Child Health
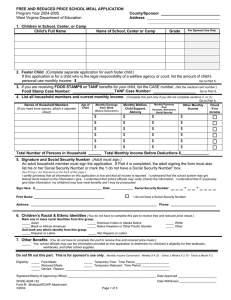
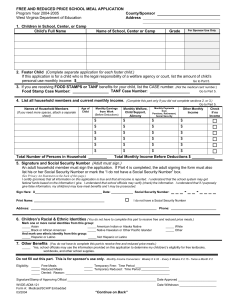
advertisement

Child Health Call for Papers Determinants of Access & Quality of Care Chair: Elizabeth Ozer, Ph.D., M.A. Implications for Policy, Delivery or Practice: These findings indicate the importance of children having an individual PCP, especially in Medicaid and managed care programs providing care to large numbers of children. Primary Funding Source: Ambulatory Pediatric Association • Ethnic Disparities in SCHIP: The Role of Acculturation Susan Haber, Sc.D., Susan Haber, Sc.D., Janet Mitchell, Ph.D., Sonja Hoover, M.P.P. Sunday, June 6 • 11:30 a.m.-1:00 p.m. • Pediatric Quality of Care is Associated with Primary Care Provider Type David Brousseau, M.D., M.S., Raymond Hoffmann, Ph.D., Jennifer Yauck, M.S., Glenn Flores, M.D., Ann Nattinger, M.D., M.P.H. Presented by: David Brousseau, M.D., M.S., Assistant Professor, Pediatrics, Medical College of Wisconsin, 9000 W Wisconsin Avenue, Milwaukee, WI 53226; Tel: 414.266.2625; Fax: 414.266.2635; E-mail: dbrousse@mail.mcw.edu Research Objective: It is not known whether parents who identify their child's primary care provider (PCP) as an individual receive higher quality care than those who view the child s PCP as a location/facility. Our objective was to compare the quality of care received by children when the identified PCP is an individual vs. a facility. Study Design: Cross-sectional analysis of 2000 Medical Expenditure Panel Survey Population Studied: We analyzed data from the 2000 Medical Expenditure Panel Survey, weighted to give national population based estimates. Only children with an identified PCP were included. The identified PCP was classified as an individual or facility; those identifying the PCP as the emergency department were excluded. Quality of care was assessed using parent reports for: 1) getting care without long waits [routine care, sick care, phone help and brief wait times with appointments], 2) getting needed care [referrals and receiving care doctor believed necessary], and 3) doctor communication [quality of doctor listening, respect, time and understandability of explanations]. Multivariate logistic regression was done to assess the ability to always receive high quality care, adjusted for income, insurance coverage, race/ethnicity, interview language, health status and age. Principal Findings: 4,497 children, representing 52 million children nationwide, had an identified PCP. Mean age was 8.0 years, 51% were male, and 24% were covered by Medicaid. 48% of parents identified their child s PCP as an individual. Parents who identified the child s PCP as an individual rated the ability to always get high quality care significantly higher than those identifying a site of care in 2 of 3 areas: getting care without long waits (22.4% vs. 15.8%, p<0.01) and doctor communication (54.2% vs. 44.5%, p< 0.001), but not for getting needed care (88.2% vs. 85.9%, p=0.06). In multivariate analyses, children whose parents identified an individual PCP had significantly higher odds of always getting care without long waits (OR 1.52; 95% CI 1.18-2.02), and highest quality doctor communication (OR 1.48; 95% CI 1.241.77), but only trended towards an increased ability for always getting needed care (OR 1.22; 95% CI 0.99-1.54). Conclusions: Parents who identify an individual rather than a facility as their child's PCP report receiving higher quality care. Presented by: Susan Haber, Sc.D., Senior Research Economist, , RTI International, 411 Waverley Oaks Road, Suite 330, Waltham, MA 02452; Tel: 781.788.8100; Fax: 781.788.8101; E-mail: shaber@rti.org Research Objective: Ethnic disparities in access to care for both insured and uninsured populations have been documented in numerous studies. This study uses survey data on children in Oregon’s Medicaid look-alike SCHIP program, collected under the Child Health Insurance Research Initiative (CHIRI), to compare the experience of Hispanic children (the primary ethnic minority in Oregon) with nonHispanic children and to explore the extent to which differences are explained by parental acculturation (as measured by language). Study Design: We conducted a telephone survey (in both English and Spanish) of parents of children in Oregon’s SCHIP program (N=1,206). Parents of Hispanic children were oversampled. Analyses compared non-Hispanic children, Hispanic children with English-speaking parents, and Hispanic children with Spanish-speaking parents. Population Studied: Children currently enrolled in or recently disenrolled from Oregon’s SCHIP program as of January 2002. Principal Findings: Over 70% of Hispanic parents and more than half of Hispanic children in our survey do not speak English at home. While there are substantial disparities between Hispanic and non-Hispanic children in Oregon’s SCHIP program, most of these are explained by parent’s language and there are generally few significant differences between English-speaking Hispanic and non-Hispanic children. Children of Spanish-speaking Hispanic parents were less likely to access primary care services than children of English-speaking Hispanic and non-Hispanic parents, despite having poorer parental rating of their health status. Nonetheless, Spanish-speaking parents were less likely to say their children had an unmet need for care. Although nearly all children have a usual source of care, most Spanish-speaking Hispanic children go to a hospital clinic or community health center, while other children mainly receive their care through a doctor’s office or HMO. Children from Spanish-speaking families were more likely to be insured during the year prior to enrolling in SCHIP. However, this was mostly through Medicaid and Spanish-speaking Hispanic families were only half as likely as English-speaking Hispanic and non-Hispanic families to have had private insurance or paid a premium for health insurance in the past. Among disenrollees, Spanishspeaking Hispanic children were the least likely to be currently insured and the least likely to have a usual source of care (but also the least likely to have an unmet need for care). Conclusions: Acculturation is an important driver of ethnic disparities in Oregon’s SCHIP program. Evidence of poorer access to care for Hispanic children with Spanish-speaking parents, despite their apparently poorer health status, is cause for concern. These utilization gaps may be explained by differences in parental perceptions of the need for care, as well as cultural differences in rating health status. Implications for Policy, Delivery or Practice: Policies that address ethnic disparities should be sensitive to the role of acculturation and variation even among members of the same ethnic group. Covering Spanish-speaking Hispanic children through policies that promote employer-sponsored insurance may be challenging because of their lack of experience with private insurance and their reliance on traditional safety net providers. Primary Funding Source: AHRQ, The David and Lucile Packard Foundation, HRSA • The Covering Kids and Families Evaluation: Findings from Parent Focus Groups on Access to Care Ian Hill, M.P.A., M.S.W, Holly Stockdale, M.P.H., M.P.P., Marilynn Evert, Katherine Gifford Presented by: Ian Hill, M.P.A., M.S.W, Senior Research Associate, Health Policy Center, The Urban Institute, 2100 M Street, N.W., Washington, DC 20037; Tel: 202.261.5374; Fax: 202.223.1149; E-mail: ihill@ui.urban.org Research Objective: The Covering Kids and Families (CKF) program, funded by the Robert Wood Johnson Foundation, seeks to expand health insurance coverage for children and families by supporting the outreach and enrollment efforts of community-based organizations across the country. As part of an evaluation of CKF, researchers conducted a series of focus groups to explore parents’ experiences accessing health care for their children, and to assess whether and how these experiences affect parents’ decisions to enroll in or renew coverage for their children under Medicaid or the State Children’s Health Insurance Program (SCHIP). Study Design: In the spring and summer of 2003, 13 focus groups were conducted in 5 cities—Boston, Massachusetts; Denver, Colorado; Los Angeles, California; Mena, Arkansas; and San Antonio, Texas. In each community, groups were conducted with parents of children insured in either Medicaid or SCHIP and parents of uninsured children. Three groups were conducted with Spanish-speaking parents in two communities—Denver and Los Angeles. The cities chosen, identified from the 10 states participating in the case study component of the evaluation, represented a range of “access scenarios” and provided geographic diversity. Population Studied: Parents of children insured in Medicaid or SCHIP and parents of uninsured children. Principal Findings: Generally speaking, access to primary care was considered good by most parents with children enrolled in Medicaid and SCHIP. This was true across all communities. For the uninsured, there was considerable variation in perceptions of access to care across communities. For example in Boston, where large numbers of private physicians participate in public programs, parents of uninsured children reported few problems obtaining care. Conversely, in Denver, where fewer providers participate in Medicaid or SCHIP, or provide charity care, uninsurance negatively affected parents’ ability to access care for their children. For parents of both uninsured and insured children, finding dentists and specialists was more difficult than finding primary care providers. Spanish-speaking families confront numerous additional barriers to obtaining care due to language barriers and perceived discrimination. Among all focus group participants, great value is placed on health insurance. Even when parents encounter problems accessing care, very few indicated a reluctance to enroll their children into Medicaid or SCHIP, or to renew their children’s public coverage. Conclusions: Medicaid and SCHIP programs appear to provide good access to primary health care services in both rural and urban communities. Dentists and specialists that accept Medicaid and/or SCHIP are more difficult to find. Efforts to expand outreach and further simplify application procedures to enroll families in Medicaid and SCHIP are essential as families with uninsured children continue to report difficulties accessing health care. Implications for Policy, Delivery or Practice: Policymakers should focus on strategies for expanding access to dental and specialty care and consider investing additional resources towards helping families navigate the health care system. Communities with high numbers of Spanish-speaking populations should focus on reducing barriers to care for these families, such as hiring more Spanish-speaking case workers, reducing discrimination, and helping families locate Spanish-speaking providers. Primary Funding Source: RWJF • Mental Health Need and Access to Services for CSHCN Moira Inkelas, Ph.D., M.P.H., Kandyce Larson, M.S.W., Kathryn Smith, M.S.N., M.A., Ramesh Raghavan, M.D., Ph.D., Susan Igdaloff, M.D. Presented by: Moira Inkelas, Ph.D., M.P.H., Assistant Professor, Health Services, UCLA School of Public Health, 1100 Glendon Avenue, Suite 850, Los Angeles, CA 90024; Tel: 310.794.0966; Fax: 310.794.2728; E-mail: minkelas@ucla.edu Research Objective: To examine self-reported need and unmet need for mental health care among CSHCN and their families, and explore access disparities by demographics, health care factors, and region. Study Design: Analysis of a new, nationally representative telephone survey of parents conducted by the National Center for Health Statistics in 2001 - the National Survey of Children with Special Health Care Needs - providing national and state estimates of access and quality for children with chronic conditions. Parents report if the child needed counseling or mental health services during the past year, if the family needed such care due to the childs condition, and if they obtained needed care. Population Studied: Parents of 38,866 children age 0-17 with chronic health conditions lasting at least one year. Principal Findings: About 25 percent of CSHCN are reported as needing mental health care while 13 percent have a family need. In logistic regression, low household income, high impairment of the child, changing rather than stable health care needs, and burden of the chronic condition on the family - measured by reduced work hours and more than one hour of weekly care coordination by the parent - are associated with higher odds of child and of family mental health care need, controlling for child age, gender, and race/ethnicity. About 16 percent of children and 20 percent of family members with a mental health need do not receive care. Of those needing care, odds of unmet need are higher for children who are African- American OR 1.43, CI 1.05-1.96, uninsured OR 3.95, CI 2.536.15, have high impairment OR 1.76, CI 1.41-2.20, and in households below 200 percent FPL. Similar access disparities are found for family members with the exception of no difference with race/ethnicity. With health care factors added to the model, odds of unmet need for the child, and a family member, are higher when the child lacks a personal physician or usual source of care, the parent reports that the childs care is not well organized, or family-centered care ratings are low. Unmet needs are greatest in Western states even adjusting for these demographic and health care factors. Conclusions: CSHCN and their family members have mental health needs that are not being adequately addressed. Rates of mental health needs among family members are independently associated with care-giving burden. Unmet mental health needs are more frequent among children who lack continuity of provider and receive lower interpersonal quality. Implications for Policy, Delivery or Practice: Children with special health care needs and their families face coping challenges that may increase their need for mental health services. Increasing coordination in and family-centeredness of primary and specialty care may improve identification of needs, improve access, and reduce disparities. Patterns of unmet need may be influenced by supply, reimbursement, and provider awareness and screening practices. The need for state-level supply and access-promoting policies are implied by regional disparities that persist even adjusting for family and health care factors. Primary Funding Source: California Healthcare Foundation • Access and Satisfaction with Care for CSHCN in Medicaid Managed Care and Other Types of Health Plans: An Analysis of the 2000 MEPS Paul Newacheck, Dr.PH, Sue Kim, Ph.D., M.P.H. Presented by: Sue Kim, Ph.D., M.P.H., Postdoctoral Scholar, Department of Medicine, University of California, San Francisco, 3333 California Street, Suite 335, San Francisco, CA 94143-0856; Tel: 415.502.4078; Fax: 415.502.8291; E-mail: sekim@medicine.ucsf.edu Research Objective: Children with special health care needs (CSHCN) -- defined as those children who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally -- use more health care services than other children and consequently have higher health care expenditures. Currently, there are no studies on this population using a nationally representative sample to examine access and satisfaction in managed care. The goal of this study is to examine whether access and satisfaction differed for Medicaid enrolled CSHCN in managed care organizations versus those not in managed care. Study Design: Medical Expenditure Panel Survey (MEPS) is designed to produce national estimates of the health care use, expenditures, and insurance coverage of the U.S. civilian noninstitutionalized population. We used the CSHCN definition adopted by the federal and state Maternal and Child Health programs, as operationalized by the CSHCN Screener, to identify the children with special health care needs. We used responses to a series of CAHPS questions included in the MEPS, which are designed to measure quality of care from consumer’s perspective, to examine access and satisfaction. We also distinguished CSHCN enrolled in Medicaid and whether or not they were in a managed care plan in the year 2000. Medicaid enrollment and health plan characteristics were determined using parental responses to survey questions in the MEPS. Population Studied: The 2000 MEPS data set contains 6581 children of which 973 (14.3%) were identified with special health care needs. There were 202 CSHCN in Medicaid managed care and 101 CSHCN in Medicaid but not in managed care. (Additional data from the 2001 MEPS will be added prior to the AcademyHealth meeting). Principal Findings: The preliminary results show that there is no significant difference between children with special health care need enrolled in Medicaid FFS and Medicaid HMO/managed care organizations in receiving a routine medical care visit in the past year or being able to get an appointment when needed. Both groups were equally likely to have had an illness or injury needing care in the past 12 months and receive care when wanted. The majority of respondents (69% for the managed care group and 80% for the non-managed care group) indicated that they did not have a problem in getting necessary care in the past 12 months. About 76% of those in non-managed care plans responded that the child’s physician always listened carefully to the parents, while only about 60% of those in managed care plans felt that the child’s doctor always listened to them (P<.01). Also, 74% of those in non-managed care plans responded that the child’s physician always showed respect for what the parents had to say, compared to 58% for those enrolled in managed care plans (P<.01). In addition, a higher percentage of the non-managed care group (69% vs. 49%) responded that the child’s physician spent enough time with the child and parent (P<.05). Conclusions: It appears that there is no significant difference in health care access for CSHCN enrolled in managed and non-managed Medicaid plans. The majority of the respondents were able to receive routine care, had no problem receiving necessary care, or getting referrals to a specialist. However, from the parents’ perspective, CSHCN enrolled in managed care Medicaid plan seems worse off in terms of family centered care. Those enrolled in managed care showed a lower satisfaction with their physicians, regarding time spent with child and parent, showing respect, and listening carefully to the parents. Implications for Policy, Delivery or Practice: Policy makers may use this information to examine state Medicaid enforcement since federal Medicaid law requires access to care in HMO/managed care to be at least as good as it is in Medicaid FFS. Before making any policy changes, it would be important to explore whether lower satisfaction with managed care plans is associated with lower clinical quality of care received. Primary Funding Source: Maternal and Child Health Bureau, DHHS Call for Papers Child Health Challenges: New Research Approaches Chair: Patrick Vivier, M.D., Ph.D. Tuesday, June 8 • 11:15 a.m.