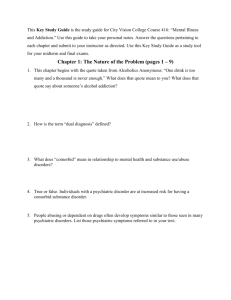
Behavioral Health
advertisement

Behavioral Health Call for Papers Disparities in Treatment for & Impact of Mental Illness Chair: Greer Sullivan, M.D., M.S.P.H. Monday, June 7 • 8:30 a.m.-10:00 a.m. • Severe Mental Illness and Congestive Heart Failure Outcomes among Veterans Jim Banta, M.P.H., B.S., Ronald Andersen, Ph.D., Alexander Young, M.D., M.S.H.S., William Cunningham, M.D., Gerald Kominski, Ph.D. Presented by: Jim Banta, M.P.H., B.S., Ph.D. Candidate, Health Services, UCLA, 1037 Willis Court, Colton, CA 92324; Tel: 909.825.2968; E-mail: jbanta1@msn.com Research Objective: Congestive heart failure is the leading cause of death among those greater than 65 years of age and is the single most expensive condition covered by Medicare. Co-morbid mental illness may lead to negative outcomes through worsened self-care and interactions with health care providers. Depression, for instance, is often associated with increased mortality and health services utilization among cardiac patients. This study focuses on the effect of severe mental illness (SMI) on mortality and readmission of heart failure patients; but also considers outpatient care. Study Design: Inpatient and outpatient data for several fiscal years were obtained from the Department of Veterans Affairs’ centralized patient database. The first heart failure admission of Fiscal Year 2001 was taken to be the index admission for this study. Logistic regression was used to test the effect of mental illness on one-year mortality and readmission. Logistic and linear regression was also used to examine receipt of outpatient medical care preceding the index admission. Using a behavioral model approach, adjustment was done for personal characteristics, including service-connected disability, co-morbid medical conditions (as measured by the CHF Index and Elixhauser method for co-morbid medical conditions), and contextual measures of the hospital and county of residence in which care was delivered. Population Studied: Veterans with a primary inpatient diagnosis of congestive heart failure during during federal Fiscal Year 2001 were selected. Patients were identified as SMI if any one of the ten diagnosis fields in the index admission or in an inpatient or outpatient service in the twelve months preceding the index admission included schizophrenia, PTSD or severe bi-polar disorder. Principal Findings: Inpatient data was obtained for 15,739 patients in 127 of 130 active VA medical centers or health care systems. Thirteen percent of patients died within twelve months of admission and fifty-four percent were readmitted. Of those living at least one more year, forty-seven percent were readmitted. Seven percent of the veterans had a severe mental illness. Twenty percent of those with SMI had cooccuring substance abuse compared to ten percent of those with no identified mental illness. Those with SMI were more likely to die than those having no mental diagnosis (Odds Ratio 1.34). This despite those with severe mental illness being younger than those with no identified mental illness (64 versus 70 years of age), and being less medically severe (CHF index of 2.4 versus 2.5). Severe mental illness was not significantly associated with readmission. Mental illness was not associated with a lower likelihood of receiving outpatient primary care in the twelve months preceding the index admission. In fact those with SMI were more likely to have received any primary care. However, substance abuse was associated with fewer outpatient services. Conclusions: After adjusting for many factors, heart failure patients with SMI were more likely to die than veterans with no mental illness. Implications for Policy, Delivery or Practice: Interventions to improve medical care in people with SMI or substance abuse are needed, particularly among those nearing retirement age. Such efforts could lead to reduced mortality. Primary Funding Source: SAMHSA • The Effect of Mental Disorders on Labor Market Outcomes among Latino Americans Pinka Chatterji, Ph.D., Margarita Alegria, Ph.D., Mingshan Lu, Ph.D. Presented by: Pinka Chatterji, Ph.D., Health Economist, Cambridge Health Alliance-Harvard Medical School, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th Floor, Somerville, MA 02143; Tel: 617.503.8449; Fax: 617.503.8430; E-mail: pchatterji@charesearch.org Research Objective: This paper investigates the effect of psychiatric disorders on current employment, the number of weeks worked in the past year, and the number of work absences in the past month among Latino Americans. Study Design: We use multiple regression models to estimate the association between psychiatric disorders and labor market outcomes. Psychiatric disorders are represented by four dummy variables indicating whether or not the respondent met diagnostic criteria for substance abuse/dependence, major depression, anxiety, or any mental disorder in the past 12 months. The models include controls for race/ethnicity, age, education, marital status, foreign born, and the number of children. Some models include an indicator of any lifetime psychiatric disorder. Standard errors are adjusted for clustering on state of residence. Drawing inference about the effects of mental disorders on labor market outcomes is complicated due to unobserved heterogeneity problems. Mental disorders may be affected by unobserved personal and social characteristics that also affect labor market outcomes. Moreover, one’s labor market outcomes can affect his current mental health. To address these issues, we follow previous research and estimate instrumental variables models using onset of mental disorders during childhood as an identifying instrument. Population Studied: Data come from the National Latino and Asian American Study (NLAAS). NLAAS is a national psychiatric epidemiologic study being conducted to measure psychiatric disorders and mental health service usage in a representative sample of Asians and Latinos. Unlike most population-based surveys, NLAAS provides detailed and good quality data on mental health status, as well as information on demographics and labor market participation. We limit the analysis sample to 1,503 Latino respondents between 18 and 65 years old who are not in school and who have complete survey information. All models are estimated separately by gender. Principal Findings: All psychiatric disorders analyzed have a negative impact on the probability of being currently employed. This finding persisted in instrumental variables models, as well as in models that included a control for any lifetime psychiatric disorder. Among males, having a psychiatric disorder is associated with a 16 to 37% reduction in the probability of being employed. Among females, having a psychiatric disorder is associated with a 14 to 25% reduction in the probability of being employed. However, among employed males and females, psychiatric disorders do not have a statistically significant association with work absences or the number of weeks worked in the past year. Conclusions: The findings indicate that psychiatric disorders have large effects on employment among Latino males and females. These results are consistent with previous work, which has focused on majority populations. Psychiatric disorders appear to have important impact on individuals’ ability to obtain and/or maintain employment. Implications for Policy, Delivery or Practice: By providing evidence on the social costs of mental disorders among Latino Americans, this study has important policy implications on issues such as mental health insurance coverage policy and health care resource allocation. The findings imply that improving access to effective mental health screening and treatment may have benefits in the labor market. Primary Funding Source: NIMH, NCMHHD • Disparities in the Adequacy of Depression Treatment in the United States Jeffrey Harman, Ph.D., Mark Edlund, M.D., Ph.D., John Fortney, Ph.D. Presented by: Jeffrey Harman, Ph.D., Assistant Professor, Health Services Administration, University of Florida, P.O. Box 100195, Gainesville, FL 32611-0195; Tel: 352.273.6060; Fax: 352.273.6075; E-mail: jharman@phhp.ufl.edu Research Objective: There is evidence that disparities in depression care exist by factors such as age, race/ethnicity, and type of insurance. The purpose of this study is to assess whether observed disparities in care are due to differences in rates of initiating treatment or differences in the quality of treatment once treatment has been initiated. Study Design: Data from the 2000 Medical Expenditure Panel Survey (MEPS) are used to obtain nationally representative estimates of the rates at which individuals with self-reported depression utilize antidepressant medications and/or psychotherapy or mental health counseling. Additionally, for those individuals who use some depression care, estimates of the adequacy of care received are obtained and compared by patient characteristics. Adequate care is defined as filling at least four prescriptions for an antidepressant medication at a minimally adequate daily dosage or receiving at least eight psychotherapy or mental health counseling sessions during the calendar year. Weighted logistic regression models are estimated to assess the independent role of patient characteristics such as age, race/ethnicity, and type of insurance on rates of initiating depression treatment for individuals with self-reported depression and on rates of adequate treatment for those individuals who receive treatment after controlling for health status, functional status, education, income, and marital status. Population Studied: The Household Component of the 2000 MEPS (N=25,096) is used. The MEPS is a nationally representative survey of households in the United States conducted annually by the Agency for Healthcare Research and Quality. All individuals with self-reported depression are included in the study (N=1,347). Principal Findings: African-Americans (OR = 0.48) and Hispanics (OR = 0.47) with self-reported depression were significantly less likely to fill an antidepressant prescription than Caucasians, but if at least one antidepressant prescription was filled, there was no significant difference in the probability of receiving an adequate trial of antidepressant medication by race/ethnicity. No significant differences in the probability of receiving any psychotherapy or mental health counseling by race/ethnicity was observed, but AfricanAmericans were more likely to receive an adequate course of psychotherapy than Caucasians (OR = 2.35). Young adults were less likely to initiate depression treatment (OR = 0.48), and if initiated, were less likely to receive adequate treatment (OR = 0.55). No significant differences for elderly persons were observed. Individuals without insurance were significantly less likely to receive any treatment than individuals with private insurance (OR = 0.58), but if treatment was initiated, no significant difference in the probability of receiving adequate treatment was observed by type of insurance. Individuals who received both antidepressants and psychotherapy/counseling were more likely to receive adequate treatment than individuals who received only psychotherapy/counseling or only antidepressants (OR = 2.92). Conclusions: Disparities in depression care appear to be primarily due to differences in rates of initiating depression treatment, as rates of adequate care do not differ once treatment is initiated. Implications for Policy, Delivery or Practice: Interventions to reduce disparities in depression care should focus on initiating depression treatment. However, interventions that improve the adequacy of care once care is initiated are still needed, as rates of adequate treatment are low for all individuals with depression. Primary Funding Source: NIMH • Racial Differences in Quality of Care for Bipolar Disorder Amy Kilbourne, Ph.D., M.P.H., Gretchen Haas, Ph.D., Xiaoyan Han, M.S., Mark Bauer, M.D., Mujeeb Shad, M.D., Harold Pincus, M.D. Presented by: Amy Kilbourne, Ph.D., M.P.H., Assistant Professor of Medicine and Psychiatry, VA Pittsburgh CHERP, University of Pittsburgh, University Drive C, Pittsburgh, PA 15240; Tel: 412.688.6477; Fax: 412.688.6527; E-mail: Amy.Kilbourne@med.va.gov Research Objective: Despite the existence of practice guidelines, quality of care and subsequent outcomes for bipolar disorder remain suboptimal. Potential disparities in quality of care for patients with bipolar disorder have been relatively unexplored. We therefore assessed racial differences and other patient factors associated with quality of care for bipolar disorder. Study Design: We conducted a retrospective analysis of data from the VA National Patient Care Database (NPCD) on patients with either one inpatient or two separate outpatient ICD-9 diagnoses of bipolar disorder (I, II, or NOS) in FY 2001. Data on all psychopharmacologic prescriptions were ascertained from the VA Pharmacy Benefits Management database, and patient demographic and outpatient use data were collected from the NPCD in FY 2001. We applied American Psychiatric Association Guideline-based indicators to assess quality of care: 1) current prescription for a mood stabilizer, 2) no antidepressant monotherapy (i.e., prescription for an antidepressant without concurrent prescription for mood stabilizer), and 3) >3 outpatient mental health visits within one year. Multiple logistic regression analysis was used to determine whether race/ethnicity was independently associated with quality of care for bipolar disorder, controlling for patient factors including age, gender, service connection eligibility, marital status, and number of comorbidities. Alternative analyses were conducted in which we limited our sample to patients diagnosed with bipolar I disorder only (n=2736). Population Studied: Patients diagnosed with bipolar disorder receiving care at one of 10 VA facilities located in Pennsylvania, West Virginia, Ohio, Delaware, and Maryland. Principal Findings: Out of 252,621 patients receiving care in VISN 4 in FY 2001, 2958 (1.2%) met criteria for bipolar disorder diagnosis. The mean age was 52 years, 11% were women, and 12% African-American. Overall, 80.1% of patients were currently prescribed a mood stabilizer, 13.4% were prescribed antidepressant monotherapy, 63.5% received >3 outpatient mental health visits. About half (53.4%) met all three criteria. After adjustment for the aforementioned patient factors, African-Americans were less likely to have a prescription for a mood stabilizer (OR=.71;p=.02) and more likely to be on antidepressant monotherapy (OR=1.61;p=.001) compared to whites. Older (>60 years) patients were also less likely to have a prescription for a mood stabilizer (OR=.54;p<.001), more likely to be on antidepressant monotherapy (OR=1.32;p=.04), less likely to receive >3 outpatient mental health visits (OR=.61;p<.001), and less likely to meet all three criteria (OR=.54;p<001) after adjustment. Similar results were obtained when the sample was limited to bipolar I disorder. Conclusions: The majority of VA patients with a diagnosis of bipolar disorder are receiving guideline-concordant care for bipolar disorder. Nonetheless, potential gaps in quality of care are evident in continuity of outpatient care; and in particular, for African-Americans and older patients, even among a more restricted sample of bipolar I patients. Implications for Policy, Delivery or Practice: Identifying the reasons for potential gaps in quality of care, including patient preferences, diagnostic instability, provider decision-making, and management factors will inform future quality improvement interventions to reduce disparities in care for bipolar disorder. Future efforts include the validation and application of performance measures to monitor quality improvement efforts for patients with bipolar disorder across the U.S. Primary Funding Source: VA • Mental Health and Employment Transitions among LowIncome Women Leigh Ann White, Ph.D. Candidate Presented by: Leigh Ann White, Ph.D. Candidate, Health Policy & Management, Johns Hopkins School of Public Health, 6427 79th Street, Cabin John, MD 20818; Tel: 301.320.9029; Fax: 301.320.1762; E-mail: lwhite@jhsph.edu Research Objective: This research examines how mental health affects employment opportunity of women in lowincome families. There is accumulating evidence regarding the negative relationship