard yet defined for determining sensitivity and specificity • Data source issues – Retrospective – Depends on consistent documentation of exposures and events in medical record • Events are relatively infrequent • Limited capability for risk adjustment Policy Implications • Complements reporting efforts – Able to detect denominator – No reporting bias • Complements indicators derived from administrative data alone – Potential for improved sensitivity – Richer database of variables 3 Policy Implications cont’d • Standard definitions – trackable over time Summary • The MPSMS is a reliable tool for measuring adverse events in hospitalized patients • Allows hospitals to use common, standard benchmarks • Can measure the outcome of errors, suboptimal systems and/or technologies • Potential for post-discharge surveillance of events • Uses standardized, patient-oriented definitions of adverse events • Usable in paper or electronic health records • Development is transparent and consensus-driven – Potential for concurrent or prospective use in error trapping or event avoidance. – strong collaboration between public and private stakeholders Conclusion The MPSMS is a valuable tool for hospitals and health care organizations to use in making transformational changes to create a safe healthcare environment. This material was prepared by Qualidigm, the Medicare Quality Improvement Organization for Connecticut, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy. Pub. # QUALCT-PSMS-200501 4