-12:45 p.m. • Racial Disparities in Hospital Admissions and Surgical Management of Children with Appendicitis T.M. Bird, M.S., Evan Kokoska, M.D., J. Alex Reading, M.A., John Tilford, Ph.D., James Robbins, Ph.D. Presented by: T.M. Bird, M.S., Research Associate, Pediatrics, University of Arkansas for Medical Sciences, 800 Marshal Street, Little Rock, AR 72202; Tel: 501.364.4936; Fax: 501.364.1552; E-mail: birdtommym@uams.edu Research Objective: To assess racial and insurance disparities and trends in hospital admissions and surgical management of children with appendicitis. Study Design: We analyzed data from the Healthcare Cost and Utilizations Project (HCUP) Kids’ Inpatient Database (KID) for the years 1997 and 2000. The KID consists of an 80% sample of pediatric discharges from all hospitals in participating states; 22 in 1997 and 27 in 2000. Data are weighted to provide national estimates. We reviewed all records for children = 18 years of age at time of admission with an ICD-9 discharge diagnosis code for acute appendicitis. Outcomes included type of surgery (open or laparoscopic), length of stay (LOS), operative delay, incidence of surgical complications, and hospital charge. Population Studied: The 1997 KID has a total of 1.9 million discharge records from 2,521 hospitals of patients 18 years of age and younger. The 2000 KID includes 2.5 million discharge records from 2,784 hospitals of patients 20 years of age and younger. We restricted our analysis to those patients age 18 years or less at the time of admission with an ICD-9 diagnosis code of simple (540.9) or complicated (540.0 and 540.1) appendicitis. Principal Findings: Weighted to represent national estimates, 73,330 cases were diagnosed with appendicitis in 1997 and 91,100 cases in 2000. Of these, only 6.6% in 1997 and 6.8% in 2000 were African American. In the year 2000, African Americans accounted for 15% of children 0 to 18 years of age in the U.S. population and 18% of hospitalizations in the KID. Even though the hospital incidence rate is lower than expected, African American children were more likely than Caucasians to be admitted with complicated appendicitis (odds ratio (OR) 1.16, p = 0.002), more likely to have a complication (OR = 1.34, p = 0.038), and less likely to undergo laparoscopic surgery (OR = 0.75, p < 0.001). When compared to Caucasians, African Americans also had a greater surgical delay, a longer length of stay, and a greater hospital charge. Conclusions: This national study demonstrates substantially lower rates of hospitalization for appendicitis and worse outcomes among African American children. The finding of a lower hospitalization rate for African Americans has not been previously reported in the epidemiology of appendicitis. Implications for Policy, Delivery or Practice: Higher perforation and complication rates, longer wait times until first procedure, and lower rates of laparoscopic techniques among African American children illustrate disparities in access to care for minority youth. • Changes in Newborn Delivery during a Period of Rapid Expansion of Medicaid Managed Care in Los Angeles and Orange County, California Ruey-Kang Chang, M.D., M.P.H., Sandra Rodriguez, B.S., Thomas Klitzner, M.D., Ph.D. Presented by: Ruey-Kang Chang, M.D., M.P.H., Assistant Professor, Pediatrics, David Geffen School of Medicine at UCLA, B2-427 MDCC, 10833 Le Conte Avenue, Los Angeles, CA 90095; Tel: 310.825.6197; Fax: 310.825.9524; E-mail: rkchang@ucla.edu Research Objective: We sought to determine changes in newborn deliveries during a period of rapid Medi-Cal managed care (MMC) expansion in Los Angeles and Orange County, two of the most populated counties in California. The objectives of this study were to determine if: 1) The Medi-Cal newborn delivery market became decentralized over time with MMC expansion; 2) Decentralization increased the rate of inter-hospital transfer; 3) Decentralization changed the pattern of care (rate of cesarean section); 4) Decentralization changed the outcomes of care. Study Design: The California statewide abstracted hospital discharge data from the January 1990 to December 1999 were used to conduct the analysis. California Vital Statistics on birth record were used to compare the numbers of births each year. American Hospital Association database on hospitals was used to determine the ownership of the hospitals. Herfindahl-Hirschman Index (HHI) was calculated to measure the distribution of newborn deliveries among hospitals. Percentages of deliveries by cesarean section were calculated. Outcomes of birth and deliveries were measured by calculating percentages of in-hospital deaths, birth weight<1500 gm, and inter-hospital transfers. Population Studied: All newborn deliveries in Los Angeles County and Orange County, CA hospitals between 1990 and 1999. Principal Findings: There were 2,351,199 newborn deliveries (LAC 1,832,287, OC 518,922) in 124 hospitals 1990-1999. The number of newborn dekiveries per year decreased by 21% in that period. Dramatic decline in the numbers of deliveries (up to 80%) was seen in all four LAC county hospitals. The overall market share of public hospitals decreased from 22% in 1990 to 8% in 1999 and the loss of market share was mostly picked up by not-for-profit hospitals, which increased market share from 54% to 68%. The newborn delivery market for Medi-Cal patients in both LAC and OC became less concentrated as evidenced by decreasing HHI. During the same period, the HHI for private patients increased slightly (more concentrated) for both counties. The rate of cesarean section for private patients decreased between 1990-1996, followed by a rise 1996-1999. In contrast, cesarean section rate for MediCal patients did not decline but continued to rise over the study period. Patterns of convergence in the CS rate over the study period between private and Medi-Cal patients were seen in both LAC and OC. The rate of newborn transfer for patients with Medi-Cal in LAC remained unchanged (around 0.8%). The newborn in-hospital mortality rates in both LAC and OC decreased and there was no significant changes in the rate of low birth weight newborns in LAC and OC over the 10-year study period. Conclusions: The expansion of MMC in LAC and OC was associated with a dramatic shift of newborn deliveries from public hospitals to not-for-profit hospitals. The increase in cesarean section rate among Medi-Cal patients may be a result of this market shift. At the same time, outcomes of newborn deliveries, including in-hospital mortality, interhospital transfer and low birth weight rate, did not change significantly. Implications for Policy, Delivery or Practice: Medicaid managed care programs appear to have resulted in decentralization of newborn deliveries among hospitals in LAC and OC. Such decentralization was associated with changes in the patterns of care, but did not have adverse effect on the outcomes of care. Primary Funding Source: AHRQ • Use of Atypical Antipsychotic Drugs by Children and Adolescents in the United States: A Retrospective Cohort Study Lesley Curtis, Ph.D., Leah Masselink, B.A., Truls Ostbye, M.D., Ph.D., Steve Hutchison, Ph.D., Ranga Krishnan, MB, ChB, Kevin Schulman, M.D. Presented by: Lesley Curtis, Ph.D., Assistant Research Professor, Center for Clinical and Genetic Economics, Duke Clinical Research Institute, Duke University Medical Center, P.O. Box 17969, Durham, NC 27715; Tel: 919.668.8101; Fax: 919.668.7124; E-mail: lesley.curtis@duke.edu Research Objective: Previous research has suggested increased use of atypical antipsychotic drugs in pediatric populations. We examined the prevalence of atypical antipsychotic use by age and sex among children and adolescents in the United States. Study Design: We conducted a retrospective cohort study using the administrative claims database of a large pharmaceutical benefit manager. The main outcome measure was prevalence of prescriptions, which we calculated for the 5 atypical antipsychotic drugs and for concurrent use of antidepressant drugs. We stratified the analysis to explore age and sex differences in use of the drugs, and we used chisquare or Fisher exact tests to test for differences in proportions and prevalence. Population Studied: Subjects were included if their insurance carriers required the benefit manager to track claims at the subject level, excluding those whose plans used a single identifier for multiple family members. The data set consisted of 6,213,824 outpatients aged 19 years and younger who were enrolled continuously from January through December 2001 and who filed at least 1 claim for a prescription drug during that period. Each subject's claims were linked using a unique identifier encrypted to ensure confidentiality. A total of 1171 insurers were represented, covering all 50 states, the District of Columbia, and US territories. Principal Findings: Prevalence of atypical antipsychotic use was 267.1 per 100,000 subjects (16,599/6,213,824). Compared to the overall study population, subjects with at least 1 claim for an atypical antipsychotic were more likely to be male (70.7% vs 51.2%; P<.001) and were older (76.9% vs 51.6% of subjects aged 10 through 19 years; P<.001). Prevalence peaked at 594.3 per 100,000 among male subjects aged 10 through 14 years, and at 291.0 per 100,000 among female subjects aged 15 through 19 years. Nearly one quarter (3830/16,599) of subjects with a claim for an atypical antipsychotic were aged 9 years or younger, and nearly 80% of those (3021/3830) were male. In contrast, the prevalence of concurrent antidepressant use was significantly higher among female subjects than among male subjects (192.6 vs 106.8 per 100,000; P<.001). Conclusions: Although evidence regarding the safety and efficacy of atypical antipsychotics in pediatric populations is limited, nearly one quarter of children and adolescents with claims for those drugs were younger than 9 years. Understanding the long-term effects of early and prolonged exposure to atypical antipsychotics is crucial given their extensive use in pediatric populations. Implications for Policy, Delivery or Practice: Off-label use of prescription drugs in children and adolescents is common, and some evidence suggests that primary care physicians are more likely than experts in pediatric psychopharmacology to prescribe psychotropic drugs. For patients covered by Medicaid, the incentive to treat behavioral problems using drug therapy may be especially strong, because Medicaid provides almost complete coverage for drug therapy and only limited reimbursement for psychiatric evaluation. Researchers must develop a better understanding of the circumstances in which physicians prescribe atypical antipsychotics to children and adolescents, especially given the scarcity of data regarding long-term effects of these drugs. Primary Funding Source: AHRQ • Newborn Hospitalizations for Birth Defects In the Pre and Post Folic Acid Fortification Periods James Robbins, Ph.D., John Tilford, Ph.D., T. M. Bird, M.S., Mario Cleves, Ph.D., Joseph Thompson, M.D., M.P.H., Charlotte Hobbs, M.D. Ph.D. Presented by: James Robbins, Ph.D., Professor, Pediatrics and Psychiatry, University of Arkansas for Medical Sciences, 800 Marshall Street, Little Rock, AR 72202; Tel: 501.364.8370; Fax: 501.364.1552; E-mail: robbinsjamesm@uams.edu Research Objective: To compare newborn hospitalization rates for birth defects during 1997, prior to mandatory fortification of grains with folic acid, and during 2000, after mandatory fortification. Study Design: Analyses use the Kid s Inpatient Database (KID) of hospital discharges for 1997 and 2000. The KID is the only all-payer, nationally representative, inpatient care database for children in the United States. Data are weighted to represent all births in the U.S. and are comparable across years. Population estimates and standard errors were calculated from weights provided by the Agency for Healthcare Research and Quality. Analyses compared newborn hospitalization rates for select birth defects per 10,000 live births across years for defects expected to be influenced by folic acid and defects not known to be influenced by folic acid. Population Studied: The 1997 and 2000 KID were accessed to identify hospital discharges for congenital anomalies easily recognized at birth or likely to require inpatient care within the first few days of life. ICD-9 discharge codes for newborns less than 10 days of age were used to define anomalies. To avoid duplicate counting of cases, infants discharged to an acute care hospital were excluded. These patients would likely be captured in the sample of the referral hospital. Principal Findings: Among birth defects thought to be affected by folic acid fortification, newborn hospitalization rates decreased significantly for four defects: spina bifida (3.30 to 2.75 per 10,000 live births), upper limb defects (2.13 to 1.88), lower limb defects (1.37 to 1.11), and common truncus arteriosis (0.80 to 0.57). Rates of orofacial clefts did not change. Newborn hospitalization rates of defects not known to be associated with folic acid (hypospadias, diaphragmatic hernia, obstetric genitourinary defects) did not change. Conclusions: Decreases in newborn hospitalization rates for spina bifida and limb defects are consistent with the known protective effect of folic acid. Results do not support a reduction in rates of orofacial clefts, despite literature suggesting that folic acid should reduce the risk of these defects. Differences over time may have been influenced by differences in diagnostic precision, maternal age, or other maternal characteristics. Implications for Policy, Delivery or Practice: In response to strong evidence that folic acid can reduce the prevalence of neural tube defects, the FDA mandated fortification of grain products with folic acid to begin in 1998. This study of national hospitalization rates for birth defects supports a more pervasive impact of the fortification policy. Primary Funding Source: CDC • Age-Specific Pathophysiologic Mortality Models for General Pediatric Inpatients Ying Tabak, Ph.D., Richard Johannes, M.D., M.S. Presented by: Ying Tabak, Ph.D., Senior Biostatistician, Research, CardinalHealth - Data and Clinical Information, 500 Nickerson Road, Marlborough, MA 01752; Tel: 508.571.5120; Fax: 508.571.6101; E-mail: ying.tabak@cardinal.com Research Objective: Studies of risk-adjusted mortality in pediatric patients have been limited to relatively small samples of ICU patients in teaching hospitals. The validity for community pediatric patients remains unknown. Moreover, age-specific weights have been applied only to vital signs (VS). No age-specific effect of laboratory values has been studied in spite of rapid developmental changes in laboratory values across childhood, especially early childhood. The goal of this study is to develop and validate age-specific pediatric mortality risk models for general pediatric inpatients using commonly measured objective pathophysiologic variables, including laboratory assessment, vital signs, and status of neurologic function. Study Design: Retrospective lab data were imported from hospitals’ electronic systems or abstracted from chart review, if automated data were not available. Vital signs and the Glasgow Coma Scores were abstracted from chart review. Age-specific normal ranges of laboratory and VS variables were crafted by referring to the medical literature and empirical examination of the data for three age groups, Neonates (0-30 days), Young Children (1-23 months), and Older Children (2-17 years). Logistic regressions were used to derive risk adjustment models, which were validated with Bootstrapping techniques. Population Studied: A total of 243,173 pediatric inpatients, excluding healthy newborns, admitted in 2000-2001 from 215 acute care hospitals were included. There were 93,011 neonates (507 deaths, .55% mortality), 46,152 young children (170 deaths, .37% mortality), and 104,010 older children (421 deaths, .40% mortality). Principal Findings: Variables that entered into all three models with generic thresholds included low platelets (<=150 10^9/L) and hypothermia (<=95F). Variables that entered into all three models with age-specific thresholds included elevated creatinine, hyperglycemia, lower heart rates, and systolic hypotension. The thresholds of elevated creatinine decreased with age (from .8mg/dL to .5mg/dL). The thresholds for hyperglycemia increased with age (>110 mg/dL, 200 mg/dL, and 300 mg/dL respectively). The risk of lower heart rates posed greater risk for neonates and younger children and the threshold was much higher for neonates (<=120) than older children (<=60). The threshold of systolic hypotension increased significantly across age groups (<=50, <=70, and <=80 respectively). All of these variables had odds ratios greater than 1.5 and p<.05. The three models contain between 11-15 variables, all of which were significant at p<.05 or better. The models showed excellent predictive power with c-statistics of .85, .86, and .89 respectively. Conclusions: The thresholds for pathophysiologic determinants vary by age. Risk adjustment using pathophysiologic variables should consider the age specificity in order to capture and quantify risks more precisely. Agespecific weights are more clinically plausible. The current models also demonstrated that commonly measured pathophysiologic variables are adequate in predicting mortality for general pediatric populations. Implications for Policy, Delivery or Practice: This study provides age-specific risk adjustment tools that are clinically valid and cost-effective. The pathophysiologic data are either automated or have potential for automation. The parsimonious models have practical values to providers, purchasers, government agencies, and public health groups for quality improvement, cost containment, and performance reporting in hospitalized general pediatric patients. Related Posters Poster Session A Sunday, June 6 • 6:45 p.m.