between poor mental health status and employment. However, we know little about how mental health and its correlates operate in influencing employment and job stability. This knowledge is an essential component of developing strategies to address mental health issues in publicly financed settings. Study Design: Estimates of the impact of mental health symptoms on subsequent employment come from probit regressions of baseline factors on employment status at the second interview. Subgroup analyses are performed for women with different work histories at baseline. OLS and tobit regressions of the proportion of time spent employed between interviews add information on job holding between interviews. All analyses focus on the effect of symptoms of prevalent mental disorders, measured using the 18-item Brief Symptom Inventory, and interactions between mental health, initial employment state, and key baseline covariates. Population Studied: Data are from two waves of interviews from the survey component of the Welfare, Children, and Families Three-City Study. The analytic sample consists of mothers in families with incomes up to 200 percent of the Federal Poverty Level, in poor neighborhoods of Boston, San Antonio, and Chicago. The analytic sample is limited to approximately 1,700 adult women ages 18 to 64 who had complete data on key variables in both waves of the survey. Principal Findings: Probit findings suggest a negative effect of baseline psychological distress on employment entry for the unemployed. Controlling for covariates, those meeting BSI case criteria were significantly less likely to be subsequently employed. Predicted probabilities were .24 vs. .13 among those with no recent experience, and .58 vs. .51 among the experienced unemployed. Among the employed, psychological distress was a negative predictor of subsequent employment; predicted probabilities were .84 and .71. Findings from twolimit Tobit regressions of the proportion of time in employment add to the picture. Controlling for covariates, the distressed group was slightly more likely to be employed at any time, .74 compared to .71. However, conditional on employment, they spent less time in jobs. Predictions showed that the women with symptoms of psychological distress spent about 43 percent of the period in some job, compared to 49 percent of the comparison group, a statistically significant difference. This finding suggests the possibility of "job churning." Conclusions: Symptoms of prevalent psychiatric syndromes may be important barriers to achieving stability in employment. They may prevent many low-income women, especially the socially marginalized, from entering employment altogether. For women with few skills and very low educational attainment, mental health problems may derive from and compound stressors that impede employment entry. Even among the employed, there is evidence suggesting a relationship between symptoms of mental disorders and labor force attachment. Implications for Policy, Delivery or Practice: Future research using these data will focus on the effects of mental health symptoms on job entry, job loss, and job-to-job transitions, to explore the relationship in a more thorough manner. The research presented here suggests the importance of continuing to develop better ways to screen and assess for mental health problems in multiple locations, and to coordinate across systems such as TANF offices, vocational rehabilitation centers, and mental health providers. It also suggests the importance of aiding in employment retention by addressing mental health issues through job training and on the job. Primary Funding Source: NIMH, University of Michigan National Poverty Center Call for Papers Mental Health in Community Context Chair: Kenneth Wells, M.D., M.P.H. Monday, June 7 • 4:00 p.m.-5:30 p.m. • Witness for Wellness: A Community-University Participatory Research Mental Health Initiative Loretta Jones, M.A., Ricky Bluthenthal, Ph.D., Marcia Ellison, Ph.D., Paul Koegel, Ph.D., Katy Minnium, M.P.H., Aziza Lucas-Wright, M.Ed., Ken Wells, M.D., Ph.D. Presented by: Ricky Bluthenthal, Ph.D., Social/Behavioral Scientist, Behavioral Health Sciences, RAND, 1700 Main Street, Santa Monica, CA 90407; Tel: 310.393.0411 Ext. 6642; Fax: 310.451.7004; E-mail: rickyb@rand.org Research Objective: Research indicates that depression treatment may have even greater positive outcomes among people of color than whites. Yet, no model has been developed, to date, to bring mental health Research suggests that minorities are less likely than whites to receive appropriate care for depression yet benefit at least as much or more from interventions that improve depression care. Yet no model has been developed to increase public engagement in depression treatment among minority communities. This presentation involves an intervention and evaluation model, and preliminary findings from such a community-based effort. Study Design: “Witness for Wellness” is a communitypartnered participatory research (CPPR) project with active community involvement in all stages. The project was initiated by Healthy African American Families, a community based organization (CBO) in South Los Angeles, UCLA, Charles R Drew Medical University, and RAND. The stages are: 1) coalition development; 2) community conferences; 3) formation of working groups to develop and implement strategies; 4) participatory evaluation using mixed methods, such as pre-post surveys of conferences, qualitative studies, and secondary data sources. Population Studied: South Los Angeles, CA, a predominantly African American and Latino community. Principal Findings: Over 30 CBOs joined and participated in coalition planning for a year. A local conference attracted 500 community members, 60 of whom later formulated plans for 3 working groups: Talking Wellness (reducing stigma and increasing community strength); Building Wellness (assuring assess and services quality); Supporting Wellness (policy and advocacy to protect vulnerable populations). As an example of evaluation data, 370 conference participants completed a survey: 50% worked in a CBO, 20% were providers, 15% government employees, 10% academics, and 5% grass roots community members; 50% were African American and 30% Hispanic; and most (90%) were women. The surveys suggested that attendees became better educated about signs and symptoms of depression and the value of and how to obtain treatments. Forty roundtable discussions were recorded by trained notetakers and coded by community and academic partners. Qualitative analysis suggested that depression is viewed primarily as a community problem. Key barriers to treatment included lack of knowledge of resources, social stigma, cultural values (e.g., that spirituality should suffice, keeping problems in the family, stoicism), endemic racism and “fear of the dominant culture’s solution to our problem,” and “normalization” or accommodation to this illness. Community members reported that they turned for help most often to non-familial social intimates. The presentation will provide further detail on the intervention model and evaluation findings. Conclusions: Participatory models are feasible for engaging community members in a research effort to address depression; but this demonstration has to date been more successful in engaging African Americans and women. Additional strategies are needed to reach diversity goals. The approach yields data that both community and academic partners are empowered to share. The effectiveness of the model is the subject of future study. Implications for Policy, Delivery or Practice: National clinical research recommendations call for new models of community participation. This mental health project demonstrates one such approach that holds potential to address this research and policy need, through empowering community members as research partners and empowering academic investigators as community intervention partners. Primary Funding Source: NIMH, RAND • Does Relative Poverty Predict the Need for Mental Health Care? Christine Eibner, Ph.D., Roland Sturm, Ph.D., Carole Roan Gresenz, Ph.D. Presented by: Christine Eibner, Ph.D., Associate Economist, Economics and Statistics, RAND Corporation, 1700 Main Street, P.O. Box 2138, Santa Monica, CA 90407; Tel: 310.393.0411 Ext. 6522; E-mail: eibner@rand.org Research Objective: We examine whether an individual’s income status relative to a reference group affects mental health outcomes. Relative poverty differs from low income because individuals with high-income reference groups might be well-off with respect to the general population but still deprived relative to their peers. Our contributions to the literature include 1) defining reference groups using demographic characteristics in addition to geographic area, 2) looking at an individual’s relative income status rather than aggregate-level income inequality, and 3) focusing specifically on mental-health related outcomes. The four mental health outcomes we examine are depression, anxiety disorder, severe mental health disorders, and a summary variable indicating any probable mental health problem. Study Design: Our primary data source is the national household survey component of HealthCare for Communities (HCC), funded by the Robert Wood Johnson Foundation to track the effects of the changing health care system on individuals at risk for alcohol, drug abuse, or mental health disorders. HCC is a complement to the Community Tracking Survey (CTS) and reinterviews participants of the main study. To construct relative poverty measures, we used data from the 5% Public Use Micro Data Sample of the 2000 Census. Our measure of relative poverty is defined using Yitzhaki’s index, a term that measures the expected income difference between an individual and others in his or her reference group that are more affluent. We evaluated the relationship between relative poverty and mental health using conditional logit models with reference group fixed effects. Population Studied: Adult respondents to the 60-site sample of the HCC study. Although the HCC over-sampled individuals who were likely to be at risk for mental health problems, our final results are weighted to be representative of the population. Principal Findings: Even after controlling for an individual’s absolute income status, those with low relative income are at higher risk for experiencing probable mental health problems. Our findings hold for all of the mental health outcomes examined. Conclusions: Our findings suggest that relative poverty is associated with an increased likelihood of probable depression, anxiety, severe mental health problems, and overall poor mental health. Our simulations suggest that a 25 percent decrease in relative poverty could decrease the probability of any likely mental health problems by as much as 8.7 percent. The evidence does not suggest that relative poverty has a markedly stronger impact on one particular mental health outcome as opposed to the others. Implications for Policy, Delivery or Practice: Social ordering and the perceptions of low relative status may contribute to socioeconomic disparities in mental health. Efforts to eradicate socioeconomic differentials should take into account psychological perceptions and self-esteem in addition to absolute material resources. Primary Funding Source: NIMH • Which Dimensions of Continuity of Mental Health Care Lead to Improved School Outcomes? Alka Indurkhya, Ph.D., Joy Basu, Ph.D., Jennifer Yu, M.S., Nicholas Ialongo, Ph.D. Presented by: Alka Indurkhya, Ph.D., Senior Research Scientist, Harvard University, 677 Huntington Avenue, Boston, MA 02115; Tel: 617.432.0964; E-mail: aindurkh@hsph.harvard.edu Research Objective: The school system in the United States is a significant provider of mental health services with three out of four children reporting treatment for mental disorders only from their school. This is the first study to examine the extent to which different dimensions of continuity of school based mental health services impact school outcomes such as grade repetition, suspension or expulsion, and future mental health service use. The aims of this research were: (a) to generate a set of dimensions for continuity of school based mental health care using parent, teacher, and school mental health professional reports for children who need/use behavior counseling services, and (b) to assess the impact of the different dimensions on future school outcomes. Study Design: Follow-up from 1993-2000 of a prospective study cohort of children in school. The school based mental health services module of the service assessment for children and adolescents (SACA) was used by teachers, school mental health professionals, and parents to report the need/use for behavior counseling services for each child in the cohort from 1993-2000. Three distinct dimensions of continuity of care were obtained from the SACA: timeliness, intensity, and stability. Information on grade repetition, expulsion and suspension were obtained from parent, and teacher reports. Logistic regression analysis was used to determine adjusted odds ratios and confidence intervals (CI) after adjusting for race, gender, and socio-economic status of the children for each of the dimensions of continuity for school based mental health care. Population Studied: A cohort of 678 first graders from nine schools in Eastern Baltimore. 87% of children are African American, 12% Caucasian, and 1% Native American, Hispanic, and Asian. The cohort contains 53% males. Principal Findings: Timeliness: 28.8% of the children were identifed as needing mental health services in Grade 1. Only one out of three children received needed services in a timely manner. Findings from logistic regression indicated that in Grade 6, children who did not receive services in a timely manner were 4.6 more likely (95% CI: (3.7, 8.3)) to need mental health services as compared to those whose needs were met in a timely manner in Grade 1. These children were also found to be 2.2 times more likely (95% CI: (1.8, 2.7))to face suspension or expulsion from school due to disciplinary reasons. The odds for grade repetition were not statistically significant. Intensity: 18% of the students received more than 10 hours of counseling from a mental health professional in Grade 1. These students were 5.3 times more likely (95% CI: (1.7, 8.4)) to need mental health services in Grade 6 when compared those that received less than 10 hours of counseling in Grade 1. The odds were not found to be statistically significant for grade repetition, expulsion or suspension. Stability: Only 23% of the children whose needs were met in a timely manner in Grade 1 were found to continue treatment until Grade 3. These children were twice as likely not to require more than 3 hours of mental health services by Grade 6 when compared to the children who received services in Grade 1 but did not receive needed services through Grade 3. The odds for grade repetition, expulsion, and suspension were not statistically significant. Conclusions: All three dimensions for continuity of school based mental health care in elementary school are predictive of mental health service use in Grade 6. Timeliness appears to be an extremely important dimension in the study of continuity of school based mental health care that may lead to improved school outcomes, and reduce the need for future mental health services. The dimensions studied did not impact grade repetition. Implications for Policy, Delivery or Practice: The results underscore the urgent need for assessing and providing school based mental health services to children in elementary school to help improve educational outcomes in middle school. Primary Funding Source: NIMH • Longitudal Relationships among Family Caregiving Intensity, Caregiver Role Strain and Treatment Outcomes for Persons with Comorbid Mental Illness and Substance Abuse Ingrid Rystedt, M.D., M.S. Presented by: Ingrid Rystedt, M.D., M.S., Ph.D. Candidate, Department of Community & Family Medicine, Center for the Evaluative Clinical Sciences, Dartmouth Medical School, 7251 Strasenburgh Hall, Hanover, NH 03755; Tel: 603.650.1141; Email: ingrid.rystedt@dartmouth.edu Research Objective: (1) To examine the long-term relationships between caregiver role strain and the intensity of caregiving for clients with comorbid severe mental illness and substance abuse and (2) to evaluate