Churning: Children’s Coverage Discontinuity and Its What we know about discontinuity in
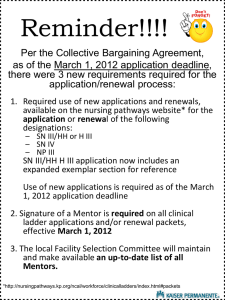
advertisement

What we know about discontinuity in children’s coverage • NY: half lost coverage in a year despite most remaining technically eligible (Lipson 2003) • 12 states: less than half timely renewed (Hill 2003) • 4 states: half lapsed at renewal but one-fourth back in 2 months (Dick 2002) • 7 states: two-thirds of disenrolled ineligible for SCHIP (but Medicaid?) (Riley 2002) • Kansas: procedural and computer problems often at fault (Allison 2003) Churning: Children’s Coverage Discontinuity and Its Consequences in Kentucky Julia F. Costich and Svetla Slavova College of Public Health University of Kentucky Kentucky Children’s Health Insurance Program (KCHIP) KCHIP Policy Changes • Medicaid expansion to 150% FPL • Look-alike to 200% FPL • Administered by Dept. for Medicaid Services • Eligibility determination by same agency as cash assistance, food stamps, etc. • Enrollment stable at ~50,000 children • Compare Medicaid at ~321,000 • 1998: Mail-in application, in-person renewal • 7/1/2000: Mail-in renewal with pre-populated form and self-declaration of income • 6/1/2001: Return to in-person interview for renewal • 7/1/2002: Mailed renewal reinstated; return to in-person interview for initial application • Confusion among caseworkers and families Percentage of All Children Enrolled in KCHIP or Medicaid, SFY 2003 Data source: Kentucky Dept. for Medicaid Services Fig. 1: KCHIP Enrollment May 2001-March 2004 56000 Under 30% Recertification policy changes 55000 30-39% 40-49% 54000 Campbell Premiums Boone Kenton 53000 50-59% Gallatin Pendleton Carrll Over 60% Bracken Grant Trimble Mason Owen Robertson Henry Fleming Nicholas Shelby Rowan Bourbon Anderson Bath Elliott Montgomery Menifee Clark Jessamine Webster Larue Mclean Ohio Livingston Ballard Warren Christian Barren Knox 45000 Mar-04 F eb-04 J an-04 Dec -03 Nov -03 O c t-03 Sep-03 Aug-03 J ul-03 J un-03 May-03 Apr-03 Mar-03 F eb-03 J an-03 Dec -02 Nov -02 O c t-02 Sep-02 Aug-02 J ul-02 J un-02 May-02 Apr-02 Mar-02 Bell F eb-02 Whitley J an-02 Mccreary Dec -01 Clinton Nov -01 Monroe Calloway Fulton O c t-01 Allen 46000 Sep-01 Simpson Harlan Wayne Aug-01 Cumberland J ul-01 Logan Letcher J un-01 Todd Leslie Russell May-01 Graves 47000 Clay Laurel Pulaski Adair Metcalfe Trigg Hickman Knott Perry Caldwell Lyon Marshall 48000 Pike Owsley Casey Green Mccracken Carlisle Jackson Rockcastle Taylor Hart Edmonson Floyd Breathitt Lincoln Grayson Butler Muhlenberg 49000 Magoffin Lee Marion Crittenden Hopkins Wolfe Estill Garrard Boyle Union Johnson Martin Madison Washington Hardin Morgan Powell Mercer Nelson Breckinridge 50000 Lawrence Fayette Woodford Spencer Bullitt Meade Hancock Daviess End of mail-in application 51000 Boyd Carter Scott Franklin Henderson Greenup Lewis Harrison Oldham Jefferson 52000 Prepared by: Julia F. Costich, College of Public Health 1 Problems with added eligibility office workload Fig. 2: Combined KCHIP and Children's Medicaid Enrollment, May 2001-March 2004 Source: Family Resource & Youth Service Center Staff Survey 380000 • • • • • • • 370000 360000 350000 340000 330000 320000 310000 Long waits in understaffed urban offices Refusal to provide scheduled appointments Overloaded phone system; unanswered voice mails Unexpected requests for additional documentation Inappropriate denial based on confusion Staff reporting suspect immigration status Failure or inability to accommodate working families’ schedules M ar-04 F eb-04 J an-04 D ec -03 N ov -03 O c t-03 Sep-03 Aug-03 J ul-03 J un-03 M ay -03 Apr-03 M ar-03 F eb-03 J an-03 D ec -02 N ov -02 O c t-02 Sep-02 Aug-02 J ul-02 J un-02 M ay -02 Apr-02 M ar-02 F eb-02 J an-02 D ec -01 N ov -01 O c t-01 Sep-01 Aug-01 J ul-01 J un-01 M ay -01 Churning effect • • • • • • • 46% did not renew on time New applications were 52% of total enrollment Yet total enrollment grew by only 4% Millions of wasted state dollars Risk of gaps in coverage Wide variation across the state Timely renewal highest in Medicaid expansion Data sources • Open records request to Medicaid for data by county, month and program – “Requires” staff to provide data • Data limitations – Not individual-level – “New” applications may be internal to system when renewal deadline is missed by staff • 3 categories – Number of children up for renewal – Number timely renewed – Number of new applications approved Methodology • Percentage of all children (Census data) enrolled in KCHIP or Medicaid – Critically important to include both because of frequent movement between programs – Failure to account for movement overstates churning • Percentage of children eligible for renewal in either program who renewed on time • New applications approved as percentage of total enrollment 2 Percentage of Children Enrolled and Percentage of Timely Renewals (R2 = .44) New Approvals as Percentage of Total and Percentage of Timely Renewals (R2 = .55) Methodology and statistical findings Discussion • SAS univariate regression analysis • F test found p < .0001 for relationships between – renewal and enrollment – new applications and non-renewal • R2 = .44 and .55 respectively • Low rate of timely renewal similar to other studies’ findings • Identified need for pre-termination contact, follow-up – Problem: hiring freezes, state budget deficit • Next steps: – Determine whether supportive environment of highrenewal counties can be replicated with outreach workers, volunteers – Advocate for more realistic federal budget allocations Limitations • Inability to track individual children • Considerable migration among programs • Eligibility determination office practice giving rise to spurious new applications • Possible delinking issues in information systems • Antiquated eligibility determination system may introduce errors 3