-8:00 p.m. • Parental Factors Associated with Childhood Immunization Status: Results from the National Immunization Survey Norma Allred, M.S.N., Ph.D., Kate Shaw, M.S., Tammy Santibanez, Ph.D., Donna Rickert, Dr.PH Presented by: Norma Allred, M.S.N., Ph.D., Epidemiologist, National Immunization Program, Centers for Disease Control and Prevention, 1600 Clifton Road, N.E., Mailstop E-52, Atlanta, GA 30333; Tel: 404.639.8722; Fax: (404) 639-8614; Email: NAllred@cdc.gov Research Objective: To measure the association of parental knowledge, attitudes and beliefs about immunization and the immunization status of their 19-35 month old children. Study Design: A supplemental module was administered from July 2001 to December 2002 to randomly selected parents in the National Immunization Survey (NIS), a national random digit telephone survey of households with children aged 19-35 months conducted annually to determine immunization status. The module included selected questions regarding vaccine safety and side effects, simultaneous vaccine administration, new vaccines and vaccinating an ill child. Chi square tests and logistic regression analyses were performed to examine associations of attitudes and beliefs with demographic characteristics and 4:3:1:3:3 up-to-date status (4+ doses of diphtheria and tetanus toxoids and pertussis vaccine, 3+ doses of polio vaccine, 1+ dose of measles-containing vaccine, 3+ doses of Haemophilus influenzae type b vaccine and 3+ doses of hepatitis B vaccine). Population Studied: Nationally representative, populationbased sample of households with children between the ages of 19-35 months Principal Findings: Between July 2001 and December 2002, 48,531 NIS telephone interviews were completed. For 32,707 of those interviews, verbal consent to contact identified providers was obtained and adequate provider data were obtained, thus yielding validated vaccination coverage data for 67.4% of interviews. Of the 9908 parents who were selected and completed the additional module, 7810 (79%) had provider-verified data and are included in this analysis. There was a significant association between parental concern about vaccine safety and their child’s immunization coverage; for those with the highest concern, coverage was 75%, for intermediate concern 65%, and for the lowest concern 53%, (p<0.01, n=7789). Children of parents who disagreed that children who stayed at home should receive the same vaccines as children in day care or pre-school had lower coverage levels (65% vs. 75%, p<0.05, n=7727). These differences remained significant after controlling for demographic characteristics. No other significant associations were found. Conclusions: The finding from this study that parental concern over vaccine safety is associated with immunization status has been reported in previous research. The significant association found between parental disagreement over which children should be immunized based on attendance in a day care or pre-school is a new finding that should be further explored. Implications for Policy, Delivery or Practice: Strategies that health care providers can use to reassure parents about vaccine safety and educate them about the importance of immunizations for all children may have a positive impact on vaccine coverage. Primary Funding Source: CDC • Prolonged Bottle-Feeding Associated with Iron Deficiency Jane Brotanek, M.D., Jill Halterman, M.D., M.P.H., Michael Weitzman, M.D., Karen Nead, M.D., M.P.H., Peggy Auinger, M.S. Presented by: Jane Brotanek, M.D., Fellow, General Pediatrics, Pediatrics, HRSA, 601 Elmwood Avenue, Box 278881, Rochester, NY 14642; Tel: 585.275.1544; Fax: (585) 5060150; E-mail: jane_brotanek@urmc.rochester.edu Research Objective: Iron deficiency in infancy and early childhood is associated with behavioral and cognitive delays. Few studies have explored the contribution of infant feeding practices, particularly prolonged bottle-feeding, to iron deficiency among toddlers. The objective of this study is to examine the association between prolonged bottle-feeding and iron deficiency among a nationally representative sample of children ages 1-3 years. Study Design: The National Health and Nutrition Examination Survey III 1988-1994 provides cross-sectional data on the feeding practices of children 1-3 years of age and contains measures of iron status including transferrin saturation, free erythrocyte protoporphyrin, and serum ferritin. Children were considered iron-deficient if any 2 of these values were abnormal for age and gender. The prevalence of iron deficiency and the duration of bottle-feeding were determined for toddlers from three major ethnic groups (Black, White, Mexican-American). Bivariate comparisons of the prevalence of iron deficiency with duration of bottle-feeding were performed. Logistic regression was used to examine the relationship between iron deficiency and duration of bottlefeeding, controlling for the effects of age, gender, lead level, obesity, maternal education and poverty status, and duration of infant breastfeeding and/or formula feeding. Population Studied: A nationally representative sample of children ages 1-3 years living in the United States between 1988-1994. Principal Findings: The prevalence of iron deficiency was 3% among White children, 4.7% among Black children, and 10.6% among Mexican-American children ages 1-3 years (p<0.001). With increasing duration of bottle-feeding, the prevalence of iron deficiency among all children increased (2.2%, bottle-fed <= 12 months; 6.6%, stopped bottle-feeding between 13 and 23 months; and 7.4%, stopped bottle-feeding between 24 and 48 months, p<0.001). At 24-48 months, 35.5% MexicanAmerican children were still being bottle-fed, as compared with 17.3% White children and 15.7% Black children (p<0.001). In a multivariate model, bottle-feeding into the 24-48 month age range and Mexican ethnicity both independently predicted iron deficiency (OR 2.7, 95% CI 1.3, 5.5 and OR 3.1, 95% CI 1.7, 5.7, respectively). Conclusions: Children with prolonged bottle-feeding are at risk for iron deficiency. Implications for Policy, Delivery or Practice: Screening practices may need to be modified to reflect this increased risk, especially the substantial risk among Mexican-American toddlers. Primary Funding Source: HRSA • The Effect of Primary Care Practice Characteristics on Pediatric Emergency Department Utilization David Brousseau, M.D., MS, John Meurer, M.D. M.B.A., Evelyn Kuhn, Ph.D., Mayme Isenberg, M.S., Marc Gorelick, M.D., MSCE Presented by: David Brousseau, M.D., MS, Assistant Professor, Pediatrics, Medical College of Wisconsin, 9000 W Wisconsin Avenue, Milwaukee, WI 53226; Tel: 414.266.2625; Fax: (414) 266-2635; E-mail: dbrousse@mail.mcw.edu Research Objective: To determine the relationship between the characteristics of a pediatric practice and ED utilization through analysis of practice and provider characteristics. Study Design: Retrospective cohort Population Studied: Retrospective cohort of children who received their primary care from a single network of twelve pediatric practices (28 pediatricians) and who were insured by United Healthcare of Wisconsin. From an insurance administrative dataset, demographic data and utilization data from 12/1/1999 through 7/31/2001 were collected for all children who had at least one visit to a practice physician. Primary care practices were contacted and characteristics of the physicians/practices were obtained. A backward stepwise hierarchical multiple regression model, controlling for person level demographics, was used to evaluate the association between these characteristics and ED reliance (the percentage of all visits for a patient that occur in the ED). Principal Findings: A total of 9,208 children were included in the analysis. Their average age was 7.7 years, 51% were male, and 21% were insured through Medicaid. The children made 52,717 visits to healthcare providers, of which 4,512 were to the emergency department. Children whose primary care providers had fewer weekends of call (p<0.05), fewer weekend office hours (p<0.001) and a higher percentage of Medicaid patients (p<0.002) showed higher ED reliance. Fewer patients per hour worked (p=0.08) also trended towards higher ED reliance, but this may be explained by the correlation between a lower number of patients and fewer years of service. Conclusions: Children cared for by more accessible primary care providers, as measured by more frequent weekend call and working in practices with more weekend hours, rely less on the ED for care. Implications for Policy, Delivery or Practice: Changes in practice characteristics, which make an individual provider more available, may decrease emergency department utilization. Primary Funding Source: Children's Hospital Foundation • When the Bough Breaks: Provider-Initiated Comprehensive Care is More Effective and Less Expensive for Sole-Support Parents on Social Assistance Gina Browne, Ph.D., Reg.N., Carolyn Byrne, Ph.D., Reg.N., Jacqueline Roberts, M.Sc., Reg.N., Amiram Gafni, Ph.D., Susan Whittaker, M.Sc., B.Sc., B.A. Presented by: Gina Browne, Ph.D., Reg.N., Founder & Director, System-Linked Research Unit; Professor, Nursing & C.E.&B., School of Nursing, McMaster University, Faculty of Health Sciences at Frid Street, 75 Frid Street, Building T30, Hamilton, Ontario, L8P 4M3; Tel: 905.525.9140 Ext. 22293; Fax: (905) 528-5099; E-mail: browneg@mcmaster.ca Research Objective: This five-year study conducted in Ontario, Canada is designed to assess the effects and expense of adding a mix of provider-initiated interventions to the health and social services typically used in a self-directed manner by sole-support parents and their children receiving social assistance in a national system of health and social insurance. Study Design: Families were randomized to receive proactive in-home visits by nurses, employment retraining, and age appropriate childcare, recreation, or skills development for all children in the household alone or combined and further compared to their own self-directed use of services. Population Studied: This was a 5-arm prospective randomized trial of 765 single parents on social assistance and their 1330 children (aged 0 - 24 years). Principal Findings: Results from a 2-year interim analysis show that providing social assistance families with proactive comprehensive care (health promotion, employment retraining, and recreation activities for children) compared to allowing families to fend for themselves in a self-directed manner, results in 15% more exists from social assistance within one year and substantial savings to society in terms of social assistance payouts. Conclusions: It is more effective and creates more savings, yet no more expensive to provide health and social services in a comprehensive fashion to parents and all children in a household on social assistance. Implications for Policy, Delivery or Practice: This study funded by Health Canada presents clear evidence that providing comprehensive care to social assistance recipients produces tremendous short and long term financial gains and societal benefits. Primary Funding Source: Health Canada • Predictors of High Cost Admissions for Congenital Heart Surgery Jean Connor, DNSc., R.N., CPNP, Kimberlee Gauvreau, ScD, Kathy Jenkins, M.D., M.P.H. Presented by: Jean Connor, DNSc., R.N., CPNP, Research Fellow, Cardiology, Children's Hospital Boston, 300 Longwood Avenue, Boston, MA 02115; Tel: 617.355.8890; Fax: 617-739-5802; E-mail: Jean.Connor@cardio.chboston.org Research Objective: To identify patient, institutional, and regional factors associated with high cost admissions for congenital heart surgery. Study Design: We used hospital discharge data from the Healthcare Cost and Utilization Project (HCUP) Kid’s Inpatient Database (KID) year 2000(data from 27 states). High cost admissions were defined as those in the highest decile for total hospital charges. Univariate and multivariate analyses with and without patients who died were used to determine demographic and hospital predictors for an increased frequency of high cost cases. Case mix severity was approximated using RACHS-1 risk groups. Regional and state differences were also examined. Population Studied: Cases of congenital heart surgery < 18 years of age. Principal Findings: Among 10,569 cases of congenital heart surgery identified, median hospital charges were $53,828. Statewide differences in the number of high cost admissions were present; CA, CO, FL, HI, PA and TX had more high cost cases and ME and SC had fewer. Subsequent analyses were performed adjusting for baseline state effects. Multivariate analyses with and without patients who died using generalized estimating equations revealed RACHS-1 risk category (OR 1.69-14.7), age (OR 3.9), prematurity (OR 4.7), the presence of other major non-cardiac structural anomalies (OR 2.5), Medicaid insurance (OR 1.47) and admission during a weekend (OR 1.64) to be independent predictors of a higher frequency of high cost cases (p<0.05). Although some institutional differences were noted in univariate analyses, bedsize, teaching and children’s hospital status, hospital ownership, and hospital volume of cardiac cases were not independently associated with greater numbers of high cost admissions. Conclusions: States varied in the frequency of high cost admissions for congenital heart surgery. Patients with greater disease complexity, younger age, prematurity, other anomalies, Medicaid and admitted during a weekend were more likely to result in high cost. Institutions of various types did not differ in frequency of high cost admissions, regardless of children’s hospital or teaching status. Implications for Policy, Delivery or Practice: Using hospital charge data as a surrogate for cost could be considered useful to health care providers, institutions, payors, and policy makers when formulating interventions and policies to allocate resources for complex congenital heart surgery • Children's Healthcare in the National Healthcare Quality and Disparities Reports: Findings, Challenges, and Opportunities Denise Dougherty, Ph.D., Susan Meikle, M.D., Pamela Owens, Ph.D., Edward Kelley, Ph.D., Ernest Moy, Ph.D. Presented by: Denise Dougherty, Ph.D., Senior Advisor, Child Health, U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850; Tel: 301.4271868; Fax: 301 4271347; E-mail: ddougher@ahrq.gov Research Objective: In 2003, the UDSDHHS, led by the Agency for Healthcare Research and Quality, released two landmark reports, the National Healthcare Quality and National Healthcare Disparities Reports. We will present selected findings from these reports on children's healthcare quality and disparities, and provide an analysis of why the reports did not pay more attention to children's issues, and the challenges and opportunities for the reports in the future. Study Design: The NHQR and NHDR were developed by AHRQ and 2 federal interagency advisory committees who relied in turn on non-federal advice. NHQR reports on the six IOM quality domains. The NHDR reports on disparities in quality, access, and use for AHRQ's 8 congressionallymandated priority populations (children, women, elderly, lowincome, inner-city, rural, people with special health care needs, racial and ethnic minorities) by race/ethnicity and income. Data reported in the reports were driven by criteria of national representativeness, collection over time, and a focus on high-cost, high-prevalence conditions at a national level. In addition, the first reports were intended to provide broad national snapshots of healthcare quality and do not provide in-depth analyses of quality for particular populations. Our analysis of the reports from a child healthcare perspective focuses on the implications of these criteria for reporting on children's healthcare quality. Population Studied: This is more a policy analysis than a study of a population per se, although findings from the reports on children will be presented. Available data on children's healthcare quality, using the reports' criteria, were studied by the report development team. For this analysis, we contrasted the reports' criteria for inclusion with the reality of children's healthcare and availability of children's healthcare quality and disparities information. Principal Findings: Quality and disparities issues for children were identified in the NHQR and NHDR. For example, the reports found that the poorest children are nearly twice as likely to be admitted to the hospital for gastroenteritis (an indicator of possible poor ambulatory care), and that black children are nearly twice as likely to be admitted to the hospitl for asthma (another indicator of possibly poor ambulatory care). A wealth of data are available in the appendix tables accompanying the report, but may not be highlighted in the main reports. Quality measures for children are relatively new, and few measures are being used to collect data in routine nationally representative data collection efforts. Children are less likely than adults to suffer from the high-prevalence, highcost chronic conditions that the report focused on. Conclusions: The reports provide guidance on quality and disparities gaps to close in children's health care. AHRQ seeks input on how to improve reporting on children's healthcare in future reports. In the longer term, attention to children may improve 1) with development and implementation of additional quality measures for children; 2) if there are changes in the ways that priorities are set in health; or 3) both. Meeting participants will be asked for input on these issues. Implications for Policy, Delivery or Practice: Findings on children in the first NHQR and NHDR can be used to set priorities for local quality improvement and disparities reduction efforts. The reports, in combination with other initiatives on children's healthcare quality, also provide a roadmap for where measurement of quality and disparities in children's health care needs to go. Primary Funding Source: AHRQ • Recommendations for the Development of Child Health Information Systems to Meet Medical Care and Public Health Needs Kristin Saarlas, M.P.H., Nicole Fehrenbach, M.P.P., Alan Hinman, M.D., M.P.H., David Ross, ScD, Nicole Fehrenbach, M.P.P. Presented by: Nicole Fehrenbach, M.P.P., Senior Research and Evaluation Associate, Public Health Informatics Institute, Emory University, 750 Commerce Drive, Suite 400, Decatur, GA 30030; Tel: 404.687.5622; Fax: (800) 765-7520; E-mail: nfehrenbach@taskforce.org Research Objective: The objectives of the December 2003 conference were to: 1. Review national initiatives and other factors influencing the development of child health information systems infrastructure. 