the impact of the intensity of caregiving and caregiver role strain on the course of the client's disorder. Study Design: Secondary data analysis using data from The New Hampshire Dual Diagnosis Study, a randomized clinical trial comparing two treatment models. Primary caregivers who were family members of the clients were included in this study (n=155). Original study hypotheses: (1.) The higher the cumulative intensity of informal care provided by the family caregiver, the greater the current level of perceived role strain. (2.) The higher the cumulative role strain perceived by the family caregiver, the lower the current caregiving intensity. (3.) High caregiving intensity and low role strain are associated with improvements in client outcomes over time. Analytic approach: Mixed effects regression analysis was utilized to model the longitudinal relationships between caregiving intensity, caregiver role strain and client outcomes. Population Studied: Client data were collected between 1989 and 1993 in seven mental health centers in New Hampshire. Clients were followed for three years and were interviewed at six-month intervals about psychiatric symptoms, substance abuse, service use, income sources and contacts with friends or family. At corresponding time points, primary caregivers were interviewed about caregiving involvement and family burden. Data on client involvement with the legal system were collected. Principal Findings: More intense cumulative caregiving was strongly associated with higher levels of currently perceived role strain. Contrary to the initial hypothesis, the current caregiving intensity was significantly higher when family members had experienced high role strain over time. All caregiving variables (cumulatively high caregiving intensity, cumulatively low role strain and co-occurring cumulatively high caregiving intensity and low role strain) were significantly associated with reduced client substance abuse. Cumulatively low role strain was significantly associated with lower probability of client arrest. Conclusions: By illustrating the effects of caregiving on both family caregivers as well as clients, this study revealed both the benefits and social costs of informal caregiving. Although the caregiving intensity was generally sustained, high caregiving intensity was consistently associated with high levels of role strain. The previously identified beneficial effects of informal caregiving on client substance abuse outcomes were replicated with a longitudinal analysis. Implications for Policy, Delivery or Practice: The findings suggest that role strain in itself does not threaten caregiving involvement. However, the indirect effects of role strain on caregiver health may affect such involvement in a more longterm perspective. The continued identification of mechanisms to support family caregivers would contribute to at least three important goals: (1) improved quality-of-life for family caregivers, (2) improved client outcomes, and (3) the development of a more cost-effective treatment system for comorbid severe mental illness and substance abuse. Future research should explore how family members are most effectively enabled to sustain informal care while maintaining low to moderate levels of role strain. Primary Funding Source: NIDA, NIMH, AHRQ (Postdoctoral Fellowships) • The Effects of Community Risk and Resource Variables on Mental Health and Substance Abuse Need and Access to Care Susan Stockdale, Ph.D., Kenneth Wells, M.D., M.P.H., Lingqi Tang, Ph.D., Thomas Belin, Ph.D. Presented by: Susan Stockdale, Ph.D., Senior Statistician, NPI Health Services Research Center, UCLA, 10920 Wilshire Boulevard, Suite 300, Los Angeles, CA 90024; Tel: 310.794.3732; Fax: 310.794.3724; E-mail: sstockdale@mednet.ucla.edu Research Objective: In spite of increasing concern over the gap between development of effective treatments for common behavioral health conditions, such as depressive and anxiety disorders and alcohol/drug abuse, and their adoption in the community, development of community-based strategies to improve care is limited by the lack of availability of comprehensive national data on how community factors and their interaction with individual factors affect occurrence of behavioral health conditions or access to services for these conditions. This study uses national data to determine how a range of community risk and resource characteristics shape individual need for and access to behavioral health care. Study Design: Two waves of data from Health Care for Communities, a national household telephone survey fielded between 1997 and 2001. Dependent variables include any alcohol, drug, or mental health (ADM) condition or perceived need for ADM care, and use of specialty mental health and/or primary care for these conditions. Neighborhood characteristics were median household income, neighborhood stressors (violent crime arrest rate and residential crowding vs. isolation), and resources (churches per 1,000 capita, health food, alcoholic beverages, personal care facilities, recreational facilities, gambling establishments, and mental health care facilities). Individual variables include education, race/ethnicity, gender, marital status, age, family savings, social support, and exposure to violence. Population Studied: Adult Population with telephones in 60 US communities Principal Findings: We illustrate findings through analyses of need. Higher neighborhood income was significantly associated with greater probability of substance abuse. Residential crowding, and its interaction with individual social support, were negatively associated with behavioral health need, such that greater social support particularly affected (lowered) ADM need in less densely crowded neighborhoods. Greater availability of social interaction establishments (churches per capita, personal care facilities, gambling establishments as a group) was associated with lower ADM need, but greater availability of stores selling alcoholic beverages increased substance abuse. Further, individual exposure to violence particularly affected (increased) ADM need in high crime areas, while those not exposed to violence in these areas had lower ADM need. We will also present and discuss findings related to access to ADM care. Conclusions: Overall, this study suggests that neighborhood factors – spanning physical capacities and risk factors, social resource availability, and physical exposure factors (alcohol availability) – are uniquely associated with mental health and substance abuse problems even after controlling for individual predictors of need. Further, community factors interact with important individual risk and protective factors, such as social support and exposure to violence, in shaping ADM need. Implications for Policy, Delivery or Practice: These findings, particularly if replicated in other data sets, have potential implications for targeting of prevention and treatment interventions to high-risk populations within the context of their neighborhood characteristics, and for the development of community resource interventions. Primary Funding Source: RWJF Call for Papers Policy Developments in Mental Health & Substance Abuse Chair: Nancy Wolff, Ph.D. Tuesday, June 8 • 11:15 a.m.-12:45 p.m. • Coverage of Mental Health Benefits and Parity Laws Myles Maxfield, Ph.D., Lori Achman, M.P.P., Jeffrey Buck, Ph.D, Judith Teich, M.S.W. Presented by: Lori Achman, M.P.P., Health Analyst, Mathematica Policy Research, Inc., 600 Maryland Avenue, Suite 550, Washington, DC 20024; Tel: 202.264.3464; Fax: 202.863.1763; E-mail: lachman@mathematica-mpr.com Research Objective: Access to mental health care by individuals with mental illness depends largely on whether the individual has health insurance and the generosity of those benefits. Benefits are influenced by federal and state mental health parity laws. This paper estimates the number of individuals with mental health insurance benefits, the generosity of those benefits, and the number of individuals subject to state and federal mental health parity laws in 1999. Study Design: Estimates are based on the March 2000 Current Population Survey (CPS), the 1999 Medical Expenditure Survey—Insurance Component (MEPS-IC), and the Mercer Worldwide National Survey of EmployerSponsored Health Plans. Each survey uses a nationally representative probability sample with 1999 as the reference period. Population Studied: The non-institutionalized U.S. population in 1999. Individuals were categorized according to their reported primary source of health insurance. Principal Findings: In 1999, 37.6 percent of the U.S. population with health insurance had mental health benefits at full financial parity with their medical/surgical benefits, meaning equality in dollar limits, cost sharing and utilization limits. An additional 37.6 percent of the insured population had mental health benefits, but they were not at parity with medical benefits. Another 14.2 percent of the population had mental health benefits, but data was insufficient to estimate the generosity. Approximately 2.9 percent of insured individuals had no mental health benefits. No information was available on the mental health benefits of the remaining 7.7 percent. To ameliorate the disparity between mental health and medical/surgical benefits, many states, as well as the federal government, passed laws requiring some level of parity for mental health benefits. The Mental Health Parity Act of 1996, which required parity only in dollar limits, applied to only 42 percent of the U.S. non-institutionalized population in 1999. State mental health parity laws often go beyond the federal law to also require parity in cost sharing and utilization limits, but these laws reach far fewer people. In 1999, 13 states had mental health parity laws requiring full financial parity for the private, employer-sponsored market. These laws covered only 8 percent of individuals with private, employersponsored health insurance, or 4 percent of the entire U.S. population. Conclusions: Access to mental health care for many people may be limited by a lack of mental health insurance benefits or by benefits that are not generous. The generosity of mental health benefits of many health plans is unaffected by federal or state parity laws because of the exemptions contained in those laws. Implications for Policy, Delivery or Practice: Implementing full financial parity in all federal health programs, reducing the exemptions from parity laws, and implementing a federal full financial parity law may be effective tools for increasing access to mental health care. Primary Funding Source: SAMHSA • Cost Effectiveness of Public Sector Substance Abuse Treatment: Comparison of a Managed Care Approach to a Traditional Public Sector System Martha Beattie, Ph.D., Teh Wei Hu, Ph.D., Rui Li, Master of Medicine, Jason Bond, Ph.D. Presented by: Martha Beattie, Ph.D., Scientist, Alcohol Research Group, Public Health Institute, 2000 Hearst Avenue, Berkeley, CA 94709; Tel: 408.272.6535; Fax: 408.264.2637; Email: mbeattie@arg.org Research Objective: A primary premise of managed care is cost containment. Linking cost of care to the outcomes of that care leads to an examination of quality of care as well. This study compares the costs and cost effectiveness of public sector substance abuse treatment in two California counties with similar substance abuse treatment system histories, one of which implemented a managed care approach to treatment in 1997. The two counties were compared three years after the system change in MidState – the county that adopted a management of care perspective – to allow time for the system to stabilize. It was hypothesized that 1. the cost per client served would be lower in MidState than in SouthState – the county whose system remained virtually unchanged; and that 2. because of its attention to quality of care as well, the cost effectiveness ratios would show greater effectiveness in MidState than in SouthState. Study Design: Baseline and outcome data were collected by trained research interviewers. At twelve months 82% of MidState’s 198 subjects and 80% of SouthState’s 256 subjects were interviewed. Information on service utilization and costs for clients participating in the study came from the counties’ automated Management Information System -MISdatabases. Analysis is limited to those who could be matched to treatment utilization data in each county’s MIS – 196 in MidState and 208 in SouthState. Population Studied: Randomly selected adult clients entering public sector substance abuse treatment in two California counties from June, 2000 to June, 2001. Principal Findings: During the index episode of treatment, SouthState averaged significantly more group - 25.7 per user v. 13.9 per user- and individual treatment services - 7.3 v. 3.8 per user - than MidState. Residential services per client were not significantly different (48.7 v. 34.8 days per user). Results of the OLS regression analysis show that MidState costs for the index treatment were significantly lower even when adjusting for predictor variables that might tend to explain the differences in costs between counties. An earlier report found no significant differences in outcomes between counties. As a result, MidState has superior cost effectiveness in all seven Addiction Severity Index functional areas due to its lower cost per client treated. Conclusions: Costs of treatment during the index episode were lower in the county that has adopted a managed care approach to treatment, yet outcomes did not differ between that and the comparison county. Because of that lower cost, MidState can claim greater cost effectiveness for its treatment dollars. The lower costs were due to lower outpatient utilization in MidState than in SouthState. Notably, residential treatment days were not significantly different between the counties: MidState had explicit policies for residential programs to average 45 days for their clients, while SouthState left decision-making on length of stay to their residential programs. Implications for Policy, Delivery or Practice: That MidState utilized fewer outpatient services could be cause for concern, however this utilization is higher than for typical treatment programs. It may be that SouthState could reduce their outpatient utilization with little or no impact on outcomes. In this time of cost containment and reduction in budgets this strategy might be applicable. Primary Funding Source: NIDA • The Cost Offset of Behavioral Health Treatment in Medicaid Jeremy Bray, Ph.D., Todd Grabill, B.A. Presented by: Jeremy Bray, Ph.D., Senior Research Economist, Health, Social, and Economics Research, RTI International, 3040 Cornwallis Road, Hobbs Building, Research Triangle Park, NC 27709; Tel: 919.541.7003; Fax: 919.541.6683; E-mail: bray@rti.org Research Objective: For more than 20 years, the potential for a cost offset of behavioral health treatment has been a key area of interest to researchers and policy makers. A cost offset is achieved when utilization of behavioral health services results in a reduction in expenditures for other medical services. Cost-offset findings have been used to bolster recent parity legislation, urging equal insurance coverage for behavioral health and other medical services. Yet little has been done to assess the extent of a behavioral health treatment cost offset in publicly financed health plans. This study analyzes the claims history of Medicaid recipients with identified behavioral health disorders in order to estimate a cost offset of behavioral health treatment. Study Design: Secondary data analysis is conducted using administrative claims data from the State Medicaid Research Files of Michigan, New Jersey, Pennsylvania, and Washington from 1995 to 1998. Adults ages 21-64 with an identified mental health and/or substance abuse - MH/SA - disorder and a comparison sample of randomly selected non-MH/SA claimants are followed in each of the four states over the 4-year period. Their fee-for-service claims are used to generate a monthly longitudinal database. Multivariate regression models control for demographic and case-mix differences across individuals. Time-series analysis is conducted, and mean expenditures are plotted for pre- and post-treatment months. Population Studied: This study focuses on the adult Medicaid populations in Michigan, New Jersey, Pennsylvania, and