2. Develop concrete recommendations, reflecting the input of stakeholders, for the development of immediate and 3-5 year actions to integrate the information about the health care that a child receives, from the moment he or she is born, in a simple yet comprehensive format so that the end user (parents, families, health professionals, insurers and policymakers) can take all appropriate actions. 3. Enlist stakeholders in communicating, supporting, and implementing the recommendations. Study Design: All Kids Count, a national program funded since 1992 by the Robert Wood Johnson Foundation, hosted an invitational conference in Atlanta, December 3-4, 2003. The conference was co-sponsored by 17 organizations and government agencies, including AHRQ, HRSA, CDC, CMS, AAP, ASTHO, AHCP, Commonwealth Fund, Family Voices, March of Dimes, and NICHQ. Over 100 representatives from 55 organizations and agencies attended the conference and worked to forge recommendations in the areas of governance and stakeholder involvement; information infrastructure, economic and funding issues, and use of information. Population Studied: The participants addressed the needs of all children, especially those with special health care needs and at-risk populations, in the course of developing the recommendations. Principal Findings: Recommendations for each of the four areas were made and will be available in the upcoming conference proceedings (www.allkidscount.org) . Common threads in the recommendations were: 1. The need to develop a national coalition of stakeholders to promote integration of separate child health information systems within the context of ongoing national initiatives such as NHII and PHIN; 2. The need to develop the business and policy cases for integrated child health information systems; 3. The need to develop agreement on standards for collecting and transferring information; and 4. The need to get the word out about the importance of integrating separate child health information systems to improve health and health services. Conclusions: There are many efforts underway to develop clinical or public health child health information systems but little attention is being paid to integrating the information from those systems. Such integration would improve our ability to identify the multiple health care needs of children and ensure services were provided in a timely and effective manner. Broad dissemination and endorsement of the recommendations from the conference are essential next steps. Implications for Policy, Delivery or Practice: The quality and delivery of health care services for children can be greatly improved through information technology. However, public health and medical care agencies must work closely together to develop information systems that integrate and link information in a complete and comprehensive way. The recommendations and action plan from this conference are significant in that they were developed with broad stakeholder input, including consumer and family advocates. Policy makers and program officers from each of the co-sponsoring agencies can use these recommendations when addressing issues related to health information systems for children. Primary Funding Source: RWJF • Detection of Health-Related Social Problems in Pediatric Primary Care Settings Using a Computer-Based Assessment Tool Eric Fleegler, M.D., Tracy Lieu, M.D., M.P.H., Paul Wise, M.D., Sharon Muret-Wagstaff, Ph.D., M.P.A. Presented by: Eric Fleegler, M.D., Fellow, Division of Emergency Medicine, Children's Hospital Boston, 300 Longwood Avenue, Boston, MA 02115; Tel: 617.355.2565; Fax: (617) 975-3691; E-mail: eric.fleegler@childrens.harvard.edu Research Objective: To assess the acceptability of and interest in a computer-based survey for identifying major health-related social problems and referral of families to appropriate social services. To use this tool (The Online Advocate, www.onlineadvocate.org) to determine the percentage of families in pediatric primary care clinics with one or more health-related social problems in the following domains: 1. Access to health care; 2. Housing; 3. Food insecurity; 4. Income insecurity; 5. domestic violence Study Design: Cross-sectional, self-administered, computerbased survey. Research assistants approached participants to take the survey on a laptop computer in the clinic waiting room and/or examination rooms. The survey was administered to the next eligible participant when a computer became available. Population Studied: The survey was administered in two primary care pediatric clinics in Boston, MA, to primary caregivers of children up to 6 years old attending well-child visits. Enrolled subjects were literate in either English or Spanish. Of 450 subjects approached 260 were eligible and 205 (79%) consented. Principal Findings: Acceptability: Of 260 eligible subjects, 12 (4.6%) were illiterate. Of the 205 consented, 194 (95%) completed the survey in an average of 16 minutes. Ninety two percent of families expressed acceptance of The Online Advocate as a tool for assessment and referral within their pediatrician’s office (welcome it, 62%; not mind at all, 30%; be mildly annoyed, 6%; be very annoyed, 2%). During informal discussion with providers at both clinics most stated that the survey did not interfere with clinic flow and allowed patients to use the wait time constructively. Providers felt these were important issues for patients to receive help. Social Problems: Eighty percent of families experience one or more health-related social problems; 34% one domain, 26% two domains, 20% three or more domains. Twenty seven percent of families experienced problems with access to health care; including 23% of parents without health insurance and 11% of children without health insurance. 56% of families identified housing problems; 43% reported one or more major household problems as defined by the American Housing Survey, 15% were either homeless or doubled up, and 8% had their utilities shut off in the past year. 39% of families experienced problems with food security as assessed by the Community Childhood Hunger Identification Project 8 question scale; 28% of families were defined as food insecure and 11% as hungry. 17% of families had income insecurity as defined by the primary provider out of work and looking for a job. 15% of mothers (n=178, 92% of participants) experienced domestic violence; 13% experienced verbal domestic violence and 8% physical domestic violence. Conclusions: Families of young children are significantly burdened by health-related social problems. The Online Advocate allows families to self-assess and identify these problems within the context of a primary care visit. The Online Advocate model demonstrated a high level of usability and acceptability among participants. Implications for Policy, Delivery or Practice: The pediatric office has the potential to assess, refer, and help families with social problems that impede the proper health and development of their children. A computer-based tool takes full advantage of emerging technologies to make the identification of social problems efficient and realistic given the cadence of clinical practice. Primary Funding Source: AHRQ • Keeping Asthmatic Children Out of Hospitals: Parents' and Physicians' Perspectives on How Pediatric Asthma Hospitalizations Can Be Prevented Glenn Flores, M.D., Milagros Abreu, M.D., Sandra Tomany, M.S., Johm Meurer, M.D., M.B.A. Presented by: Glenn Flores, M.D., Director, Community Outcomes; Associate Director, Center for the Advancement of Urban Children, Pediatrics, Medical College of Wisconsin/Children's Hospital of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: 414.456.4454; Fax: (414) 456-6385; E-mail: gflores@mail.mcw.edu Research Objective: 214,000 hospitalizations occur each year among the 6.3 million US children who have asthma. Not enough is known about how to prevent pediatric asthma hospitalizations. The goal of this study was to identify the proportion of preventable pediatric asthma hospitalizations and how such hospitalizations might be prevented, according to parents and physicians of hospitalized asthmatic children. Study Design: Cross-sectional survey of parents, primary care pediatricians (PCPs), and inpatient attending physicians (IAPs) of a consecutive series of all children admitted for asthma to an urban hospital in a 14-month period. Population Studied: Consecutive series of all children admitted for asthma to an urban hospital over a 14-month interval. The comparison group for bivariate analyses consisted of a consecutive series of all children admitted for other ambulatory-sensitive conditions to the same urban hospital over a 14-month period (N = 325). Principal Findings: The 235 hospitalized children had a mean age of 4 years; most were poor (mean annual family income = $14,795), non-white (91%), and had public (74%) or no (14%) health insurance. Compared with children hospitalized for other ambulatory-sensitive conditions, hospitalized asthmatic children were significantly more likely to be African-American (70% vs. 57%; P = 0.02), older (mean age = 4.4 vs. 3.3 years old; P < 0.001), and to not have made a physician visit or phone contact prior to admission (52% vs. 41%; P = 0.008). Only 26% of parents said that their child's admission was avoidable, compared with 36% of PCPs and 43% of IAPs. The proportion of asthma hospitalizations assessed as preventable varied according to the source or combination of sources, from 17% for agreement among all three sources to 52% as identified by any one of the 3 sources. PCPs (81%) and IAPs (71%) significantly more often (P < 0.001) than parents (39%) cited parent/patient-related reasons for how hospitalizations could have been avoided, including adhering to and refilling medications, better outpatient follow-up, and avoiding known disease triggers. Parents (28%) and IAPs (28%) significantly more often (P < 0.008) than PCPs (10%) cited physicianrelated reasons for how hospitalizations could have been avoided, including better education by physicians about the child's condition, and better quality of care. Multivariate analyses revealed that an age > 10 years, finding medical care to be too expensive, no physician contact prior to the hospitalization, working poor family income, and having no health insurance were associated with approximately 2-9 times the odds of a preventable asthma hospitalization. Conclusions: The proportion of asthma hospitalizations assessed as preventable varies from 17-52%, depending on the source making the assessment. Adolescents, families who find care to be too expensive, families who fail to contact physicians prior to hospitalization, children from working-poor families, and uninsured children are at greatest risk for preventable hospitalizations. Implications for Policy, Delivery or Practice: Many pediatric asthma hospitalizations might be prevented if parents and children were better educated about the child’s condition, medications, the need for follow-up care, and the importance of avoiding known disease triggers. Primary Funding Source: RWJF, Agency for Healthcare Research and Quality • Engaging Parents in Decision Making Shirley Girouard, Ph.D., R.N., FAAN Presented by: Shirley Girouard, Ph.D., R.N., FAAN, Associate Professor, Nursing, Southern Connecticut State University, P.O. Box 2458, Branford, CT 06405; Tel: 203.488.5135; Fax: (203) 488-5165; E-mail: sgirouard@aol.com Research Objective: To evaluate the impact of a civics training program on parental engagement in the community and to assess knowledge and skills related to democracy benchmarks. As the nation and states struggle with budget deficits and resource allocations and with the increasing demand for public accountability, society’s ability to meet the needs of children is compromised. Given the vulnerability of children, their dependence on parents and other adults to speak for them and the necessity of providing children’s services that will assure healthy and productive adults of the future, programs and policies are needed to assure positive outcomes. Parents, especially in the public arena, are an underutilized resource for developing, implementing and assessing programs and policies to positively affect the health, education and overall well-being of children. This paper describes an innovative program of the Connecticut Commission on Children aimed at enhancing parental involvement through democracy and civic skills training and provides the results of an evaluation of one program component. Study Design: A descriptive study design assessed the foci and outcomes associated with the community projects of the civics training program participants. All projects conducted over a three-year period (N=333) in 13 communities in one state were analyzed using content analysis and descriptive statistics. Population Studied: Parents who developed and implemented the 333 community projects represented diverse social, economic, ethnic and racial groups. Principal Findings: Of the 333 projects, 40% addressed early childcare or educational issues; 19%, health and health care issues; and 13%, safety concerns. Remaining projects reflected skill development and personal growth in civic skills. The projects met one or more of the democracy benchmarks: all demonstrated knowledge about and skill in democratic participation. A number of projects focused on specific democracy benchmarks: 17% addressed social or economic growth issues; 19%, tolerance of diversity; and 14%, promotion of shared values and the public good. Conclusions: The civic training program provided parents with knowledge and skills in civics and democracy that were translated into community activities and programs to enhance child health, education and safety. In addition, parents used their knowledge and skills to influence decision making by others, including policy makers at the community and state levels, to benefit children. Implications for Policy, Delivery or Practice: When parents have knowledge and skills to affect the public domain of decision-making about children’s issues, they contribute significantly to better programs and policy. By providing opportunities for parents to enhance their civic training, this important constituency can bring about needed and appropriate change. Providers, educators, public officials, researchers and others should engage parents to improve children’s present and future health and well being. Primary Funding Source: State funding • Impact of State Children’s Health Insurance Program (SCHIP) on Children’s Access to Primary Care in South Carolina: A Study of Hospitalizations with Ambulatory Care Sensitive Conditions (ACSC) Whiejong Han, Ph.D. Presented by: Whiejong Han, Ph.D., Research Assistant Professor, Health Services Policy and Management, University of South Carolina, Arnold School of Public Health, Columbia, SC 29208; Tel: 803.777.3460; Fax: (803) 777-1836; E-mail: hanwj@gwm.sc.edu Research Objective: The purpose of this study was to evaluate the effect of State Children’s Health Insurance Program (SCHIP) on children’s health in South Carolina as measured by the incidence of hospitalizations with Ambulatory Care Sensitive Conditions (ACSC). Study Design: To compare rates of ACSC admissions before and after SCHIP, longitudinal and cross-sectional hospital discharge data were used. This encounter-level data was linked with Medicaid data to identify the children enrolled in SCHIP. For multivariate analysis logistic regression was applied to find out likelihood of being hospitalized for ACSC. Study also used Generalized Estimating Equations (GEE) with a negative binomial model to investigate differences in rates of ACSC admissions across time. Population Studied: Population of this study included children (ages 0 to 18) in South Carolina who experienced a hospital admission during the period of 1995 ~ 2001. Principal Findings: During the study period 269,403 hospital admissions were detected from children aged 0 to 18 years old. Of those, 77,339 (28.7%) were with ACSC. After controlling other variables children under Medicaid had a lower probability to be hospitalized with ACSC, while younger children, male, African-American children, or children living in rural and very-rural areas had higher probability for ACSC admissions. Having community health centers in county was negatively related to the proportion of ACSC admissions. Number of primary care physicians per 10,000 children had significant association with ACSC admission but the effect was a minimal. Although the number of uninsured children declined after SCHIP introduced, no program effect was found on rates of ACSC over time. During study period, bacterial pneumonia, asthma and dehydration were most prevalent pediatric ACSC in South Carolina. Conclusions: The results detected no significant changes in ACSC admissions after SCHIP introduced. This study, however, confirmed that race, insurance status, and children’s residence are strong predictors for ACSC hospitalizations. Followings can be mentioned as possible explanations for the absence of positive findings in rates of ACSC over time. First, this study examined only four years of data after program implementation. Some new initiatives, however, take a while to be effective. Secondly, those who first enrolled in the program could have relatively poor health status because they were mostly uninsured previously. Study with more years of data could show different results on preventable hospitalizations. Implications for Policy, Delivery or Practice: Since certain population (eg., younger children, children in rural area) were more likely to have an ACSC admission, population-specific insurance eligibility might help to reduce ACSC admission rates. Allocation of SCHIP funding to counties with more target population, community-based initiatives for areas with higher ACSC rates, extend after-hour care for those areas could be other ways to improve children’s health. Finally, hospital discharge data provides an efficient way to analyze trends of preventable hospitalizations, and analyzing this trend can be a strong predictor of impact of SCHIP. Therefore, continuous study with extended data is suggested to keep policy makers informed on this issue. • The Role of Medicaid, SCHIP, and Other Public Sectors in the Financing of Children's Mental Health Services Embry Howell, M.S.P.H., Ph.D. Presented by: Embry Howell, M.S.P.H., Ph.D., Principal Research Associate, Health Policy Center, The Urban Institute, 2100 M Street, N.W., Washington, DC 20037; Tel: 202.261.5714; Fax: 202-223-1149; E-mail: ehowell@ui.urban.org Research Objective: To identify the financing streams for children's mental health services and the roles of each sector. To describe how the various sectors interact to fund services, and how those roles are changing over time. To provide new data on the prevalence of mental health conditions and use of mental health services by income and insurance status. Study Design: Three types of information were used in this study. We performed a comprehensive review of the literature on the topic; we interviewed 38 knowledgeable key informants around the country; and we analyzed new data from the National Survey of America's Families. Population Studied: Low income children with mental health problems. Principal Findings: Medicaid is a very prominent funder of children's mental health services and its role is growing. SCHIP is not yet a very prominent funder, but it provides relatively generous coverage compared to the private sector, and its role is also growing. The role of other sectors is also very important (public mental health agencies, education, child welfare, and juvenile justice), but there is a need for coordination across sectors. There are new collaborations evolving to blend funding and coordinate services that serve as models. Low income children have higher rates of mental health problems than non-poor children, and they have similar rates of use of mental health services. Uninsured children with mental health problems have much lower rates of use than Medicaid/SCHIP children. Conclusions: Medicaid and SCHIP funding of mental health services provide important access to mental health services for low income children, and their roles are increasing. There is a need for greater coordination across the various sectors involved in providing and funding such services. Implications for Policy, Delivery or Practice: For the benefit of low-income children, Medicaid/SCHIP agencies should play increased roles in monitoring the quality and cost of the mental health services that are provided under their programs. Primary Funding Source: RWJF • The Direct Medical Cost of Diabetes in Children Kumiko Imai, Ph.D., Ping Zhang, Ph.D., Giuseppina Imperatore, M.D. Presented by: Kumiko Imai, Ph.D., Centers for Disease Control and Prevention, 4770 Buford Highway, MS K-10, Atlanta, GA 30341; Tel: 770.488.4876; Fax: (770)488-5966; Email: kimai@cdc.gov Research Objective: To estimate the excess direct medical cost of diabetes in children and to demonstrate a use of an administrative claims database in analyzing children's health care utilization. Study Design: We used a large commercial administrative claims database for 1999, 2000 and 2001. Total direct medical costs were calculated using inpatient, outpatient, and pharmaceutical claims for more than 740,000 children, and were fitted by a modified two-part model that controlled for age, sex, and other factors specific to each family. The first part of the two-part model used a logit model that estimated the likelihood of incurring any medical costs, while the second part of the model was based on a generalized linear model that predicted the amount of medical costs for children who had positive costs. Inclusion of family random effects allowed us to control for unobservable factors shared by siblings. Population Studied: Claims and enrollment data came from 737,561-914,372 children aged 0-19 who were enrolled in a variety of employer-sponsored insurance plans in 1999, 2000 and 2001. For those, 2,266-3,755 children were identified as diabetic. Principal Findings: Compared to children without diabetes, children with diabetes on average spent an excess of $2,500 if they were not on insulin and $4,000 if they were on insulin. Outpatient services accounted for about half of total expenditures for non-insulin treated diabetic children, while drugs accounted for about a quarter for insulin-treated diabetic children. Also, estimates from the three years showed that the medical cost of diabetes in children grew considerably during the period. Conclusions: The cost of diabetes during childhood is substantial. Implications for Policy, Delivery or Practice: Considering the large economic burden of diabetes during childhood, more research is needed to find ways to prevent the disease in younger populations. Also, large administrative claims databases might be a useful source of information for researchers analyzing children's health care utilization and its trends over time. • Association of Having a Personal Physician with Quality of Care for CSHCN Moira Inkelas, Ph.D., M.P.H., Kandyce Larson, M.S.W., Kathryn Smith, M.A., M.S.N., Paul Newacheck, Dr.PH Presented by: Moira Inkelas, Ph.D., M.P.H., Assistant Professor, Health Services, UCLA School of Public Health, 1100 Glendon Avenue, Suite 850, Los Angeles, CA 90024; Tel: 310.794.0966; Fax: (310) 794-2728; E-mail: minkelas@ucla.edu Research Objective: Determine what percentage of children with special health care needs have a usual place for care and/or personal health care provider, and if report of these relationships is associated with sociodemographic factors, health insurance, and experiences with care when adjusting for condition severity. Study Design: Data are from National Survey of Children with Special Health Care Needs, a 2001 nationally representative telephone survey conducted by the National Center for Health Statistics providing national and state-based estimates. In addition to prevalence of usual place and of personal physician, a provider continuity measure is constructed with categories of: 1-having both a usual place for health care, and a provider (doctor or nurse) who knows the child best, 2-usual place but no personal provider, 3-personal provider but no usual place; and 4-no usual place or personal provider. 95 percent of parents reporting a personal provider say it is a physician. Family-centered care - FCC - is the 5 item FACCT measure on a 0-100 scale. Bivariate and multivariate analyses are used. Population Studied: Parents of 38,866 children with a chronic health condition that has lasted or is expected to last at least one year. Principal Findings: About 10 percent of CSHCN have no usual place for care and another 9 percent have a usual place but receive sick care and routine preventive care from different places. Parents of 11 percent of CSHCN report that no single provider knows the child best. The provider continuity measure shows that more uninsured and publicly-insured than privately insured children have a usual place but lack a personal physician. In logistic regression controlling for child age, condition severity, and total visits in the past year, odds of having a personal physician are lower for children who are uninsured OR 0.38, CI 0.31-0.48, publicly insured OR 0.73, CI 0.61-0.86, Latino with Spanish-speaking parent OR 0.54, CI 0.36-0.82, and whose mother has lower educational attainment. In multivariate OLS using these same control variables, compared to children with both a usual place and personal provider, FCC is similar for those with no usual place who have a personal physician b= -0.55, p=0.48, but lower for those with a usual place but no personal provider b= -11.9, p<0.001 and those with no usual place or a personal provider b= -16.2, p<0.001. Conclusions: Although causality in the association and all reasons for variability in physician relationship among CSHCN are not known, having a single physician whom the family counts on for information and coordination appears to improve access and parent-provider communication for CSHCN. Having only a usual source confers little benefit. Implications for Policy, Delivery or Practice: CSHCN may receive care from one or more specialists in addition to a primary care physician. Even with multiple providers, having a physician who knows the child best - whether a specialist or PCP - may lead to better coordination of care and quality of physician-parent communication. Ascertaining if parents feel they lack this relationship may enable the specialist or primary care physician to help the family determine where the medical home should be. Primary Funding Source: California Healthcare Foundation • Medicaid Enrollment and Utilization In Cuyahoga County: Evaluating the Early Childhood Initiative Amid Other Health Systems Changes Siran Koroukian, Ph.D., M.S.N., M.H.A., Engel Polousky, M.S., Rob Fischer, Ph.D., Claudia Coulton, Ph.D. Presented by: Siran Koroukian, Ph.D., M.S.N., M.H.A., Assistant Professor, Epidemiology and Biostatistics, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106-4945; Tel: 216.368.3197; Fax: 216-368-3970; E-mail: sxk15@case.edu Research Objective: A primary goal of the Cuyahoga County Early Childhood Initiative (ECI) is to facilitate early and sustained enrollment in Medicaid, which in turn is likely to promote receipt of timely and adequate amount of preventive services, through increased access to health services. Due to a coincidence in timing of the expansion of Medicaid managed care programs (MCPs) and the State Child Health Insurance Program (SCHIP) with that of the ECI, it was necessary to evaluate the performance of the ECI independently from that of MCPs or the SCHIP – programs with goals consistent with that of the ECI. The objective of this study was to compare outcome measures across counties with similar expansions in MCPs. Study Design: Ohio Medicaid enrollment and claims history files for 1998-2001, encompassing fee-for-service claims and managed care encounter data, were used to obtain the relevant measures. These measures included age at first enrollment in Medicaid; length of enrollment in Medicaid; as well as the timing and number of comprehensive preventive visits (CPVs) in the first 15 months of life. Multivariable survival analysis and logistic regression analyses were employed to assess the effects of residence in Cuyahoga County, as an indicator for having been exposed to ECI, independently from the effects of the expansion of MCPs, or the SCHIP, relative to the measures of interest, and to control for differences in demographic profile across the counties. Adjusted hazard ratios (HRs) and odds ratios (ORs) were derived respectively from multivariable survival and logistic regression analyses. Population Studied: Children enrolled in Ohio Medicaid during 1998-2001, and residing in seven large urban counties with mandatory managed care programs. Principal Findings: The study population included approximately 140,000 children 6 years of age or younger. The measures were comparable across the counties, and followed the same trends of improvement over time. A small, but statistically significant advantage was observed in these measures relative to Cuyahoga County. In particular, Cuyahoga children were significantly more likely than others to enroll early in Medicaid and have sustained enrollment in the program (HR of 1.02 and 0.88, respectively, p < 0.01 for each comparison). Relative to the receipt of CPVs, Cuyahoga children were significantly less likely not to have received any CPV, or less than 4 visits during the first 15 months of life (OR of 0.76 and 0.88 respectively, p < 0.01 for each comparison). They were more likely than others to receive at least 5 CPVs in the first year of life – the recommended number of preventive visits by the American Academy of Pediatrics (OR=1.11, p < 0.01). Conclusions: The findings reflect favorably upon the ECI, and support the notion that the ECI may have yielded modest benefits above and beyond the effect of MCPs or the SCHIP program. Additional analyses on programmatic details and the logistics entailed in accessing and using Medicaid and health services may help identify factors that could further improve the relevant outcomes. Implications for Policy, Delivery or Practice: The provision of additional services at the community level seems to enhance the existing synergy yielded by the expansion of MCPs and SCHIP, two programs with goals similar to that of the ECI. Primary Funding Source: Cuyahoga County • Feasibility of Influenza Immunization for Children 6-23 Months in the Inner-City Chyongchiou Lin, Ph.D., Richard Zimmerman, M.D., M.P.H., Mary Patricia Nowalk, Ph.D., RD, Alejandro Hoberman, M.D., David Greenberg, M.D., Stuart Weinberg, M.D. Presented by: Chyongchiou Lin, Ph.D., Assistant Professor, Health Policy and Management, University of Pittsburgh, A613 Crabtree Hall, 130 DeSoto Street, Pittsburgh, PA 15261; Tel: 412.624.3625; Fax: 412-624-3146; E-mail: cjlin@pitt.edu Research Objective: Determine the feasibility of vaccinating typically hard-to-reach, low-income children against influenza, and assess its effect on timely receipt of other vaccines. Study Design: Before/after trial with the health care center as the unit of intervention in three types of settings: pediatric residency, family practice residencies and faith-based practices, at ten offices in low-income urban locations. Population Studied: Children aged 6-23 months, during the 2002-2003 influenza season, were selected for intervention. The comparison group for analysis was children who were in the same age range in the previous influenza (2001-2002) season and were active patients of the practice, that is, they had been seen in the office in the last 6 months. Active patients born between October 1, 2000 and April 1, 2002 were the 2002-2003 intervention group (n = 1,534) and children born between October 1, 1999 and April 1, 2001 comprised the pre-intervention comparison group (n = 1,210). Principal Findings: Immunization rates of the two-dose influenza vaccine improved significantly at all three types of health care centers. Compared with the pre-intervention season, vaccination rates for the first dose during the intervention season significantly increased from 7.6% to 42.3% at pediatric residency offices, from 4.3% to 15.6% at family practice residencies; and from 4.3% to 47% at faithbased practices (P<0.001). Rates for the second dose were significantly improved over pre-intervention, but lower than first dose rates (P<0.001). Average ages at vaccination for other recommended childhood vaccines did not differ or were significantly younger (MMR and varicella) for children who received influenza vaccine vs. those who did not. Moreover, a higher percentage of influenza-vaccinated than unvaccinated children received their MMR, DTaP 3, IPV 2 and Hib 2 vaccines within a two-month grace period of the recommended age (P<0.05), with no change in the timing of receipt of varicella, DTaP 1, IPV 1 and Hib 1. Conclusions: With directed effort, it is possible to increase influenza vaccination at health care centers serving lowincome children. The addition of a two-dose vaccine does not delay receipt of other vaccines. Implications for Policy, Delivery or Practice: Our findings, presented to the Advisory Committee on Immunization Practices (ACIP), provided a basis for full recommendation of the influenza vaccine for all 6-23 month old children, beginning in 2004. Primary Funding Source: CDC, the Association of Teachers of Preventive Medicine (ATPM) • Effects of Maternal Characteristics on Cesarean Delivery Rates among U.S. Department of Defense Healthcare Beneficiaries, 1996 - 2002 Andrea Linton, Ph.D., Michael Peterson, Dr.P.H., Thomas Williams, Ph.D. Presented by: Andrea Linton, Ph.D., Senior Health Program Analyst, TRICARE Management Activity, Dept. of Defense, 5111 Leesburg Pike, Falls Church, VA 22041; Tel: 703.681.3636; Email: andrea.linton@tma.osd.mil Research Objective: To identify rates of cesarean birth for the Military Health System (MHS) healthcare beneficiary population from 1996 to 2002 and compare those rates to the national experience. We also sought to identify non-clinical factors associated with cesarean delivery including maternal age, race, socioeconomic status, and insurance coverage. Study Design: Hospital discharge and claims records for babies born in the military and civilian hospitals that comprise the Military Health System (MHS) healthcare network were used to calculate total and primary cesarean rates and vaginal birth after cesarean (VBAC) rates from 1996 to 2002. Annual cesarean rates for subgroups defined by maternal age, race, and socioeconomic status were calculated to examine rate variations and rate trends within the study population. Pooled data from 1999 to 2002 were used to compare rates across socioeconomic status, stratified by age and race. Population Studied: Beneficiaries who had a childbirth experience at any one of the military and civilian hospitals within the MHS between 1996 and 2002. Principal Findings: Total and primary cesarean rates among the MHS population were lower than