Washington. Principal Findings: Expenditures for non-behavioral health services rise substantially prior to behavioral health treatment initiation and peak 1 month prior to treatment. Following behavioral health treatment initiation, other medical expenditures decline below pretreatment levels when measured at 12, 24, and 36 months after treatment initiation. Total expenditures return to but do not decline below pretreatment levels, indicating a cost offset but not overall cost reduction for behavioral health treatment. Other medical and total expenditures remain above the mean expenditure levels of the comparison sample. Conclusions: Several researchers have raised concerns that the cost-offset hypothesis promotes the justification of treatment based on cost savings rather than on costeffectiveness or better health, and behavioral health care therefore is held to a higher standard than general medical care. In demonstrating a cost offset but not an overall cost reduction for behavioral health treatment under the Medicaid program, we echo other researchers’ concerns. Our finding that long-term total costs do not increase following the initiation of behavioral health treatment suggests that followup treatment does not impose a serious economic burden. Implications for Policy, Delivery or Practice: Economic grounds alone should not determine coverage for behavioral health services and do not correspond to sound public policy. Nonetheless, our results suggest that economic concerns should not hinder the expansion of behavioral health coverage under the Medicaid program. Policy makers may use these cost-offset findings to support parity legislation but should be cautioned that treatment need and cost-effectiveness are more appropriate parameters for justifying behavioral health care. Primary Funding Source: SAMHSA/CMHS • The Association Between Federal Block Grants and Individual Mental Health and Substance Abuse Expenditures Alexander Cowell, Ph.D., Jeremy Bray, Ph.D. Presented by: Alexander Cowell, Ph.D., Research Economist, Health, Social, and Economics Research, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: 919.541.8754; Fax: 919.541.6683; E-mail: cowell@rti.org Research Objective: Considerable public resources are spent on mental health and substance abuse - MH/SA. One key mechanism by which the federal government addresses MH/SA needs among the population is the substance abuse and mental health block grants, which provide annual grants to states. Despite the block grants being a primary source of funding to address MH/SA needs, the impact of such public expenditures and policies on individual behavior has received little attention in the literature. To help address this research gap, this project uses data from several sources to assess the impact of the substance abuse and mental health block grants on individual mental health and substance abuse - MH/SA expenditures. Study Design: We conduct secondary data analysis using administrative claims from the private sector for 1997 matched with data containing a comprehensive list of policy variables. MarketScan data provide information on plan characteristics, key demographics, and MH/SA expenditures for over 380,000 claimants with private, fee-for-service insurance. Matched to these individual data are several policy-relevant state-level variables measuring: the amounts of the federal substance abuse block grant and the mental health block grant; statutory state fines and jail terms for marijuana possession; cigarette and beer taxes; and adult and juvenile crime rates per thousand population by type of crime. Regression analysis is used to examine the impact of the two types of block grant on whether individuals seek MH/SA care and on MH/SA expenditures, conditional on seeking care. Population Studied: This study focuses on adults covered by private sector fee-for-service insurance plans. Principal Findings: Results indicate that individuals are very responsive to changes in both the mental health and substance abuse block grants. The results also indicate that the response to mental health block grants can be very different from the response to substance abuse block grants. Conclusions: The federal government relies heavily on two types of block grant – the mental health block grant and the substance abuse block grant – to help deliver services to those in need. This paper represents the first research that examines how these important funding mechanisms affect the use of MH/SA care. The findings indicate that both kinds of block grants affect individual decisions and utilization of MH/SA care. Simulations indicate that a 10 percent increase in the mental health block grant is associated with a 14.1 percent increase in the likelihood of using MH/SA care, but a total decrease in MH/SA payments of approximately $22 million. A 10 percent increase in the substance abuse block grant is associated with a 19.8 percent decrease in MH/SA care and a total increase on MH/SA payments of about $4 million. Implications for Policy, Delivery or Practice: The findings indicate that the block grant mechanisms operating in the public domain have spill-over effects on MH/SA utilization in the private domain. Primary Funding Source: SAMHSA/CMHS • Effect of Managed Care on Treatment Costs for a Medicaid Population with Psychiatric Disabilities Kristine Jones, Ph.D., Neil Jordan, Ph.D., Huey Jen Chen, Ph.D., Roger Boothroyd, Ph.D., David Shern, Ph.D. Presented by: Neil Jordan, Ph.D., Assistant Professor, Mental Health Law & Policy, University of South Florida, 13301 Bruce B Downs Boulevard, MHC 2713, Tampa, FL 33612; Tel: 813.974.9243; Fax: 813.974.9327; E-mail: njordan@fmhi.usf.edu Research Objective: To examine the effects of differing financial risk arrangements for health, mental health and pharmacy services on the costs of these services and on total social costs, with particular attention to cost containment and cost shifting for individuals with severe mental illness. Study Design: Study subjects were interviewed bi-monthly for 15 months following enrollment. Comprehensive service utilization data were collected, including information about mental health, substance abuse, physical health, pharmacy, and social and other human services (e.g., corrections) provided by both formal and informal providers, and on and off of the Medicaid budget. Administrative data were used to validate and supplement the self-report data. Details on providers allowed us to investigate the differences among financing conditions in the overall distribution of financial burden between formal and informal providers, among sectors (health, pharmacy, social services, etc.) and payors. Rate information was used to calculate costs, and a two-part regression model was employed to test for differences among risk conditions. Population Studied: Study subjects were adults with severe mental illness (SMI) who received Medicaid Supplemental Security Income benefits (n=630). Collectively, 72% of the subjects were women, they averaged 42 years old, and were 47% white, 32% Black, and 15% Hispanic. Given this was an observational study and did not involve random assignment, there were some differences found across the three financing arrangements with respect to subject demographics. Subjects were enrolled in either a fee-for-service (FFS), carvein, or mental health carve-out plan. In the FFS arrangement, all enrollees’ health, mental health, and pharmacy services were paid on a fee-for-service basis with no financial risk to providers. In the carve-in arrangement all enrollees’ health, mental health and pharmacy services were paid using a capitated per member per month (PMPM) payment, with providers bearing full risk for these services. In the mental health carve-out arrangement, all enrollees’ mental health services were paid using a PMPM capitated rate while their health and pharmacy services were paid on a fee-for-service, non–risk basis. Principal Findings: Total treatment costs were found to significantly vary depending on risk arrangements. Differential pharmacy costs were principally responsible for these differences. No differences in total social costs were found between conditions, with individuals in the conditions with financial risk showing a relatively greater use of out of plan and informal resources than persons in the FFS condition. Conclusions: Financial risk is significantly related to access to pharmaceuticals in this sample of Medicaid recipients with severe mental illness. There was modest evidence of cost shifting for persons in managed care plans, with greater financial risk associated with greater off-plan costs. Implications for Policy, Delivery or Practice: When evaluating the impact of Medicaid managed care on access and cost of services for persons with SMI, it is important to use a societal perspective because overall cost savings within health budgets may be offset by other social costs. Primary Funding Source: , Substance Abuse and Mental Health Services Administration (Grant # 5 UR7 TI11278) Related Posters Poster Session B Tuesday, June 8 • 7:30 a.m.-8:45 a.m. • Physicians’ Diagnoses Associated with Antidepressant Use between 1995 and 2001 Ayse Akincigil, Ph.D., Benjamin Druss, M.D., M.P.H., John Bowblis, M.A., Stephen Crystal, Ph.D. Presented by: Ayse Akincigil, Ph.D., Research Associate, Institute for Health, Health Care Policy and Aging Research, Rutgers, The State University of New Jersey, 30 College Avenue, New Brunswick, NJ 08901; Tel: 732.932.5348; Fax: 732.932.8592; E-mail: aakinci@rci.rutgers.edu Research Objective: Describe the trends in clinical diagnoses underlying the prescription of antidepressant. Study Design: Cross sectional data from National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, 1995 to 2001, a nationally representative sample of ambulatory care providers in physician offices and hospital outpatient departments. Population Studied: Patients aged 18 or older, who were prescribed antidepressants. Principal Findings: In 1995, antidepressants were prescribed at 5.5% of visits, compared to 8.5% in 2001. Of those receiving antidepressants, 39% were diagnosed with depression, 5% with anxiety, 12% with some other mental illness (including bipolar and schizophrenia), and 44% had no primary or secondary diagnosis of mental illness In 1995, 10 million antidepressant prescriptions were written without any diagnosis of mental illness, rising to 23 million in 2001. The most common diagnoses other than mental disorders for visits at which antidepressants were prescribed were diseases of the circulatory system (25%), chronic joint pain (16%), diabetes (9%), chronic back or neck pain (8%), migraine or headaches (7%), and cancer (6%). Conclusions: The prescription of antidepressants rose sharply between 1995 and 2001. Use without a diagnosis of depression or other mental disorder increased even faster during the period. Implications for Policy, Delivery or Practice: The rising rate of use of antidepressants in patients without mental diagnoses suggests either rising off-label use of these treatments for other conditions, or else their use for unreported (e.g., subsyndromal) mental problems. Under either scenario, there appears to be a widening use of antidepressants beyond populations for whom they have been shown to be effective. Primary Funding Source: NIMH, AHSR • Employing Community-Based Research Methods to Describe the Process of Competitive Employment for Persons with Serious Mental Illness Marjorie Baldwin, Ph.D., Rebecca White, M.P.H. Presented by: Marjorie Baldwin, Ph.D., Professor, School of Health Administration & Policy, W. P. Carey School of Business, Arizona State University, Box 4506, Tempe, AZ 85287-4506; Tel: 480.965.7868; Fax: 480.965.6654; E-mail: Marjorie.Baldwin@asu.edu Research Objective: This work applies community-based participatory research methods to develop a comprehensive model of mental illness and work disability. The research objective is to identify important determinants of employment outcomes for persons with serious mental illness that are not currently measured, or measurable, on national survey data. Study Design: The study uses qualitative, community-based methods to assess the experiences of persons with mental illness in the competitive workplace and identify factors that facilitate or impede success in competitive jobs. In the first phase a series of focus groups was conducted with mental health professionals. In the second phase individual semistructured interviews were conducted with employers and mental health services consumers. The researchers assessed how illness characteristics, individual characteristics, family and community characteristics, productivity-related characteristics, and work-related characteristics affect employment outcomes for this population. Population Studied: This research targeted three stakeholder groups: (1) mental health services professionals, (2) supervisors and managers who have hired or employed a person with mental illness, and (3) persons with serious mental illness who are working or trying to work in competitive employment and living in the community. Principal Findings: The information obtained through interviews and focus groups paints a rich picture of a range of employment experiences. Many persons with even the most serious mental illnesses are working. Persons with mental illness work in the full spectrum of jobs, ranging from professional to service to unskilled laborer positions. Important characteristics related to the individual, his or her illness, family and community support systems, productivity, and work environment have been identified as factors that may influence employment outcomes for this population. Conclusions: Although there are a number of studies of persons with mental disorders in transitional or supported employment settings, this is the first study to provide in-depth analyses of the experience of persons with mental disorders in the competitive labor market. Developing and testing a comprehensive model of mental illness and work disability is a fundamental step toward advancing mental health services by recognizing employment as a primary component of the recovery process. Implications for Policy, Delivery or Practice: While national surveys have examined issues related to competitive employment, mental health issues have been given only cursory attention, possibly because no one knows the right questions to ask, or because it is assumed that persons with serious mental disorders are unable to work. This study helps to identify the concepts that need to be measured to support a more comprehensive analysis of persons with mental disorders in the workplace. The results will inform the development of a survey instrument that will be used to obtain sufficient data, with adequate samples of persons with different types of mental disorders, to support a comprehensive analysis of the important determinants of labor market outcomes for persons with serious mental illness. Potentially, the findings will contribute to improving employment outcomes for future generations of persons with mental illness who want to work. Primary Funding Source: Office of Research and Sponsored Projects Administration, Arizona State University • Health Services for Women in Outpatient Substance Abuse Treatment Cynthia Campbell, Ph.D., M.P.H., Jeffrey Alexander, Ph.D. Presented by: Cynthia Campbell, Ph.D., M.P.H., Postdoctoral Fellow, Psychiatry/Division of Research, UCSF/Kaiser Permanente, 2000 Broadway, 3rd Floor, Oakland, CA 94612; Tel: 510.891.3584; Fax: 510.891.3606; E-mail: cynthia.i.campbell@kp.org Research Objective: Research suggests that gender-sensitive services can positively influence outcomes for women in substance abuse treatment, yet some treatment organizations fail to provide services that are sensitive to women's needs. This study evaluates how a sample of outpatient substance abuse treatment units respond to organizational and environmental influences by adopting and implementing health services for women. Study Design: A national sample of outpatient drug abuse treatment units were surveyed in 1995 and 2000 about their organizational structure and treatment practices. The dependent variables in this paper are health services for women in substance abuse treatment. The predictors include organizational and environmental factors that represent resource dependence and institutional