those reported nationally for every year examined. The cesarean and VBAC rate trends in the national and MHS populations were similar. Within the MHS population, total cesarean delivery increased with increasing maternal age and was more highly associated with racial minorities relative to white women. The higher socioeconomic subgroup (defined as active duty, retired, and warrant officers, and their families in this study) was generally associated with reduced cesarean section rates. Conclusions: Cesarean deliveries are performed less frequently for the MHS healthcare beneficiary population, relative to the national population. Associations between socioeconomic factors and cesarean rates reported for the national population were not apparent in the study population. The consistent pattern of rate variation across racial subgroups in the MHS population suggests that factors beyond those examined in this study are needed to explain the elevated cesarean rates for racial minorities. Implications for Policy, Delivery or Practice: The historically lower cesarean rates and higher VBAC rates in the DoD suggest that further studies of DoD healthcare practice patterns, institutional culture, and outcomes may offer insights for developing interventions to slow the increase in cesarean use and ultimately reverse a three decade-long trend without compromising maternal or fetal health. Primary Funding Source: Dept. of Defense • The Economic Impact of Persistent Pulmonary Hypertension of the Newborn (PPHN): Use of the KID Database for a Common Neonatal Disease Scott Lorch, M.D., MSCE, Joel Portnoy, M.D. Presented by: Scott Lorch, M.D., MSCE, Neonatologist, Neonatology and Center for Outcomes Research, The Children's Hospital of Philadelphia, 3535 Market Street, Suite 1029, Philadelphia, PA 19104; Tel: 215.590.1714; Fax: (215) 5902378; E-mail: lorch@email.chop.edu Research Objective: Much of the epidemiologic data on PPHN has come from randomized controlled trials, which may not demonstrate the societal impact of the disease. Administrative databases would allow for such populationbased studies, but only include codes for comorbidities and thus do not capture clinical data, such as the use of inhaled nitric oxide. Because of this fact, neonatal diseases have not been studied using asuch dministrative databases. The objective of this study is to (1) determine national estimates of total charges and length of stay for infants with PPHN; and (2) to develop prediction models for death, need for extracorporeal membrane oxygenation rescue treatment (ECMO), and length of stay (LOS) in infants with PPHN, and to validate these results with models using clinical data. Study Design: Infants <14 d of age with an ICD-9 code for PPHN (416.0 or 747.89) were identified using the 2000 KIDS database, an 80% stratified random-sample of pediatric hospitalizations in 27 states. 1 cohort required an ICD-9 code for meconium aspiration, pulmonary hypoplasia, asphyxia, pneumonia, or sepsis, and a second included all infants except those with an ICD-9 code for complex congenital heart disease, diaphragmatic hernia, or birth weight <1750g. A third cohort included all infants transferred to CHOP with PPHN between 1996 and 2001 (N=91). Patient-weighted, stratumspecific methods estimated total hospital charges, ECMO use, LOS, and mortality. Logistic and linear regression models determined the effect of demographic and comorbid conditions on LOS and total charge for all three cohorts and were validated using bootstrap methods. Population Studied: Infants <14 d of age with an ICD-9 code for PPHN (416.0 or 747.89) in the 2000 KIDS database. Principal Findings: Using the narrow cohort, there were an estimated 7149 infants treated with PPHN in the US in the year 2000 (95% CI 6525-7773), with an average LOS of 12 days (95% CI 11.4-12.6). 42% were female, 5.1% required ECMO (95% CI 3.4%-6.7%), and 4.9% died (95% CI 4.0%-5.9%). 69.7% were treated in teaching hospitals. Their estimated hospital charge was $378.2 million (95% CI $325 million-$432 million). Similar results were seen using the broad cohort. Predictive models using either administrative cohort had excellent predictions for risk of death (c-statistic 0.86, 95% CI .83-.89) and need for ECMO (c-statistic 0.87, 95% CI .85-.9), but weaker validity for LOS (r2=.27, 95% CI .25-.3). Clinical data improved the predictive validity only for the LOS model (r2=.6) by including a major determinant of LOS, total days on oxygen, which cannot be ascertained in administrative datasets. Higher number of days on oxygen predicted fewer residual hospital days prior to discharge. Conclusions: PPHN has substantial economic costs. ECMO use and mortality rates are lower than previously published rates. Administrative databases allow for the development of strong predictive models for death or need for ECMO, but detailed clinical data are needed for adequate LOS predictions, especially length of oxygen administration. Implications for Policy, Delivery or Practice: Administrative databases allow for population-based studies of neonatal diseases. Understanding the factors leading to more days on oxygen could aid in reducing the economic burden of PPHN. Primary Funding Source: AHRQ • Planning for Medical Transitions for Adolescents with Special Health Care Needs Debra Lotstein, M.D., Moira Inkelas, Ph.D., Kandyce Larson, M.S.W., Neal Halfon, M.D., M.P.H. Presented by: Debra Lotstein, M.D., Research Fellow, Robert Wood Johnson Clinical Scholars Program, UCLA, 911 Broxton, 3rd Floor, Los Angeles, CA 90024; Tel: 310.794.0612; E-mail: lotstein@ucla.edu Research Objective: There is growing consensus that adolescents with special health care needs should eventually transition to adult-oriented health systems. Transition planning has been suggested as a way to ease the process of transition for chronically ill adolescents and to ensure that teens are assisted with age-related changes in medical care, insurance coverage and independent living. The objectives of this study were: 1) to estimate the proportion of teens with special health care needs receiving transition assistance from health care providers, and 2) to assess the factors associated with receiving transition assistance. Study Design: Analysis of a nationally-representative, random digit dial telephone survey of parents of youth with special health care needs. Dependent variables measuring transition assistance were (1) general discussion of changing needs in adulthood (“transition discussion”), and (2) transition discussion plus more specific planning for future needs (“transition planning”). We carried out bivariate and multivariate analyses to identify predictors of transition discussion and planning. Population Studied: Parents of 5,555 adolescents aged 13-17 with at least one chronic condition included in the National Survey of Children with Special Health Care Needs (conducted by the National Center for Health Statistics in 2000-2002). Principal Findings: 50% of parents reported having transition discussions with their child’s physicians and fewer (34%) reported receiving transition planning. Logistic regression models with social, disease severity and medical care process variables were performed, first for transition discussion and secondly for transition planning. Hispanic teens had lower odds than whites of discussing transition (OR=0.47, 95% CI 0.29-0.76). Adolescents with more than 10 physician visits in the last year were more likely to discuss transition (OR=1.69, CI 1.31-2.17) as were those with more family-centered communication (OR=2.10, CI 1.71-2.57). Age of the adolescent was not associated with transition discussion. Odds of transition planning were higher for teens with more visits (OR=1.91, CI 1.45-2.51) and for those with better ratings of communication (OR=2.21, CI 1.77-2.74). Older teens were more likely than younger teens to have received transition planning from their pediatric provider (17 year olds vs. 13-16 year olds, OR 1.61, CI 1.24-2.08). Conclusions: Most adolescents with chronic health conditions are not receiving the transition assistance that guidelines suggest is needed, and some racial/ethnic disparities are evident. Even among 17 year olds, planning rates are low. Those with a large number of provider contacts have greater odds of receiving transition assistance. Transition discussion and planning are associated with the quality of provider-patient communication Implications for Policy, Delivery or Practice: Efforts to increase the number of youth receiving transition planning might effectively be linked with strategies to improve familyprovider communication. Further research is needed to understand 1) the ways that patient characteristics shape transition needs and 2) which forms of transition assistance are most helpful in improving adult outcomes for young adults with chronic conditions. Primary Funding Source: RWJF • An Evaluation of the Accountability and Quality of Managed Care for Medicaid and SCHIP Children: State Approaches to Monitoring and Enforcing Oral Health and Lead Screening Contractual Standards Sara Rosenbaum, J.D., Anne Markus, J.D., Ph.D., Colleen Sonosky, J.D., Lee Repasch, M.A., D. Richard Mauery, M.P.H. Presented by: Anne Markus, J.D., Ph.D., Assistant Research Professor, Health Policy, The George Washington University Medical Center, 2021 K Street, N.W., Suite 800, Washington, DC 20006; Tel: 202.530.2339; Fax: (202) 296-0025; E-mail: armarkus@gwu.edu Research Objective: To examine state experiences with monitoring and enforcing contractual standards of pediatric care imposed on managed care organizations (MCOs). Study Design: Review of Medicaid/SCHIP managed care contracts and semi-structured telephone interviews with Medicaid/SCHIP officials involved in contract oversight. Questions focused on the logic behind the selection of one high and one low prevalence condition (oral disease and lead poisoning) to emphasize in the contract, and the development of expectations regarding MCO performance in these two areas of child health and the monitoring of actual performance against those expectations. If a state was sufficiently concerned with a particular child health condition to address it with some specificity in the contract, it was expected to focus on it as part of its oversight efforts. A conceptual framework on key components of an effective state monitoring plan was used to guide the analysis and organize findings. Population Studied: 16 states with 27 Medicaid and separately-administered SCHIP full-risk managed care programs, representing more than half of the nation’s population, a broad range of fiscal capacity, child well-being, managed care markets, and approaches to government programs; 9 states—15 programs—participated (RR=56%). Principal Findings: Medicaid and SCHIP contractual provisions varied in specificity across/within states but generally addressed the service components and periodicity schedules of oral health and lead screening. Contractual standards differed between Medicaid and SCHIP because of different federal benefit requirements and state health needs. All states had a formal monitoring plan. All agencies collected data regularly to measure MCO compliance with quantifiable standards but few used quality benchmarks specific to oral health and lead screening. Many programs designed a graduated incentive and penalty system, believed to favor compliance. Most states, even those with high managed care penetration, approached enforcement more as collaboration with MCOs because of underlying systemic issues beyond state and MCO control. Conclusions: States play a significant role in ensuring pediatric quality and they adapt their quality improvement strategies to the conditions of local markets to achieve the best possible outcomes for children under the circumstances. States pay attention to the contract and generally perform some contract monitoring as one avenue to ensuring quality. They do not consider the contract as all encompassing on quality improvement because its reach falls short of addressing underlying systemic issues. Implications for Policy, Delivery or Practice: Findings have implications for Medicaid/SCHIP quality improvement. Legislation is broad in that regard and should remain broad so that states can tailor their approaches to what is happening at the local level. Because underlying systemic issues appear to lessen the influence of contract language and enforcement, states should be encouraged to turn to additional, noncontractual strategies, such as community awareness, to address these problems. Findings also have implications for children’s right to coverage under Medicaid and SCHIP, and for children with special health care needs whose higher prevalence in Medicaid and SCHIP warrants particular efforts on the part of states to monitor the quality of care they receive. Primary Funding Source: The David and Lucile Packard Foundation. • Translating Evaluation Research Into Practice: EvidenceBased Strategies to Enhance Service Delivery and Quality of Care to Vulnerable Children Maryam Navaie-Waliser, Dr.P.H., Laura Ensler, MS.E.d., Aubrey Spriggs, M.A., David Jones, C.S.W. Presented by: Maryam Navaie-Waliser, Dr.P.H., Senior Research Associate, Center for Home Care Policy and Research, Visiting Nurse Service of New York, 5 Penn Plaza, 11th Floor, New York, NY 10001; Tel: 212.609.5762; Fax: (212) 290-3756; E-mail: maryam.navaie@vnsny.org Research Objective: Although evaluation research in health settings aims to improve understanding of care processes and outcomes, successfully translating results into practice to enhance service delivery and quality of care remains a challenge to many professionals. This study will present evidence-based strategies that demonstrate multiple pathways of using research data to impact practice to enhance service delivery and quality of care to vulnerable children within homeand-community-based health settings. Study Design: A prospective cohort study was begun in 20022003 with participants in an Early Head Start (EHS) program of a large, urban home health agency targeting adolescent/young parents and their children. Trained staff performed interviews and observational assessments around the time of admission and every 4 to 6 months thereafter for follow-up using standardized, reliable, and validated instruments to capture multiple health and social outcomes. Outcomes data were linked with service utilization and administrative data for comparative assessments and analytic purposes. Population Studied: Children between ages 0 to 3 years (n = 101) and their parents (n = 99 mothers and 70 fathers) served by an EHS program of a large, urban home health agency in 2002-2003. Over 90% of children were African-Americans or Hispanics living in poverty. Principal Findings: Process and outcome measures revealed: (a) a need for more timely charting and comprehensive documentation, (b) high levels of need among families of infants/toddlers in understanding child development, building self esteem, managing depression and stress, developing parenting competence and skills, reducing anxieties surrounding attachment issues, reducing social isolation, and engaging in community building and civic activities; and (c) an increased need among children for preventive health care and use of standardized child developmental assessments. Translating these findings into constructive and meaningful practice changes was achieved by administrators and practitioners using three key strategies: (a) conducting rigorous staff development to better prepare practitioners through knowledge and skill enhancements by training, reflective supervision, and enhanced in-service education; (b) tailoring and prioritizing home-based and center-based health and social services to reflect needs through implementation of multidimensional individualized care plans; (c) performing thorough quality assurance monitoring through various enhancements of administrative processes; and (d) adoption of age-appropriate, standardized child developmental evaluation tools. To date, follow-up data have been promising, suggesting that evaluation research results have been successfully incorporated into practice improvement initiatives as evidenced by program expansion, increased advocacy efforts, improved parent-child interactions, better child and parent outcomes, improvement in staff knowledge and readiness skills, and earlier identification and referral of children with special needs. Conclusions: Although there is no simple formula for translating research into practice, through collaborative efforts, creative strategies can be devised and employed incrementally to enhance service delivery and quality of care to vulnerable children and their families. Implications for Policy, Delivery or Practice: Within homeand-community-based health settings, researchers, administrators, and front-line practitioners can maximize research applications to practice. Short-term and long-term implications of the study will be discussed, emphasizing use of multiple data sources to establish priorities, identifying and targeting service delivery, and monitoring improvements in care processes and outcomes. • Utilization of Intracranial Pressure Monitors in Critically Ill Children with Meningitis Fola Odetola, M.D., John Tilford, Ph.D., Matthew Davis, M.D., MAPP Presented by: Fola Odetola, M.D., Clinical Instructor, Department of Pediatrics and Communicable Diseases, University of Michigan, F6884 mott/0243, 1500 East Medical Center Drive, Ann Arbor, MI 48103; Tel: 734.615.8418; Fax: 734.615.5153; E-mail: fodetola@med.umich.edu Research Objective: To describe patient- and hospital-level factors associated with the use of Intracranial pressure monitors (ICPM) in critically ill children with meningitis. Study Design: A retrospective cohort study of hospitalizations for meningitis requiring mechanical ventilation was conducted using the Kids’ Inpatient Database (KID). The KID includes over 2 million pediatric discharge records obtained from 22 states in 1997 and 27 states in 2000, drawn from the 4 major US census regions. Records were weighted to obtain national estimates of meningitis hospitalizations and ICPM use. ICPM cases were identified using ICD-9 procedure codes. Meningitis was defined using ICD-9 codes for a primary or secondary diagnosis of meningitis. Hospitalizations with ICD-9 codes for traumatic brain injury or ventriculo-peritoneal shunts were excluded, as were pre-transfer hospitalizations. Using data pooled from 1997 and 2000, bivariate comparisons of factors related to ICPM use were performed, and multivariate logistic regression models were fit to determine which factors were independently associated with ICPM use. Population Studied: Hospitalizations for meningitis requiring mechanical ventilation,in children 0-18 years old in 22 states in 1997 and 27 states in 2000. Principal Findings: There were an estimated 1067 and 1170 hospitalizations for childhood meningitis requiring mechanical ventilation in 1997 and 2000, respectively. Most (79%) of the hospitalizations involved infants (<1 year old). There was no difference in the frequency of ICPM use by calendar year. In bivariate analyses, ICPM use differed by age (4% in infants, 14% in children 1-4 years old, 21% in children 5-18 years old; p<0.01) and by census region. There was no difference in ICPM use by gender, race, etiologic organism, median household income, primary payer, or hospital characteristics (rural/urban, teaching status, bed size). In multivariate analyses, increasing age in 1-year increments (OR 1.14, 95%CI 1.09-1.20) and living in the West (OR 2.59, 1.384.87) compared to other census regions were independently associated with ICPM use, while controlling for other factors. Conclusions: The findings indicate heretofore unrecognized variation in the use of ICPM for childhood meningitis by child age and by census region. Further study is warranted to examine the reasons for this variation and effects on clinical outcomes related to ICPM use. Implications for Policy, Delivery or Practice: No clear guidelines exist for the use of ICPM in children hospitalized for meningitis, neither have outcomes in these children been well described. Additional research incorporating these study findings, could improve the care of critically ill children with meningitis for whom ICPM is implemented. • Regionalization of Non-Cardiac Neonatal Surgery in California: Is it Geographically Feasible? Ciaran Phibbs, Ph.D., Roderic Phibbs, M.D., Susan Schmitt, M.S., Diana Farmer, M.D., Laurence Baker, Ph.D., Beate Danielsen, Ph.D. Presented by: Ciaran Phibbs, Ph.D., Research Economist, Health Economics Resource Center (152), VA Medical Center, 795 Willow Road, Menlo Park, CA 94025; Tel: 650.493.5000 Ext. 22813; Fax: (650) 617-2639; E-mail: cphibbs@stanford.edu Research Objective: While the association between surgical volume and mortality risk has been demonstrated for neonatal cardiac surgery, there have been no studies that look at this association for non-cardiac neonatal surgery, or at the feasibility of regionalizing these cases. The objectives of this study were to: - Look at where neonatal surgery was being performed. - See if it was geographically feasible to concentrate neonatal surgery in hospitals that perform high-volumes of these procedures. - See if the number of non-cardiac neonatal surgeries a hospital performs was associated with mortality for neonates who require major surgery. Study Design: California birth certificates for 1991-2000 were linked to death certificates, and hospital discharge data, including neonatal transfers. ICD-9 procedure codes were used to identify major non-cardiac surgical procedures. Descriptive data were summarized by NICU level of care and hospital surgical volume. Distance was measured using straight-line distance between hospitals. Data from the birth certificate and discharge abstracts were used to control for clinical risk factors in logistic regression models to examine the association between surgery volume and mortality risk. Population Studied: All births in California that 1991-2000 who underwent major non-cardiac surgery before they were discharge home. Principal Findings: A majority of the non-cardiac neonatal surgery was performed at tertiary centers that had high surgical volumes. In 1991 the 12 hospitals that performed at least 50 surgeries did a total of 948 (58%) of the 1638 surgeries performed in California. But, in 1991 there were 37 hospitals that performed less than 15 major non-cardiac surgical procedures on neonates, and an additional 21 hospitals that performed between 15 and 49 of these surgeries. These numbers were similar over the 1990s, except that there was a modest decline (21 to 16) in the number of hospitals with moderate surgery volumes. Most of the moderate surgery volume hospitals were State-certified to perform neonatal surgery (16 of 21 in 1991 and 16 of 16 in 2000). Only 5 of the 37 low-volume providers were certified to perform neonatal surgery in 1991. This increased to 17 of 38 in 2000. All of these moderate volume hospitals and virtually all of the low volume hospitals were located in major urban areas within reasonable geographic access to hospitals that had high surgical volumes. There was no significant volumeoutcome effect on mortality when all non-cardiac surgical cases were considered, but many of these procedures were for conditions not associated with high levels of mortality. The volume effect may be significant for higher-risk procedures, or for other measures of outcome. Conclusions: While 60% of non-cardiac neonatal surgery was performed in hospitals that were high-volume providers of pediatric surgery, there were relatively large numbers of hospitals that performed low volumes of neonatal surgery. All but 6 of the hospitals with low surgery volume were close to a high-volume provider. Implications for Policy, Delivery or Practice: Regionalizing non-cardiac neonatal surgery in California to high-volume providers is geographically feasible; virtually all of the surgery is already being performed at hospitals near a high-volume provider. Primary Funding Source: NICHD • Nationwide Estimates of the Use of Implantable Medical Devices in Children Joel Portnoy, M.D., Scott Lorch, M.D., MSCE, Chris Feudtner, M.D., Ph.D., M.P.H. Presented by: Joel Portnoy, M.D., Assistant Professor, Center for Outcomes Research, Department of Anesthesiology and Critical Care Medicine, Children's Hospital of Philadelphia, 3535 Market Street, Suite 1029, Philadelphia, PA 19104; Tel: 215.590.5758; Fax: 215-590-2378; E-mail: portnoy@email.chop.edu Research Objective: Implantable medical devices (IMDs) can have a substantial impact on the lifespan and quality of life of children with chronic diseases, yet little is known about the epidemiology of these devices in children. The aim of this study is to calculate national estimates of the frequency of placement of IMDs in children, describe characteristics of the associated hospital admissions, and test the hypothesis that the number of IMDs placed is increasing. Study Design: We conducted a descriptive study used the Kids Inpatient Database, a stratified random sample of pediatric discharges from non-federal community hospitals in 1997 and 2000. We identified cases by procedure codes corresponding to the placement of an IMD. National estimates of the number of devices implanted in patients less than 18 yrs old were obtained using survey estimation techniques, and the increase over time was tested using a ttest. Population Studied: Pediatric patients admitted to all nonfederal, short-term, general and other specialty hospitals in the years 1997 and 2000 Principal Findings: There were an estimated 503,653 (standard error 14,013) IMDs placed in pediatric inpatients during 1997 and 2000. The procedures were done mostly in large, urban, teaching hospitals; half were performed in children's hospitals. For an admission where a device was placed the average length of stay was 15.9 days, the average charge was $55,281, 4.5% of the patients died, 4.0% were transferred to long-term care, and 8.0% were discharged with home health care. Between 1997 and 2000 respectively there were significant increases in the total number of devices (222,224 vs. 281,429, p<.001), internal fixations (24,925 vs. 44,419, p<.001), gastrostomies (10,462 vs. 13,087, p=.011), spinal fusions (7,157 vs 11,418, p<.001), and skin grafts (221 vs. 476, p=.021). Conclusions: The number of IMDs placed in children in 1997 and 2000 was large and increasing. Prospective trials are needed to study the safety, efficacy, costs, and benefits of these devices in pediatric patients. Implications for Policy, Delivery or Practice: Because the population of children using implantable medical devices is large and growing, policymakers may need to reevaluate the steps required to bring an IMD to market for pediatric use. • Health Insurance and Children’s Reliance on Emergency Departments for Non-Urgent Care Mary Rimsza, M.D., William Johnson, Ph.D., Tricia Johnson, Ph.D. Presented by: Mary Rimsza, M.D., Director of Health, School of Health Administration & Policy, Arizona State University, Box 2104, Tempe, AZ 85287-2104; Tel: 480.965.1145; Fax: (480) 965-4605; E-mail: Mary.Rimsza@asu.edu Research Objective: This study uses micro-data from a unique community health data system to estimate the effect of insurance on emergency department use for non-urgent care, controlling for demographics, health care needs and accessibility. Study Design: Data from a unique community health information system are used to examine factors that affect access, including (a) predisposing characteristics, (b) characteristics that enable access, and (c) characteristics that represent a need for care. We estimate the probability of reliance on an emergency department using multivariate logit equations. Population Studied: Participants include children 0 to 19 years of age, living in a semi-rural border county in Arizona, who either used the emergency department or relied on primary care providers for routine, non-traumatic care in 1999. Principal Findings: Uninsured children were 7.7 times more likely to rely on the emergency department than insured children. The children most likely to rely on the emergency department were adolescents, Native-American, uninsured and those living in the city of Yuma. The majority of children whose usual source of care is the emergency department, in terms of numbers, were privately insured, ages 0 to 4, Latino, and living in the city of Yuma. Children insured by Medicaid were 90% less likely than privately insured children to rely on the emergency department as their usual source of non-urgent care. Conclusions: Providing health insurance for children living in the border counties will reduce, but not eliminate, reliance on the emergency department for care, since the majority of children who rely on the emergency department for care already have health insurance. The highest utilization rates are observed for Native American Children. Controlling for insurance status, Latino children are not more likely than White, non-Latinos to rely on emergency department care. Implications for Policy, Delivery or Practice: Reliance on the emergency department for routine care is more costly, less effective and less coordinated than care provided by a primary care provider. There is a widespread belief that expanding health insurance coverage for children will effectively end children’s reliance on emergency departments as the usual source of care for non-urgent conditions. This research suggests that health insurance coverage alone will not substantially reduce the numbers of children who inappropriately rely on emergency departments for care. The search for alternatives should include targeting children with characteristics that are associated with a high probability of reliance on the emergency department, weighted by the numbers of children with those characteristics. The ranking of interventions could then be evaluated by analyzing the probability of success for the interventions associated with each of the weighted targets. Primary Funding Source: The Flinn Foundation & Arizona State University • Children with Special Health Care Needs with Emotional, Developmental and/or Behavioral Needs: Barriers to Utilization Roberta Scheinmann, M.P.H., Gerry Fairbrother, Ph.D., Melinda Dutton, JD, Beth Osthimer, JD, Rachel Cooper, M.A. Presented by: Roberta Scheinmann, M.P.H., Research Associate, Division of Health and Science Policy, The New York Academy of Medicine, 1216 Fifth Avenue, New York, NY 10029; Tel: 718.788.3216; E-mail: rs536@hotmail.com Research Objective: To examine how Children with Special Health Care Needs (CSHCN) with emotional developmental and/or behavioral problems differ from other CSHCN and from children without special needs (non-CSHCN), in measures of their barriers to utilization of health services. Study Design: A cross-sectional random-digit dial survey of parents of publicly insured or uninsured children was conducted in New York City in 2002/2003. Questions about access to and use of medical care were asked about a focal child. Population Studied: Publicly insured and uninsured children in New York City Principal Findings: Of the 1172 respondents, 24% (n=266) identified their child as a CSHCN using a standard tool developed by FACCT. Of the 266 CSHCN children, 33% had an emotional, developmental or behavioral problem that was expected to last more than one year. Children with emotional, developmental or behavioral problems were more likely than other CSHCN and non-CSHCN to have seen a mental health professional in the past year [54% vs. 5% vs. 4%; p<.001] and were more likely to have delayed or gone without emotional developmental and behavioral care [18% vs. 2% vs. 2; p<.001]. Among the problems these children and their families face in getting care compared to the other CSHCN and non-CSHCN were cost of care [23% vs. 9 % vs. 8%; p=.01]; not knowing where to go for care [22% vs. 10% vs. 8%; p=.01]; not getting a referral or approval [25% vs. 13% vs. 7%; p<.01]; and transportation to care problems [25% vs. 14% vs. 7%]. Conclusions: Even after controlling for insurance status, CSHCN with emotional, developmental or behavioral problems, experience greater health access difficulties than other CSHCN and than children without special needs. Implications for Policy, Delivery or Practice: Outpatient mental health services need to be expanded or made more accessible in order to effectively link all CSHCN with care. Primary Funding Source: WT Grant and Altman Foundations • Measuring Health-Related Quality of Life (HRQOL) in Pediatric Cerebral Palsy: Hearing the Voices of Children Sandra Sherman, B.A., Tasha Burwinkle, Ph.D., Psy.D., James Varni, Ph.D., Kanela Hanna, B.A., Susan Berrin, B.A., Jason Miller, B.A. Presented by: Sandra Sherman, B.A., doctoral student, Motion Analysis Laboratory, SDSU/UCSD Joint Doctoral Program in Clinical Psychology, Children's Hospital of San Diego, 6363 Alvarado Court, Suite 103, San Diego, CA 92120; Tel: 858.455.1887; Fax: 619-594-6780; E-mail: ssherman@ucsd.edu Research Objective: Outcomes research has typically focused on physical measures, proclaiming them quantifiable and scientifically valid. Recently, a paradigm shift resultant in a holistic approach to healthcare emphasizes measurement of HRQOL, encompassing both physical and psychosocial domains. Due to cognitive deficits associated with pediatric CP, however, outcomes research using children’s selfperceptions of their HRQOL is limited. Furthermore, research has focused on physical functioning, as studies suggest only modest correlations between parent and child measures of internal states. We hypothesize that: (1) children with CP and their parents can reliably self and proxy-report HRQOL, (2) higher correlations between parent-proxy and child self-report on physical than psychosocial functioning; (3) CP patients will report lower HRQOL than a healthy sample; (4) greater disease severity will be associated with lower HRQOL scores. Study Design: The Pediatric Quality of Life Inventory™ (PedsQL™) 4.0 Generic Core Scales, which generates a total score and two main subscales: physical and psychosocial (comprised of emotional, social, and school functioning), was administered to 60 CP patients (5-18) and 183 parents of patients (2-18). Internal consistency reliability coefficient alphas for child and parent reports were determined for group comparisons, and correlations between parent-proxy and child reports were calculated. ANOVAs to determine the relationship between disease severity and HRQOL, and t-tests for independent samples to compare CP patients with a healthy sample (401 children, 718 parents) were performed. Population Studied: CP patients and their parents Principal Findings: Internal consistency reliability alpha coefficients for total, physical, and psychosocial functioning were: child = .84, .76, .77; parent = .90, .89, .85. Correlations between parent and child reports were higher for physical (.61, p<.01) than psychosocial functioning (.22, n.s.). Within the psychosocial domain, these correlations were moderate and significant (p<.01) for social (.46) and school (.32), indicating emotional functioning (.12, n.s.) was the source of crossinformant variance. For both parent-proxy and self-report, HRQOL was significantly (p<.001) lower for CP patients than healthy children, with large effect-sizes for differences between these groups for both physical (self-report = .94, parent-proxy = 1.70) and psychosocial functioning (self-report = .89, parentproxy = 1.76). For child and parent-proxy, greater CP disease severity was associated with lower total HRQOL (hemiplegia > diplegia, quadriplegia, p<.05). Conclusions: Our most striking finding is that children with CP can reliably report their HRQOL. Although parent-child correlations for physical, social, and school functioning are moderate to strong, the small, non-significant correlation for emotional functioning (the most internalized psychosocial domain) indicates parents are not accurate reporters of their children’s emotional state, and emphasizes the importance of child self-report. Additionally, large effect-sizes between CP patients and healthy children in both physical and psychosocial functioning suggest the latter as an important domain that