pressures for the treatment unit. Logistic regression and Heckman selection models were used to test study hypotheses. Population Studied: The program directors and clinical supervisors at each treatment unit, who were interviewed by telephone in 1995 and 2000. Principal Findings: Units that depended on specific funding for women’s programs and that depended on government funds were more likely to adopt, but not necessarily implement, women’s services. Methadone units and units that train more staff to work with female clients were more likely to adopt as well as implement women’s services. Private not-for-profit units were more likely to adopt some services, while for-profit units were less so. However, in general, neither for-profit or not-for-profit unit significantly implemented services. There was evidence that the odds of adopting services were greater in 2000 than 1995 for two services, but were otherwise stable. Conclusions: There is considerable variation in the adoption and implementation of women’s services. In addition, not all adopted services were significantly implemented, which could reflect limited organizational resources and/or conflicting expectations. This also suggests that referral mechanisms to these services, and therefore access, may not be adequate. Government funds and specific funds for women’s programs are important resources for the provision of these services. Women’s services appear more available in methadone units, suggesting that regulation has been influential and that the recent methadone accreditation system should be evaluated. Staff training may be one strategy to encourage implementation of these services. For the most part, the adoption of services for women did not change between 1995 and 2000. Implications for Policy, Delivery or Practice: Health services for women in substance abuse treatment can be important for improving outcomes, yet we know little about the factors that lead to the provision of these services. This study found that continued government funding is critical for adoption. In addition, efforts to develop and strengthen linkages to other resources specifically for women’s services should be undertaken. One option to encourage implementation of services is to train staff to work with female clients. JCAHO accreditation could also be useful for improving treatment if the criteria were broadened to include women’s services. While overall there were no decreases in the level of services, it is quite possible that the effects of lower federal funding have not yet become apparent and this should be monitored in the future. Primary Funding Source: NIDA • Concept Mapping for Mental Health Services Evaluation and Planning: Results from a Project Involving Providers, Consumers, and Family Caregivers Edie Cook, M.S., ABD Presented by: Edie Cook, M.S., ABD, Evaluation Specialist, Graduate School of Public Health; Center of Public Health Practice, University of Pittsburgh, 3109 Forbes Avenue, Pittsburgh, PA 15260; Tel: 412.383.2400; 412.383.2883; Fax: 412.383.2228; E-mail: cooke@edc.pitt.edu Research Objective: To enhance the quality of comprehensive mental health services planning through an increased involvement of hospital and community providers, consumers, and family caregivers in the evaluation of mental health treatment. The Psychiatric Services Planning Project was implemented as a collaborative effort to improve transition from hospital to community mental health services. Study Design: Concept mapping (Trochim, 1989) consists of a graphical representation of multidimensional scaling and cluster analyses of group sorting and rating tasks and was chosen as an innovative tool to facilitate understanding between groups. Participant groups were actively involved in all four phases in the project: 1) the development of a classification of area mental health services, 2) provider, consumer, and family caregiver interpretation of data represented by concept maps, 3) recommendations for improvement, and, 3) a prioritization of focus areas for further evaluation research. Population Studied: Participant groups were comprised of thirty-two psychiatric hospital staff, twenty-seven community mental health service providers, thirty-three consumers of mental health services, and eighteen family caregivers of adults with chronic mental illness. Principal Findings: Concept Mapping yielded graphical representations which were helpful during all phases of the project, but was particularly useful for developing a classification of area mental health services due to use of cluster analysis and labeling of clusters in individual group interpretation sessions. Recommendations from consumers for improvement reflected a desire for increased educational opportunities and greater independence, and family caregivers focused on discharge planning, medication management, and family rights to information. The prioritization method piloted in this study generated patient aftercare, family education, and relapse prevention as the three top focus areas for further evaluation attention. Conclusions: Concept mapping can be a useful tool for facilitating the involvement of multiple stakeholders in a single study or evaluation project. The data derived through the concept mapping activities and analyses were used in the development of a classification of mental health services as well as in program evaluation and treatment quality improvement. Implications for Policy, Delivery or Practice: Health service planners and policy makers may want to consider concept mapping for evaluation and planning projects which involve multiple stakeholders, whether they represent different disciplines of hospital staff, or community and agency providers. Projects which call for modeling consumer and family caregiver perceived treatment needs, or for conceptualizing aspects involving care or treatment delivery would benefit from the visual representation of data that concept mapping provides. Primary Funding Source: Mayo Clinic Psychiatry and Psychology Department • Effect of Medicaid Managed Care on Somatic Health Care Utilization for Adults with Severe and Persistent Mental Illness in Maryland Gail Daumit, M.D., M.H.S., Wenke Hwang, Ph.D., Christopher Anthony, Anthony Lehman, M.D., Donald Steinwachs, Ph.D. Presented by: Gail Daumit, M.D., M.H.S., Assistant Professor of Medicine, Johns Hopkins University School of Medicine, 2024 East Monument Street, Suite 2-500, Baltimore, MD 21205; Tel: 410.614.6460; Fax: 410.614.0588; E-mail: gdaumit@jhmi.edu Research Objective: Individuals with severe and persistent mental illnesses such as schizophrenia and bipolar disorder have a high burdenof medical comorbid disease, and they often receive health insurance benefits through Medicaid, Medicare or both. Beginning in 1997, Maryland capitated somatic health care services for those Medicaid recipients without Medicare coverage while maintaining mental health services in fee-for-service. Reciepients with dual coverage remained in fee-for-service Medicaid for both somatic and mental health care. Effects of Medicaid managed care on medical service utilization for vulnerable, disabled populations are understudied. This policy change provided a natural experiment to examine if the transition to managed care had any adverse impact on utilization and quality of somatic health care for individuals with severe mental illness in Maryland Study Design: We performed a cohort study of Maryland Medicaid recipients with severe and persistent mental illness before (1996) and after (2000) implementation of Medicaid managed care for somatic care.Participants without Medicare dual coverage had managed Medicaid in 2000. Our primary outcomes were hospitalizations and emergency department visits for medical diagnoses and hospitalizations for ambulatory sensitive conditions. We calculated outcomes per person-time adjusting for age, race and gender of recipients, and also performed multiple logistic regression using generalized estimating equations to account for events per individual in different years. Population Studied: Two-thousand eight hundred seventynine adult Maryland Medicaid recipients with schizophrenia or bipolar disorder identified in 1994 and followed through 2000. Principal Findings: The mean age was 43.3 years; 49% were women, 42% were African American, and 89% lived in an urban area. Seventy percent had schizophrenia; 32% had Medicare and Medicaid dual coverage. The following analyses are adjusted for age, race, gender and person-years of followup. In 1996, participants with Medicare/Medicaid had 0.87 (95% CI, 0.78-0.95) medical emergency department (ED) visits/person-year; participants with Medicaid had 0.91 (95%CI, 0.83-1.00) visits/person-year. In 2000, participants with Medicare/Medicaid had 0.70 (95% CI, 0.63-0.78) medical ED visits/person-year; participants with Medicaid managed care had 0.75 (95%CI, 0.68-0.83) visits/person-year. In 1996, participants with Medicare/Medicaid had 0.28 (95% CI, 0.240.32) medical hospitalizations/person-year; participants with Medicaid had 0.29 (95%CI, 0.26-0.33) per person-year. In 2000, participants with Medicare/Medicaid had 0.22 (95% CI, 0.18-0.25) medical hospitalizations /person-year; participants with Medicaid managed care had 0.22 (95%CI, 0.18-0.25) per person-year. In multivariate analyses adjusted for sociodemographic and clinical characteristics, the relative odds of any medical ED visit were 0.82 (95% CI 0.67-0.99) for participants in Medicaid managed care compared to those not in Medicaid managed care. The adjusted relative odds of any medical hospitalization were lower in 2000 (OR 0.74, 95% CI 0.56-0.97) than in 1996. Participants’ ambulatory sensitive admissions remained constant at 0.05 (95% CI 0.042-0.060) per person-year from 1996 to 2000 in both Medicaid and Medicare/Medicaid in 1996 and 2000. Conclusions: These Medicaid recipients with severe mental illness had high levels of acute care utilization. We found lower medical emergency department utilization with transition to Medicaid managed care. Medical hospitalizations decreased from 1996 to 2000 for both managed care and feefor-service programs. Rates of ambulatory sensitive hospitalizations remained high. Implications for Policy, Delivery or Practice: Medicaid managed care in Maryland may have contributed to a reduction in use of the medical emergency department for recipients with severe and persistent mental illness. While it is reassuring that admissions for ambulatory sensitive conditions did not increase, the level of these admissions is relatively high compared to non-disabled populations. Future work should examine the effect of Medicaid managed care on outpatient health utilization for this vulnerable population. Primary Funding Source: NIMH • Substance Abuse Treatment among Opioid Pain Medication Users with Private Insurance Andrea DeVries, Ph.D., Katherine Harris, Ph.D., Kelli Dimidjian, M.B.A., Brian Day, Ed.D Presented by: Andrea DeVries, Ph.D., Head of Health Services Research, Healthcare Informatics, Research & Analysis, Highmark Blue Shield, 120 Fifth Avenue, Suite P7250, Pittsburgh, PA 15222-3099; Tel: 412.544.0794; Fax: 412.544.0700; E-mail: andrea.devries@highmark.com Research Objective: To (1) determine whether frequent users of opioid pain medication have an increased likelihood of seeking substance abuse treatment. (2) identify the proportion of pain medication users who have a history of behavioral health problems. (3) identify the extent to which a history of behavioral health problems increases the likelihood for substance abuse treatment among pain medication users. Study Design: Medical and pharmacy claims data are analyzed for a large insured population over a two-year period. Members with frequent opioid pain medication use are identified, where “frequent use” is defined as a >90 day supply in a 12 month period. Substance abuse treatment rates among the pain medication users are compared to general population treatment rates for this same period, adjusted by age and gender. Among the pain medication users, members with a recent history of behavioral health problems are identified, where ‘recent history’ is defined by either mental health or substance abuse services provided during the preceeding 12 month period. The rates of substance abuse treatment among pain medication users with a recent history of behavioral health problems are calculated separately. Population Studied: The population is drawn from a large mid-Atlantic health insurer with more than 3 million members enrolled in a range of insurance products. We analyzed the subpopulation of 1.5 million members between the ages of 18 and 65 with both prescription drug and behavioral health benefits provided through the health plan. There were 22,529 individuals identified as being frequent users of opioid pain medication. Principal Findings: Preliminary analyses suggest that members with frequent use of opioid pain medication had higher rates of substance abuse treatment. The pain medication users were 5 times more likely to receive substance abuse treatment services as compared to the general health plan population. Pain medication users with a recent history of behavioral health problems were 15 times more likely to receive substance abuse treatment services as compared to the general health plan population. Members with a recent history of behavioral health problems represented 17% of the total pain medication users and 47% of pain users receiving substance abuse treatment services. Conclusions: Our results are consistent with recent studies suggesting that official statistics underestimate the problem of addiction to prescription pain medication. However, a patient population with vulnerability to addiction may be responsible for the observed higher treatment rates. Individuals with a history of substance abuse disorders and mental health problems comprise a disproportionate share of individuals who frequently use opioid pain medications. Implications for Policy, Delivery or Practice: When prescribing opioid pain medication providers should screen for risk factors that would increase the likelihood of misuse and indicate history of untreated or inadequately treated behavioral health problems. Recognition and treatment of comorbid mental health problems may reduce the likelihood of pain medication misuse. Future research is needed on the relationship between chronic pain, mental health disorders, and vulnerability to addiction. • Work Disability and Barriers to Evidence-Based Psychosocial Treatments Farifteh Duffy, Ph.D., Joyce West, Ph.D., M.P.P., William Narrow, M.D., M.P.H., Ilze Ruditis, M.S.W., Lisa Countis, Darrel Regier, M.D., M.P.H. Presented by: Farifteh Duffy, Ph.D., Research Scientist, , American Psychiatric Institute for Research & Education, 1000 Wilson Boulevard, Suite 1825, Arlington, VA 22209; Tel: 703.907.8620; Fax: 703.907.1087; E-mail: fduffy@psych.org Research Objective: Disabilities associated with mental disorders are equally or more debilitating than those associated with chronic general medical conditions (Von Korff 1994, Wells et al., 1989). This study examines: 1) rates and correlates of work-disability among adult psychiatric patients; and 2) rates and correlates of receiving psychosocial services (i.e., vocational rehabilitation, social-skills training, and casemanagement services) among work-disabled patients. Study Design: Cross-sectional observational data from the 1999 American Psychiatric Practice Research Network (PRN) Study of Psychiatric Patients and Treatments (SPPT) were used. A national sample of 1,596 psychiatric patients 18 years of age or older (median age=44) were systematically selected by 615 psychiatrist-members of the American Psychiatric Practice Research Network (PRN). Data were weighted to provide nationally representative estimates. Population Studied: Adult psychiatric patients (n=1596); approximately 43% of patients were male; 79% white, 10% African American, and 7% Hispanic. Principal Findings: 33% of patients were not working due to disability (i.e., work-disabled). Only 15% of the work-disabled patients received any vocational rehabilitation (1.1%), social skills training (4.9%), or case management (12.4%) services within a 30-day period. Highest rates of work-disability were observed among patients with: schizophrenia (67%), substance use (43%), and bipolar (40%) disorders although substantial levels of disability were also found in patients with personality (34%), anxiety (26%) and depressive (24%) disorders. Multiple logistic regression analyses indicated patients with schizophrenia, co-occurring general medical conditions, multiple psychosocial problems, public insurance, older age, and less education were more likely to be workdisabled. Among work-disabled patients, those with schizophrenia, Axis II comorbidity, and public insurance were more likely to receive any of the aforementioned psychosocial services. Conclusions: One out of every three adult psychiatric patients treated by psychiatrist is reported to be work-disabled, yet only one out of every seven work-disabled patients received any psychosocial services. Socioeconomically disadvantaged patients and patients with clinically complex conditions were more likely to be work-disabled, and were more likely to receive psychosocial services. Implications for Policy, Delivery or Practice: This study highlights a number of patient subgroups at increased risk for work-disability. Despite evidence in support of psychosocial services for persons with serious mental illness (Surgeon General’s Report 1999, PORT 2002, Bond et al. 2001), our findings indicate only a small minority of work-disabled patients received any vocational rehabilitation, social skills training, or case management services (15%). Although not every work-disabled individual would require, seek, or benefit from psychosocial interventions (depending on duration and severity of the person’s disability), models of service delivery which aim to improve the coordination and integration of services and strive toward the provision of individually-tailored treatment programs are critical to meet the needs of persons with work-disability. Current health care financing and services delivery policies and interventions, however, need to address the gaps in insurance coverage and enhance the organization and financing of services that are considered major barriers to access (Surgeon General’s Report 1999). Primary Funding Source: , The Center for Mental Health Services, the American Psychiatric Foundation, the Center for Substance Abuse Treatment, and the John D. and Catherine T. MacArthur Foundation. • An Examination of ED Psychiatric Consultation Arrangements Jennifer Field, B.A., B.S.N., M.S.N., Ph.D. Candidate Presented by: Jennifer Field, B.A., B.S.N., M.S.N., Ph.D. Candidate, Psychiatric Clinical Nurse Specialist, Health Administration, Virginia Commonwealth University, 718 Greensboro Avenue, Virginia Beach, VA 23451; Tel: 757.491.7985; E-mail: jlfield@hsc.vcu.edu Research Objective: The purpose of this study was to examine the degree to which environmental and economic factors affect an emergency department's psychiatric consultation arrangement and how arrangement influences service effectiveness. It answers two questions: 1) What factors lead hospitals to create an emergency department psychiatric consultation service, to purchase the services from an outsider, or to not provide the service? 2) Does variation in the consultation arrangement have a significant impact on service outcomes Study Design: The study utilizes a balanced cross-sectional design. It retrospectively examines hospital ED psychiatric service arrangements and outcomes. It uses a combination of primary and secondary data gathered from several sources. ED encounter data was obtained from two state ambulatory care and inpatient databases (Maryland and South Carolina). America Hospital Association and Area Resource File databases provided information on facility characteristics. A survey of ED administrators from the participating facilities was conducted to capture information about facility psychiatric consultation arrangements. Regression and multilevel structural equation modeling were the chosen methods of analysis. Population Studied: The target sample included all nonfederal acute care medical-surgical hospitals that have emergency departments in South Carolina and Maryland (N=102). Seventy-one facilities responded to the survey resulting in a 69.6% response rate. Respondents were categorized by type of PES arrangement (in-house, contract, or no service) and this characteristic was the focus of subsequent analysis. Data from 66 randomly selected ED psychiatric patients was drawn from each participating hospital yielding a sample N=71*66=4686. Principal Findings: The hypotheses were derived from a conceptual model based upon the principles of transaction cost economics (TCE). The model proposes that organizations choose the arrangement that incurs the lowest transaction costs, which are determined by the degree of environmental and behavioral uncertainty, asset specificity, and transaction frequency. The results support each TCE construct as a statistically significant predictor of arrangement; however, not all indicators demonstrated the predicted relationships. In addition, the conceptual model proposed that arrangement influences outcomes (time, disposition, readmission, and cost). The results demonstrated arrangement significantly affected outcomes but only partially supported the proposition that vertically integrated services are associated with more positive outcomes. Conclusions: The results support the application of TCE theory to explain ED psychiatric service variation and provide new information about the effects of arrangement on outcomes. Implications for Policy, Delivery or Practice: The study confirms that variation in ED psychiatric consultation arrangement exists and has an influence on outcomes. Hospital administrators, accrediting organizations and insurers should explore this further to confirm the conditions and type of arrangement that are necessary to produce the most promising outcomes for the patient and organization. Policy makers and accreditors may want to impose guidelines that reduce variation in effort to create more comparable units for evaluation. Health insurers could use the findings as performance criteria for network selection. Finally, this study represents the creative merging of multiple data sources to develop a comprehensive portrayal of psychiatric service utilization. It demonstrates the utility of state ambulatory service data encouraging future use of an HCUP emergency service database currently under development. Primary Funding Source: AHRQ • Mental Illness, Traumatic Brain Injury, and Medicaid Expenditures Wenhui Wei, M.A., M.S., Patricia Findley, Dr.PH, M.S.W., Usha Sambamoorthi, Ph.D., Stephen Crystal, Ph.D. Presented by: Patricia Findley, Dr.PH, M.S.W., Asst Research Professor, Program for Disability Research, Rutgers University, 303 George Street, New Brunswick, NJ 08901; Tel: 732.932.3421; Fax: 732.932.1894; E-mail: pfindley@rci.rutgers.edu Research Objective: Use Medicaid administrative data to analyze variations in rates of mental illness and annual Medicaid expenditures for individuals with diagnosed traumatic brain injury (TBI) by their sociodemographic and health characteristics Study Design: The study used personal summary information and paid Medicaid claims data from State Medicaid Research files for Alabama, Georgia, New Jersey, and Wisconsin. Annual expenditures for total, inpatient, and non-inpatient services were derived from personal summary files. Mental illness and TBI were derived based on International Classification of Diseases 9th revision, Clinical Modification codes recorded in paid Medicaid claims. Chi-square statistics were used to test for subgroup differences in the proportion of individuals with TBI and mental illness. Kaplan-Meier survival techniques were used to estimate annual expenditures for different types of services and t-tests were used to test the statistical significance of bivariate subgroup differences in annual and monthly expenditures. Finally, Ordinary Least Squares regression was used on average monthly expenditures, and Cox-Proportional Hazards regression was used on annual expenditures to determine the extent to which differences in mental illness account for variations in Medicaid expenditures. The extrapolation of results into current Medicaid policy on programs with for individuals with TBI was considered. Population Studied: Continuously enrolled Medicaid recipients who were aged 21-64 and diagnosed with TBI in 1995. Principal Findings: Overall, less than 1% (n = 4,266) were diagnosed with TBI in four states in 1995. Significant geographic, demographic, racial, and health status differences were found in the rates of TBI. Among those diagnosed with TBI, a majority (67%) did not have a diagnosis of mental illness and 17% were diagnosed with serious mental illness. Individuals in the age group 40 – 49 years, racial minorities other than African American and Latinos, diagnosed with substance abuse, and burdened with chronic comorbidity were more likely to have a mental disorder. Significant differences in estimated total, inpatient and non-inpatient expenditures by mental illness were also noted. In general, those with serious mental illness had higher expenditures than those with out any mental illness. Additionally, the presence of high burden of chronic comorbidity significantly increased the overall expenses, most significantly for inpatient expenses. Conclusions: This study found that expenditures, although variable across service types, are generally higher for those with TBI and severe mental illness. This suggests the overall need for general awareness that differences do exist in the expenditures for the dual diagnosis, and that this should be considered in programming and budget planning, particularly for tightly budgeted programs like State Medicaid programs. Implications for Policy, Delivery or Practice: Future Medicaid policy modifications need to take into consideration the health and mental health care needs of this duallydiagnosed subpopulation, particularly in aspects that address home and community based programs. Primary Funding Source: NIMH, National Insitute of Child Health and Human Development • Satisfaction of Impaired Health Care Professionals with Mandatory Treatment and Monitoring Carol Fletcher, Ph.D., R.N., David Ronis, Ph.D. Presented by: Carol Fletcher, Ph.D., R.N., Research Specialist, Center for Practice Management and Outcomes Research, Veterans Health Administration, Box 130170, Ann Arbor, MI 48113-0170; Tel: 734.769.7100 Ext. 6212; Fax: 734.761.2617; Email: carol.fletcher@med.va.gov Research Objective: To determine the level of satisfaction of active participants mandated into the Michigan Health Professional Recovery Program, HPRP, and the Indiana State Nurses Assitance Program, ISNAP. Study Design: Mailed surveys were used to assess overall program satisfaction, the usefulness of various aspects of monitoring, several miscellaneous items, e.g., insurance coverage and whether the person was currently working in a position requiring licensure, and basic demographics. Mailed responses, n=263, 43% for the HPRP; n=120, 45% for ISNAP, were anonymous. Population Studied: All active participants in the HPRP, n=620, and ISNAP, n=267, programs in July 2002. The HPRP covers >300,000 persons in 19 professions including physicians, nurses, pharmacists and dentists. ISNAP covers >100,000 nurses. Principal Findings: Means on the 1 to 5 satisfaction scale were 3.6, SD=.94, for the HPRP and 4.1, SD=.86, for ISNAP, indicating overall satisfaction with the programs. Means on the 1 to 4 monitoring scale were 2.7, SD=.62, for the HPRP and 2.7, SD=.57, for ISNAP, indicating most aspects of monitoring were considered useful. 40% of HPRP respondents and 53% of ISNAP respondents lacked any insurance coverage for program costs. 39% of HPRP and 35% of ISNAP respondents stated they had substance abuse or mental health difficulties prior to their professional career. Conclusions: Although 20% or less of the HPRP and ISNAP participants come into the programs by their own choice, respondents appear to be generally satisfied with these mandatory programs once they become involved. Implications for Policy, Delivery or Practice: Maintaining patient safety by ensuring health professionals continuing competency to practice is essential. Impaired professionals can be mandated into treatment, but true success depends upon their willingness to follow the program. Satisfied persons are more likely to truly cooperate. This study demonstrates that it is possible to create satisfaction with mandated programs. Primary Funding Source: Michigan Health Professional Recovery Corporation • Outpatient Mental Health Service Use: Racial and Ethnic Variations? Nell Forge, Ph.D., M.P.H., M. Audrey Burnam, Ph.D., Cathy Donald Sherbourne, Ph.D. Presented by: Nell Forge, Ph.D., M.P.H., Associate Behavioral Scientist, Health, RAND, 1700 Main Street, Santa Monica, CA 90056; Tel: 310.393.0411; Fax: 310.451.7063; E-mail: Nell_Forge@rand.org Research Objective: To examine whether there is any racial and ethnic variation in the use of outpatient mental health services and to identify pathways to mental health service use among a national sample of HIV-infected individuals. Study Design: This study draws upon baseline data from the HIV Cost and Services Utilization Study, a national longitudinal survey of HIV-infected adults receiving HIV care. Logistic regression models estimated the effect of race and ethnicity on likelihood of mental health service utilization. Population Studied: The analytic sample is comprised of individuals who have a need for mental health services. Principal Findings: Whites were more likely to receive psychotropic medications, whereas African Americans were more likely to use mental health support groups. Perception of mental health need was a robust pathway to mental health services, whereas financial and knowledge-related barriers decreased likelihood of use. Conclusions: Gaps continue to exist in psychotropic medication even among racial groups who were receiving care for their HIV status. Implications for Policy, Delivery or Practice: Increasing knowledge of mental health need, coupled with providing financial mechanisms to access care are needed to address racial variation in mental health service use. Primary Funding Source: NIMH • Translation and Adaptation of a Mental Health Outcome Measure Susan Eisen, Ph.D., Mariana Gerena, M.A., Dharma Cortes, Ph.D., Mariana Gerena, M.A., Glorisa Canino, Ph.D., Sergio Aguilar-Gaxiola, M.D., Ph.D., Cristina Magana, Ph.D. Presented by: Mariana Gerena, M.A., , Center for Health Quality, Outcomes and Economic Research (CHQOER), EN Rogers Memorial Veterans Hospital, 200 Springs Road (152), Bedford, MA 02464; Tel: 781.687.3257; Fax: 781-687-3106; Email: gerena@bu.edu Research Objective: To develop a culturally and linguistically appropriate mental health assessment instrument to assess outcome of treatment for Spanish-speaking mental health and substance abuse service recipients. Culturally and linguistically appropriate outcome measures are especially needed to determine the presence and direction of health disparities, and to assess quality and outcomes of treatment among minority populations. Clinical outcome is widely recognized as an important indicator of the quality and effectiveness of mental health care. However, due to a dearth of mental health outcome assessment instruments that have been translated and validated, Spanish-speaking mental health consumers are often excluded from efforts to assess treatment outcomes. Study Design: This study is using qualitative and quantitative methods to adapt, translate, field test and validate the revised Behavior and Symptom Identification Scale (BASIS-R), a mental health instrument developed on English speakers in the United States. The translation and adaptation used addresses key dimensions of cross-cultural equivalence: content, semantic, technical, criterion and concept equivalence. This presentation summarizes results of the qualitative methods. A professional translator provided a preliminary Spanish translation of the instrument, which was back-translated by a second translator, then reviewed by a multi-national bilingual committee. Focus groups and individual cognitive interviews were conducted to obtain feedback about the content and format of the instrument, and to assess respondents’ understanding of the instructions, questionnaire items, time frame and response options. Respondents’ ratings of clarity and importance of each item