should be measured and addressed, in addition to traditional physical measures. Implications for Policy, Delivery or Practice: Children with CP suffer distress in both physical and psychosocial functioning. The feasibility of self-report in CP patients suggests a unique opportunity to evaluate HRQOL in this population, allowing for targeted interventions that address areas of concern for the child, including physical and emotional difficulties, to begin to hear the voices of these children. Primary Funding Source: March of Dimes • Obesity and Medicaid: A Life-Cycle Model of Pediatric Obesity Judith Shinogle, Ph.D., Melayne Morgan McInnes, Ph.D., Eric Johnson, Ph.D. Presented by: Judith Shinogle, Ph.D., Assistant Professor/NCHS AcademyHealth Fellow, Arnold School of Public Health, University of South Carolina, NCHS 3311 Toledo Road, Rm 3310, Hyattsville, MD 20782; Tel: 301458.4799; Email: shinogle@cop.sc.edu Research Objective: The prevalence of obesity in the U.S. has increased at epidemic rates for both children and adults. The increase in obesity potentially raises Medicaid expenditures by two pathways. First, obesity has been shown to increase the risk of a variety of chronic conditions and diseases even in childhood. Second, obesity may impact outcomes in the labor and marriage markets and thereby affect the likelihood of qualifying for Medicaid. We consider both pathways in calculating the obesity attributable fraction of Medicaid expenditures for children and adults. Study Design: Using data from the 1998 Medical Expenditure Panel Survey (MEPS) and the 1996- 1997 National Health Interview survey, we estimate a two part Medicaid expenditures model for children ages 4-17 and adults ages 1864. We follow the Manning and Mullahy algorithm for retransormation of logged dependent variable. The model of Medicaid expenditure includes controls for characteristics other than obesity that may cause expenditures to differ. Since MEPS has a complex survey design, all analysis was performed using survey weights, primary sampling units, and strata as defined by the documentation and analyzed with StataTM survey commands. We also consider the links between adult obesity and childhood obesity. Longitudinal data shows that obesity in childhood raises the risk of adult obesity substantially even after controlling for parental obesity. Using probability estimates from longitudinal data, we calculate the fraction of adult Medicaid expenditures that can be attributed to pediatric obesity. Population Studied: The population studied for this paper are children ages 4 to 17. Principal Findings: We find that children’s obesity accounts for nearly 8% of children’s annual Medicaid expenditures while adult obesity accounts for over 12% of adult Medicaid expenditures. When we link adult obesity back to pediatric obesity, we find that pediatric obesity is associated with an increase in adult Medicaid expenditures of nearly 3%. The discounted lifetime cost to Medicaid of adult obesity is found to be over $900. Conclusions: Our results for the pediatric obesity attributable fraction of adult Medicaid expenditure suggest that more emphasis needs to be given to the prevention and reduction of childhood obesity. Studies exploring the causes of the increase in adult obesity may also want to consider the role of pediatric obesity in adult obesity. Focusing solely on adult obesity may lead one to look for factors that affect current adults while missing the root causes that occur much earlier. Implications for Policy, Delivery or Practice: From the perspective of policy makers, a better understanding of the full life-cycle cost of obesity will determine whether there are potential cost savings from allocating resources to the prevention of pediatric obesity. • Promoting Change for Children through Parent Leadership and Civic Engagement: A Report on the Connecticut Parent Leadership Training Institute Michele Solloway, Ph.D., RPP Presented by: Michele Solloway, Ph.D., RPP, Research Associate Professor, Health Management and Policy, University of New Hampshire, Hewitt Hall, #327, Durham, NH 03824; Tel: 603.862.4150; Fax: 603-862-3461; E-mail: micheles@cisunix.unh.edu Research Objective: Evaluate the effects of Connecticut Parent Leadership Training (PLTI) on civic engagement, parent leadership in communities, state policy, systems serving children, and outcomes for children, families and communities Study Design: Retrospective design included focus groups, participant survey, and in-depth interviews with participants and community leaders. The survey included assessments of the curriculum; measures of civic engagement, literacy and leadership skills; and outcome measures for individuals, children, families, and communities. Descriptive statistics were used for survey data. Content and thematic analyses were used for qualitative data. Population Studied: All PLTI participants over 10-year lifetime of project n=836. Principal Findings: The PLTI is a state-sponsored community-based program located in 10 sites and consists of a 20-week training curriculum designed to prepare parents to become leaders in their communities. It teaches principles of child development, how to effect change in communities, tolerance for diversity, and civic skills, tools, and knowledge. The PLTI attracts people from all socioeconomic and demographic groups. The sites vary significantly by demographic groups, but participant outcomes and expectations showed consistently high scores. The curriculum and instructors received high scores with some variation by training module, site and sociodemographic groups. 80 percent of respondents said PLTI improved their ability to be an agent of change in their community and improved their self-confidence. 93-51 percent use various civic skills at least once a month or more. 49 percent said PLTI helped them make changes in their children’s schools or communities and provided new opportunities for participation and civic engagement. 20 percent returned to school for additional or advanced education; 15 percent got new jobs; 11 percent developed new careers; and 8 percent received raises at their place of employment. 79 percent reported positive changes in their children: Almost half said their children are now participating in community activities; 41 percent said their children showed improvements in self-confidence; and 31 percent said their children began to take more interest in the news. About one-third said their children showed positive changes in 4 or more outcomes. 61 percent said PLTI helped their families, including improved family cohesiveness, family problem solving; quality time spent with each other; and feeling more connected with other families in the community. Conclusions: The PLTI is an effective program for engaging parents to become leaders and agents of change for their children at the individual and policy level. When given civic tools, parents can guide public policy and decision-making through their commitment to children. Significant positive externalities for children and families are found. Implications for Policy, Delivery or Practice: Parents represent a significant resource for policy makers and systems serving children. Continuation and replication of PLTI in other states is warranted. Funding remains critical. Methodologies for tracking ripple effects require further investigation. Primary Funding Source: State of Connecticut, Commission on Children • Psychiatric Comorbidity among Hospitalized Children and Adolescents Joseph Thompson, M.D. M.P.H., James Robbins, Ph.D., Mary Aitken, M.D. M.P.H., Teresa Kramer, Ph.D., Terri Miller, Ph.D. Presented by: Joseph Thompson, M.D. M.P.H., Director, Arkansas Center for Health Improvement, University of Arkansas for Medical Sciences, 5800 West 10th Street, Little Rock, AR 72204; Tel: 501.660.7555; Fax: (501) 660-7543; E-mail: thompsonjosephw@uams.edu Research Objective: To examine patterns of comorbid psychiatric diagnoses in patients 6-17 years old hospitalized for selected illnesses and injuries and to determine length of stay and hospital charges associated with comorbid psychiatric disorders. Study Design: Analyses are based on the 1997 Healthcare Cost and Utilization Project (HCUP) Kid s Inpatient Database (KID). The KID is the only national, all-payer database of hospital discharges for children. KID data are weighted to represent all pediatric discharges from general hospitals in the U.S. Frequencies of discharges with principal diagnoses of selected acute and chronic illnesses and injuries, and secondary diagnoses of mental or substance-related disorders were calculated. Length of stay and costs were compared for patients with and without comorbid psychiatric diagnoses. Population Studied: The 1997 KID includes an 80% sample of discharges from all general and children's hospitals in the 22 participating states. A total of 1.9 million discharge records of patients 18 years of age and younger from 2,521 hospitals are included in the database. These analyses are limited to children between the ages of 6 and 17. Principal Findings: There was wide variation across medical conditions in proportions of discharges with secondary diagnoses of mental or substance-related disorders. Comorbid psychiatric diagnoses were most common for epilepsy (23.89%), burns (10.31%), traumatic brain injury (TBI; 9.67%), diabetes (8.60%), and internal injuries (7.11%) and less common for appendicitis (1.77%), sickle cell anemia (2.97%) and gastroenteritis (3.39%). Most common comorbidities overall included ADHD, substance-related disorders, depression, and mental retardation. The most frequent comorbidities within conditions included substance-related disorders in hospitalizations for internal injuries and TBI, depression in diabetes, and ADHD and developmental disorders in epilepsy. The presence of psychiatric comorbidity was consistently associated with longer mean length of stay, and higher mean hospital charges. Conclusions: Common comorbid psychiatric diagnoses in hospitalized children include prevalent and readily identified disorders that are associated with an increased burden of care. Patterns of diagnoses often follow recognized etiologic associations between mental or substance-related disorders and physical illnesses or injuries. Implications for Policy, Delivery or Practice: These national data highlight the need for increased attention to the influence of psychiatric disorders in the care of hospitalized youth. Comorbid mental health and substance-related disorders increase the length and costs of hospital stay. • Pediatric Hospitalizations for Traumatic Brain Injuries: 1997 and 2000 John Tilford, Ph.D., Mary Aitken, M.D. M.P.H., Allen Goodman, Ph.D., Jeffrey Killingsworth, BS, Jerril Green, M.D., Debra Fiser, M.D. Presented by: John Tilford, Ph.D., Associate Professor, Pediatrics/Health Policy and Management, University of Arkansas for Medical Sciences, 800 Marshall Street, Little Rock, AR 72202-3591; Tel: 501.364.3340; Fax: (501) 364-1552; Email: tilfordmickj@uams.edu Research Objective: This study evaluates the incidence, use of procedures, and outcomes of pediatric hospitalizations (age 0-18) for traumatic brain injuries (TBI) by patient and hospital characteristics using a unique database covering the years 1997 and 2000. Study Design: ICD-9 diagnosis codes from the Kids Inpatient Database for the years 1997 and 2000 were used to identify children with a TBI and classify the type of injury. ICDMAP-90 computer software also was used to develop abbreviated injury scores and injury severity scores to risk-adjust outcomes. The abbreviated injury scores were used to create mild, moderate, and severe categorizations of TBI severity. ICD-9 procedure codes were used to determine whether the patient received therapies such as mechanical ventilation and intracranial pressure monitoring. Patient payer status was coded as public, private, self-pay (uninsured), or other insurance. Population Studied: National estimates of pediatric TBI hospitalizations, use of procedures, and outcomes were developed using weights supplied with the database. Principal Findings: Hospitalizations involving mild TBI decreased by 28% over the two periods. There were no differences in the incidence of moderate or severe TBI hospitalizations. Patient insurance status was associated with use of therapies and in-hospital mortality. Self-pay patients with moderate TBI were less likely to receive mechanical ventilation, but there was no difference in in-hospital mortality. Self-pay patients with severe TBI, had significantly higher rates of unadjusted in-hospital mortality relative to privately insured patients (21.4% vs. 10.1%) and adjusted in-hospital mortality (OR = 3.45; p<0.001). Differences in injury severity explained some, but not all of the increased mortality in self-pay patients. Rates of intracranial pressure monitoring did not differ by payer status. Conclusions: A unique database for developing national estimates of pediatric hospitalizations indicates a downward shift in hospitalizations for mild TBI consistent with recent management guidelines. For moderate and severe TBI hospitalizations, the data show significant differences in inhospital mortality and therapies for uninsured children, but the available evidence does not provide a link between quality of care and outcomes. Implications for Policy, Delivery or Practice: Understanding why uninsured children with TBI die more frequently than publicly or privately insured patients is necessary to generate a link between health insurance expansions and reductions in TBI-related deaths. This study suggests insurance may play a role in reducing injury severity (prevention) rather than improving technical quality of care, but the possibility that better outcomes for insured patients are related to higher quality care cannot be ruled out. Primary Funding Source: HRSA, MCHB • SCHIP Eligibility and Access to Care for Children with Special Health Care Needs: Results from a Nationally Representative Survey Hao Yu, M.Sc., Andrew Dick, Ph.D, Peter Szilagyi, M.D., M.P.H. Presented by: Hao Yu, M.Sc., Ph.D Candidate, Community and Preventive Medicine, University of Rochester, 601 Elmwood Avenue, Box 644, Rochester, NY 14642; Tel: 585.275.3432; Fax: (585)461-4532; E-mail: hao_yu@urmc.rochester.edu Research Objective: While studies in specific states have examined enrollment in the State Children’s Health Insurance Program (SCHIP) among children in general and children with special health care needs (CSHCN), little is know at the national level about the role of SCHIP with respect to CSHCN. This study aims to assess the: (1). Proportion of CSHCN eligible for SCHIP across the U.S., (2). Proportion of SCHIP-eligible CSHCN who are uninsured, (3). Characteristics of the SCHIP-eligible but uninsured CSHCN, and (4). Difference in unmet needs and satisfaction of care between CSHCN enrolled in SCHIP and those eligible but uninsured. Study Design: Data were from the first National Survey of CSHCN, which was conducted in 2000-2001. Bivariate and multivariate analyses were performed. SCHIP-eligibility was defined by age and income according to state-specific policies as of October 2000. Population Studied: All the 38,866 CSHCN interviewed by the survey. Principal Findings: Nationally, 19.0% of CSHCN, or 1.7 million, were eligible for SCHIP in 2000, and among these eligible CSHCN, 8.2%, or 141,000, were uninsured. Substantial variation existed across states in terms of SCHIP eligibility and the proportion of eligible but uninsured CSHCN. CSHCN who were SCHIP-eligible but uninsured were less likely than CSHCN enrolled in SCHIP to have a personal health care provider (70.5% vs. 85.6%, P<0.001), more likely to have an unmet need (47.7% vs. 14.4%, P<0.05), and less satisfied with care (77.7% vs. 89.8%, P>0.05). After controlling for other patient features, the SCHIP-eligible but uninsured CSHCN were 5 times more likely to have unmet needs than those enrolled in SCHIP. Between the SCHIP-enrolled CSHCN and CSHCN who were SCHIP-eligible but privately insured, there were significant differences in the rates at which CSHCN had a personal provider (85.6% vs. 91.7%, P<0.01), although the two groups had similar rates of usual source of care (92.0% vs. 92.8%, P>0.05). The two groups were also similar in rates of unmet needs (14.4% vs. 12.1%, P>0.05), and of satisfaction with care (89.6% vs. 91.6%, P>0.05). Conclusions: A substantial number of CSHCN nationally were eligible for SCHIP but were uninsured, and these uninsured CSHCN were more likely to have problems in access to health care. The SCHIP-enrolled CSHCN resembled CSHCN privately insured in terms of unmet needs and satisfaction. Implications for Policy, Delivery or Practice: It may be helpful for states with high insurance rates among SCHIPeligible CSHCN to share strategies by which they successfully enrolled these children into SCHIP. On the other hand, states with low insurance rates may wish to review their eligibility criteria, enrollment practices, and outreach strategies. Another implication is that, despite the high rates of unmet needs, satisfaction with care is relatively high according to the standard CAHPS measures. These measures may not be sensitive indicators of unmet needs for vulnerable populations such as CSHCN. An implication for clinicians is that many uninsured CSHCN may in fact be eligible for SCHIP. Clinical offices can play a role in educating about SCHIP, and in helping families enroll. Primary Funding Source: The Maternal Child Health Bureau Invited Papers Strategies for Moderating the Long-Term Impact of Childhood Obesity Chair: Christopher Forrest, M.D., Ph.D. Sunday, June 6 • 5:00 p.m.-6:30 p.m. • Panelists: Scott Gee, Kaiser Permanente, Roland Sturm, RAND, Joseph Thompson, University of Arkansas for Medical Sciences (no abstracts provided) Invited Papers Impact of SCHIP on Vulnerable Children: Findings from the Child Health Insurance Research Initiative Chair: Cindy Brach, M.P.P. Monday, June 7 • 8:30 a.m.-10:00 a.m. • Panelists: Andrew Dick, University of Rochester; Elizabeth Shenkman, University of Florida; Peter Szilagyi, University of Rochester Medical Center (no abstracts provided)