were also obtained. Population Studied: The sample consisted of Spanishspeaking, adult mental health service recipients from three regions, Boston, Fresno and San Juan, who are of Dominican, Mexican or Puerto Rican origin. Thirty-six individuals participated in one of four focus groups, and 45 individuals participated in cognitive interviews. Principal Findings: Analysis of focus group data identified a number of items reported to be confusing or difficult for participants. These were deleted or re-worded to clarify or simplify them prior to conducting cognitive interviews. Analysis of the cognitive interviews indicated that 22 out of 26 items tested were rated as completely clear by at least 80% of respondents and 24 out of 26 items were rated as very important by at least 80% of respondents. Respondents’ qualitative explanation of item meaning did not always correspond with their rating of item clarity. Thus the qualitative explanations of item meaning were important in supplementing ratings of clarity. Several “psychosis” items were identified by Latino participants as ordinary experience within their culture and religious beliefs, and consequently, are not necessarily indicative of psychosis in a Spanish-speaking population (e.g., “hearing voices or seeing things,” and “having special powers”). Conclusions: The combined use of qualitative and quantitative methods is important for determining crosscultural equivalence of mental health assessment instruments. Implications for Policy, Delivery or Practice: Assessment instruments developed on Anglo populations may not be generalizable to minority groups. Use of inappropriate instruments may lead to erroneous conclusions about mental health status or outcomes. Consequently, assessment instruments should be adapted, tested and validated when used to assess individuals from other countries or cultures. Primary Funding Source: NIMH • Automating Clinical Practice Guidelines for Tobacco Use Cessation – The 5 A’s: Ask, Assess, Advise, Assist and Arrange Jack Green, M.B.A., B.S., James Chesney, Ph.D., Patricia Williams, MPA, Susan Szpunar, Ph.D. Presented by: Jack Green, M.B.A., B.S., Sr. Systems Analyst, Office of Public Policy Initiatives, Henry Ford Health System, 1 Ford Place Drive - OPPI 3C, Detroit, MI 48202; Tel: 313.874.3127; Fax: 313.874.3039; E-mail: JGreen1@hfhs.org Research Objective: To assess the effectiveness of an Automated Clinical Practice Guideline (ACPG) for Tobacco Use Cessation (TUC) designed for use within the electronic medical record. Outcome variables include TUC guideline adherence, tobacco use quit rates, and staff satisfaction with the TUC ACPG. Study Design: TUC guideline adherence was assessed with a pretest – posttest nonequivalent control group design. An intervention group received the TUC ACPG and a business process re-engineering (BPR) whereby patient vital signs and check-in notes are entered and viewed within the electronic medical record (CarePlus) instead of on paper. As the provider views this information, he or she is prompted, when appropriate, to follow the TUC guideline. The intervention group is referred to as the TUC sites. Two control groups served as comparison: one group received the BPR but not the TUC ACPG (Check-In sites), and the second group received no intervention (Control sites). Data on guideline adherence, tobacco use, and patient demographics were collected through telephone interviews of research subjects and through ACPG process point data. Provider reaction to the ACPG was determined through provider surveys and focus group sessions. Information was collected on the six month quit rates of post-implementation subjects who reported tobacco use. Data analyses include Chi-square tests of association and logistic regression. Population Studied: Patients aligned to study or control physicians at Henry Ford Health System in Detroit, Michigan were asked to consent to an interview. Of the 44,000 patients who consented, 8,867 patients at baseline and 7,809 patients post-implementation presented at the study clinics during the study months and were included for survey. 5,334 baseline patients and 3,970 post-implementation patients completed telephone interviews. 700 post-implementation tobacco users were resurveyed to assess 6-month quit rates. Principle Findings: Race, age, and education level for participants varied slightly among study groups. At baseline all study groups had high adherence rates; however, the TUC sites had higher guideline adherence rates than either of the controls. At the TUC sites, post-implementation adherence rates increased relative to baseline for all five points of the guideline with the largest increases seen in the ASSESS and ARRANGE guideline points (17% and 14% respectively). Logistic regression results indicated that the probability of a provider ASKing their patient’s tobacco use status was twice as high in the TUC sites relative to the no-intervention Control, controlling for time, related co-morbidities, and race. In addition, being at a TUC site significantly increased the probability of the ASSESS, ADVISE, and ARRANGE guideline points being followed over the control site, after accounting for time period, demographics and co-morbidities. Only the ASSIST rate was not significantly related to intervention group. Six-month quit rates showed no differences among the study groups; however, the TUC sites were more likely to report use of assistive therapies in their quit attempts. Provider understanding and acceptance of the Tobacco Use Cessation guideline varied among the study groups with the TUC sites demonstrating the highest acceptance of the requirements. Time constraints were the largest reported barrier to compliance with the guideline. Providers from TUC sites positively evaluated the ACPG implementation, with unanimous support for the automated means to refer patients for follow-up. Conclusions: The TUC ACPG was easily assimilated into the clinic process and promoted the provision of appropriate healthcare advice at the appropriate time. Implications for Policy, Delivery or Practice: Increased provider adherence with the established TUC guideline should translate into higher quit rates for current users and less recidivism for recent quitters. Tobacco-related morbidity and mortality remain major health concerns in the U.S. with large financial implications, thus further efforts at encouraging tobacco use cessation are imperative for the health of the U.S. and the U.S. economy. • Self-Medication of Mental Health Problems Katherine Harris, Ph.D., Mark Edlund, M.D., Ph.D. Presented by: Katherine Harris, Ph.D., Research Fellow, Office of Applied Studies, Substance Abuse and Mental Health Services, 5600 Fishers Lane, 16-105, Rockville, MD 20856; Tel: 301.443.0747; E-mail: kharris@samhsa.gov Research Objective: To evaluate the association between past 30 day use of alcohol, marijuana, and other illicit drugs and past year unmet need for and use of mental health care. Study Design: A subsample of 18,849 respondents from the 2001 National Household Survey on Drug Abuse and the 2002 National Survey on Drug Use and Health. Subjects were between the ages of 18 and 65 and had least one past year mental disorder symptom and no past year substance dependency. Logistic regressions of past 30-day substance use on past 12-month unmet need for mental health care and past 12-month use of mental health services controlling for clinical and socio-demographic characteristics. Predicted probabilities and corresponding standard errors are reported. Population Studied: Use of illicit drugs other than marijuana increased with unmet need for mental health care (4.4% vs. 3.2%, p=.046) but was not reduced with mental health care use. Heavy alcohol use was not associated with increased unmet need for mental health care, but was higher among individuals with no mental health care use (4.4% vs. 2.7%, p<.001). By contrast, marijuana use did not appear associated with either unmet need or mental health care use. Principal Findings: Substance use varies with past year unmet need for mental health care and mental health care use in ways consistent with the self-medication hypothesis. Results suggest that timely screening and treatment of mental health problems may prevent the development of substance use disorders among those with mental disorders. Use of illicit drugs other than marijuana increased with unmet need for mental health care (4.4% vs. 3.2%, p=.046) but was not reduced with mental health care use. Heavy alcohol use was not associated with increased unmet need for mental health care, but was higher among individuals with no mental health care use (4.4% vs. 2.7%, p<.001). By contrast, marijuana use did not appear associated with either unmet need or mental health care use. Conclusions: Substance use varies with past year unmet need for mental health care and mental health care use in ways consistent with the self-medication hypothesis. Implications for Policy, Delivery or Practice: Results suggest that timely screening and treatment of mental health problems may prevent the development of substance use disorders among those with mental disorders. Further research should identify subgroups of individuals for whom timely and appropriate mental health treatment would prevent the development of substance use disorders. • Healthcare Utilization, Expenditures, and Financial Burden of Families with Persons with Severe Mental Illness: Results from the 2000 Medical Expenditure Panel Survey Denys Lau, Ph.D., Thomas Taylor, Ph.D. Presented by: Denys Lau, Ph.D., Research Fellow, Outcomes Research, Pfizer / University of Michigan, 315 S. Division, #9, Ann Arbor, MI 48104; Tel: 734.622.4011; Fax: 734.622.2641; Email: Denys.Lau@Pfizer.com Research Objective: (1) Describe the socio-demographic and health characteristics, and the family situations of persons with severe mental illness (SMI-persons). (2) Examine the healthcare utilization, expenditure, and financial burden of families with a SMI-person (SMI-families). Study Design: Data were from the 2000 Medical Expenditure Panel Survey (MEPS), which contains self-reported data on the socio-demographic and health information, as well as healthcare utilization and expenditures of a nationally representative sample of the civilian, non-institutionalized U.S. population. SMI included schizophrenia (ICD-9-CM codes: 295.XX); affective psychoses (296.XX); paranoia disorder (297.XX); severe neurotic and personality disorders (300.4 and 301.11-301.13); and other functional psychoses (298.XX and 299.XX); all of which were grouped into three clinically meaningful categories by the Clinical Classification Software included in MEPS (CCS codes: 69-71). Financial burden for a family was the percentage of total family income for out-ofpocket health care expenditures. For non-normally distributed outcome variables, logarithmic transformation was performed before conducting bivariate analyses, z-test or t-test, depending on the un-weighted sample size. Only statistical significant results were reported (p-value<=0.05). Estimates were adjusted for the complex multistage survey design of MEPS. Population Studied: SMI-persons were estimated to be 1.0% of the civilian, non-institutionalized U.S. population, or about 2.9 million people. Among SMI-persons, 57.3% or 1.6 million people were living in a family (household with two or more persons). Among all U.S. families, 2.1% or 1.5 million families had a SMI-person, and 39.6% of the SMI-families had a SMIperson as the head of household. Principal Findings: Compared to the general population, more of the SMI-persons were between the ages of 18 to 64, earned less than $10,000, unemployed, on public health insurance, and reporting poorer self-perceived health, more functional and role limitations, and more comorbidities. Compared to other families, more of the SMI-families were either single adult with children or two adults with no children, had no private health insurance, and were poor or near poor. On average, SMI-families collectively had more office-based visits to healthcare providers (8.2 [SE=0.9] vs. 4.5 [SE=0.1]), higher overall healthcare expenditures ($2,821 [SE=$329] vs. $2,294 [SE=$81]), higher pharmaceutical expenditures ($701 [SE=$93] vs. $375 [SE=$13]), and greater financial burden (5.5% [SE=0.8%]) vs. 3.4% [SE=0.1%]), compared to other families. Poor or near poor SMI-families on average had four times greater financial burden as the high-income SMI-families (8.1% [SE=1.7%] vs. 2.2% [SE=0.3%]). Within SMI-families, the SMI-person on average had the lion share of the healthcare utilization and expenditures, with 12.7 [SE=1.7] office-based visits, $4,856 [SE=$668] overall healthcare expenditures, and $1,391 [SE=$217] pharmaceutical expenditures. Conclusions: Although SMI-families had greater healthcare utilization and expenditures, and higher financial burden than other families, the majority of the consumption was incurred by the SMI-person. Limited by the small un-weighted sample size, this study could not further investigate how the increased burden affected the healthcare utilization and expenditures for family members with no SMI. Implications for Policy, Delivery or Practice: Adequate resources may be required for SMI-families, especially the poor and near poor families, to meet the substantial healthcare needs of the SMI-person and the social welfare needs of their family members. Primary Funding Source: Pfizer, Inc. • Clinic Variation in Use of Antidepressant Medications for Primary Care Patients with Depression Chuan-Fen Liu, M.P.H., Ph.D., Edmund Chaney, Ph.D., Duncan Campbell, Ph.D., Yu-Fang Li, Ph.D., Mary McDonell, M.S., Stephen Fihn, M.D. Presented by: Chuan-Fen Liu, M.P.H., Ph.D., HSR&D Investigator, Health Services Research and Development, VA Puget Sound Health Care System, HSRD (152) 1660 S. Columbian Way, Seattle, WA 98108; Tel: 206.764.2587; Fax: 206.764.2935; E-mail: chuan-fen.liu@med.va.gov Research Objective: Depression is under-detected and undertreated in primary care. Yet, antidepressant pharmacotherapy has been shown to be effective in this setting. There is apparent variation in antidepressant prescription practices among settings. Studying the potential sources of this variation could help guide depression treatment improvement. This study examined variation in use of antidepressant medications among VA primary care clinics. Study Design: This was a retrospective, longitudinal study of veterans with a positive screen for major depressive symptoms at entry into the Ambulatory Care Quality Improvement Project (ACQUIP). Treatment utilization and pharmacy data were obtained from administrative databases for each local site. We examined variation in use of antidepressant medication during one year after the baseline across the 7 sites. Logistic regression was used to estimate the probability of any antidepressant use. Zero-inflated negative binomial regression models were used to estimate the number fills and the number of days of supply of antidepressant medications Population Studied: The study sample included 2,111 patients in the 7 primary care clinics participating in ACQUIP with Hopkins Symptom Check List (SCL) scores > =1.75 at baseline screening, suggestive of significant symptoms of major depression Principal Findings: Overall, 52% of patients with significant symptoms of major depression received at least one fill of antidepressant medication during the year (range 35- 58% across clinics). Across clinics, patients with depression averaged 4.5 fills of antidepressants with a mean supply of 160 days. The average number of fills and the number of days of supply per patient ranged from 2.8 to 5.7 and 101 to 168 days across clinics, respectively. After controlling for patient characteristics, case-mix, and baseline SCL score, depression history, prior use of antidepressant, and outpatient care utilization, treatment location (i.e., Primary Care Clinic) was significantly related to the likelihood of receiving at least one antidepressant fill, the number of fills, and to the number of days of supply. Conclusions: In this sample, only about half of primary care patients with significant symptoms of major depression were treated with antidepressant medications. After adjusting for patient characteristics, there was significant variation in antidepressant use among primary care clinics, likely reflecting different practice patterns among the clinics. Implications for Policy, Delivery or Practice: Further research is needed to improve practice patterns among primary care clinics in delivering evidence-based depression treatment. Primary Funding Source: VA • Financial Incentives and Gaming in Alcohol Treatment Mingshan Lu, Ph.D., Ching-to Albert Ma, Ph.D. Presented by: Mingshan Lu, Ph.D., Associate Professor, Department of Economics, University of Calgary, 2500 University Drive, N.W., Calgary, T2N1N4; Tel: 403.220.5488; Fax: 403-282-5262; E-mail: lu@ucalgary.ca Research Objective: Whereas a simple fee-for-service (FFS) allows much flexibility and minimal interference on the physician-patient relationship, managed care seeks to impose controls to achieve objectives deemed necessary by health plans or payers. Against the cost and quality controls in payment regimes other than FFS, clinicians may find ways to game the system. Our paper provides direct testing of the impacts of financial incentives on clinician gaming. Study Design: We present two data sets on client information in alcohol treatment episodes. Each of the two data sets originated from the same clinician. One set consisted of reports required by the Maine Addiction Treatment System for administrative and funding assessments; the other was abstract from actual medical records. Performance Based Contracting was a policy implemented by the state of Maine around the middle of the period for our data sets. MATS data were used by PBC to assess program performance, which then determined future funding. There are discrepancies in the two data sets. We hypothesize that the information inconsistencies are due to clinicians misreporting information to MATS to game the system. The implementation of PBC resulted in a financial incentive for clinicians to misreport information to MATS. Good performance recorded in MATS can be due to over-reporting of a client’s alcohol use at admission, or under-reporting at discharge. We identify over-reporting and under-reporting by comparing MATS data against medical record abstracts. We identify gaming incentives by the time dummy of the implementation of PBC. We are able to directly test gaming because of our unique data sets. The comparison between the MATS and medical abstract data is a straightforward way to identify gaming. The identification of financial incentives on gaming was due to the implementation of PBC. Our results call for attention on provider reactions against incentive mechanisms: information manipulation should not be ruled out when such actions have financial consequences. Population Studied: About 1,000 alcohol abuse treatment episodes in the state of Maine covering the period from October 1990 to June 1995. Principal Findings: We find strong empirical evidence for our hypotheses. PBC was found to have a significant and positive effect on clinicians over-reporting client alcohol use at admission and under-reporting at discharge. Because performance evaluation is from assessing alcohol use reduction and abstinence, these misreporting help boost treatment performance where clients actually have not improved. Conclusions: We find that the introduction of PBC has increased gaming. The pattern of gaming is consistent with clinicians exaggerating treatment performance to obtain higher financial rewards. Implications for Policy, Delivery or Practice: Our study suggests two policy implications. First, and perhaps more directly, auditing should be used more often when regulatory authorities must rely on information supplied by providers for financial and funding decisions. Appropriate auditing may deter gaming, and gives more reliability to the veracity of reports. Second, and perhaps less directly, establishing a gold standard should be considered whenever it is feasible. In our case, the analysis was possible precisely because we were able to compare the administrative reports against an appropriate standard, namely the medical record abstracts. Having an independent and reliable data source for testing the reliability of administrative data may seem obvious but appears to have received less emphasis. Data collection methods should consider obtaining the same information in more than one way. Primary Funding Source: NIAAA, Alberta Heritage Foundation for Medical Research • Clinical Supervision Issues in the Implementation of Randomized Clinical Trials Sarah Turcotte Manser, M.A., Joseph Guydish, Ph.D., Barbara Tajima, MEd, Martha Jessup, R.N., Ph.D. Presented by: Sarah Turcotte Manser, M.A., Senior Administrative Analyst, Institute of Health Policy Studies, University of California, San Francisco, 3333 California Street, Suite 265, Box 0936, San Francisco, CA 94143-0936; Tel: 415.476.3378; Fax: (415)476-0705; E-mail: sarahtu@itsa.ucsf.edu Research Objective: This qualitative study investigated the dissemination of evidence-based interventions in substance abuse treatment settings. We studied the extent to which evidence-based substance abuse treatments were adopted by programs participating in multi-site clinical trials. This study explored issues and challenges that emerged in the implementation of research initiatives within communitybased clinic sites and the factors that influenced adoption of the new treatment intervention. This study investigated: 1) the process and extent to which drug abuse treatment interventions are implemented and adopted by programs participating in multi-site Randomized Clinical Trials (RCTs), and 2) the barriers to intervention adoption and factors that increase or decrease the likelihood of adoption. This paper focuses on the issues and themes that emerged in the process and nature of the clinical supervision that occurred during the RCT. Study Design: We studied these issues within the research initiative of the Center for Substance Abuse Treatment’s (CSAT) Methamphetamine Treatment Project (MTP) which tested a manualized intervention for methamphetamine users at seven clinic sites. Forty-two individual, semi-structured interviews were completed at seven levels of clinical trial participation. Interviews were audio-taped and conducted inperson or, if necessary, by phone. Respondents were asked about their experiences with the clinical trial and issues related to project implementation and adoption of innovative interventions. Population Studied: Respondents consisted of 42 staff participants in the CSAT MTP clinical trial. These respondents were identified within seven organizational levels of the research initiative: study funders, steering committee members, study coordinating center staff, site principal investigators, site evaluators, clinic directors, and clinicians. Principal Findings: The supervisory model used in this RCT was a decentralized model where weekly conference calls with the study coordinating center and project clinical staff were used for monitoring of protocol adherence and case consultation. Critical challenges were identified in applying the distance supervision model within an existing supervisory model at the participating clinics. Issues and tensions arose between the project clinical component and the RCT clinical supervision component with the use of the distance supervision model. Conclusions: Themes related to the process and nature of the model used for clinical supervision in the RCT were: 1) supervisory relationships that were not well developed, 2) loss of autonomy, 3) lack of flexibility, 4) conflict with individual needs of clients and needs of client population, and 5) issues of intervention fidelity. Implications for Policy, Delivery or Practice: Identification and discussion of these themes will inform specific recommendations to the planners and implementers of RCTS and enhance the opportunities for the adoption of evidencebased interventions in substance abuse treatment. Primary Funding Source: NIDA • Contracting For Coordination of Behavioral Health Services in Privatized Child Welfare and Medicaid Managed Care D. Richard Mauery, M.P.H., Julie Collins, M.S.W., LCSW, Jan McCarthy, M.S.W., Charlotte McCullough, MEd, Sheila Pires, MPA Presented by: D. Richard Mauery, M.P.H., Senior Research Scientist, Department of Health Policy, GWU School of Public Health and Health Services, 2021 K Street, N.W., Suite 800, Washington, DC 20006; Tel: 202.530.2376; Fax: (202) 2960025; E-mail: rmauery@gwu.edu Research Objective: This study examined coordination between privatized child welfare initiatives and Medicaid managed care systems for the delivery of behavioral health care services for children and families in the child welfare system. Specific objectives: 1) to assess how states’ expectations as embodied in their contract documents are actually happening during program implementation; and 2) to identify promising approaches for delivery of coordinated behavioral health care services and contracting that can be shared with other stakeholders. The goal was to highlight the real world experiences and lessons learned that others may draw upon when designing and implementing similar contracts for systems of care. Study Design: Two linked qualitative research methods: 1) content analysis of Medicaid managed care and privatized child welfare contract documents that specify requirements for care coordination and interagency collaboration, and 2) site visits in four states to interview key stakeholders about how these paper requirements were playing out in practice. Population Studied: Staff of state child welfare, behavioral health, and Medicaid agencies; managed care organizations; family organizations; and foster and birth parents of children in child welfare systems in El Paso County, Colorado, Franklin County, Ohio, Massachusetts, and Missouri. Principal Findings: Despite varying degrees in scope and specificity of language regarding collaboration and care coordination, the child welfare contracts all encompassed service delivery expectations that acknowledge the importance of having access to an array of behavioral health services for children and their families (including supportive wraparound services) to maximize the likelihood of achieving successful permanent placements within shorter periods of time. All contracts covered standard behavioral health treatments. Specialized services, such as domestic violence treatment and sexual abuse/offender treatment, were far less likely to be covered in the contracts, particularly the Medicaid contracts. The success of interagency collaborations depends largely on key leadership having the authority, and taking the responsibility, for development and implementation of programs and systems that stress a coordinated approach to holistic care that integrates health, behavioral health, and permanency issues. Multiple categorical funding and reimbursement streams can create treatment silos that can hamper care coordination when children are perceived as belonging to one funding stream or another. Even well-written contracts cannot overcome shortages of providers with child and adolescent treatment expertise that result from low reimbursement rates and/or under-funding and under-staffing of public and private child welfare and behavioral health systems. Conclusions: Agencies and contractors are encountering difficulties fulfilling their contractual care coordination obligations, largely due to external factors such as the inadequate supply of specialized treatment providers and insufficient case rates and Medicaid reimbursements. Interagency collaborations serve to bring together decisionmakers who can apprise their colleagues of the intended and unintended effects of their actions on their programs. Implications for Policy, Delivery or Practice: Contract specifications, while critical, are only an essential first step to ensure effective care coordination for children with behavioral health needs and their families. Ongoing attention must be paid to implementation issues and to the factors that impede adherence to contract specifications and potentially threaten the achievement of positive outcomes for children and their families. Primary Funding Source: Center for Health Care Strategies, Inc. • Healthcare Cost Waste in the Treatment of Depression Stephen Melek, B.A. Math, FSA Presented by: Stephen Melek, B.A. Math, FSA, Consulting Actuary, Health, Milliman USA, 1099 18th Street, Suite 3100, Denver, CO 80202; Tel: 303.672.9093; Fax: (303) 299-9018; Email: steve.melek@milliman.com Research Objective: To identify and quantify potential healthcare cost savings associated with inappropriate and ineffective use of antidepressants, primarily among those prescribed by PCPs. Study Design: Individual prescription drug claim records were examined for services provided between 7/1/02 and 5/31/03 (based on claim service dates). Claimants that received prescriptions for any of 10 different popular anti-depressants during this period, regardless of diagnosis, were identified and chosen as the study group. We analyzed the treatment patterns for these antidepressant-taking patients by age and gender, by prescribing doctor, and by filling pharmacy in an attempt to identify areas of major concern for high levels of inappropriate or ineffective treatment – areas where behavioral healthcare quality is of major concern. Using data from the managed behavioral carve-out vendor, we separated patients that had also received treatment from a behavioral health specialist from those that did not, in order to identify differences in Rx treatment patterns for these two patient groups. We also analyzed other medical claims incurred by the antidepressant-taking patients during the experience period, including coded primary and secondary diagnoses, and types of services provided for these patients. This effort was to help quantify the potential amount of additional medical and diagnostic services provided to these same patients that may also be inappropriate or ineffective treatment costs. Population Studied: State of Louisiana employees and dependents. Principal Findings: The following potential annual savings were identified: $2.3 million in direct costs of antidepressant drugs, $10.2 million in direct costs of substituting generic for brand antidepressants, $0.3 million in direct costs of low dosage use. Nearly 15% of the State of LA adult population (ages 19+) filled an antidepressant prescription (annualized basis). That is comparable to recent AMA findings that 6.6% of adults in the U.S. suffer from major depression annually, and only about one-third of them receive medications. Approximately 67% of all patients that began treatment with antidepressants discontinued prior to the minimum six month duration stated in clinical guidelines; 25% of all patients that were prescribed an antidepressant never refilled their prescription. We also identified additional healthcare costs incurred by patients discontinuing antidepressant treatment too early that were associated with behavioral and psychosocial diagnoses in the claims data. Depending on the definition of behavioral and psychosocial disorders, for these patients: Between $9.9 million and $55.2 million of additional nonbehavioral healthcare costs are incurred annually; Between $2.3 million and $12.9 million of additional nonantidepressant prescription drug costs are incurred annually. Conclusions: Depressed patients too often get the wrong treatment by the wrong providers. Disruptive innovation to the current healthcare delivery system is needed to solve the multi-faceted problems with the way depression is treated today. Implications for Policy, Delivery or Practice: There is a substantial opportunity for quality improvement and increase in healthcare cost effectiveness through more effective identification, education and treatment of patients suffering from depressive disorders. There is also a substantial savings opportunity through more effective and appropriate use of antidepressants for the patients that truly may benefit from such treatment, and the elimination of inappropriate use of such drugs. Primary Funding Source: State of LA OGB • A Trial of Incentives to Improve Depression Therapy Appointment Adherence among Low-Income AfricanAmericans Edward Post, M.D., Ph.D., Jeff Harman, Ph.D., Mario Cruz, M.D. Presented by: Edward Post, M.D., Ph.D., Assistant Professor of Medicine and Psychiatry, Medicine and Psychiatry, University of Pittsburgh, 230 McKee Place, Suite 600, Pittsburgh, PA 15213; Tel: 412.692.4846; Fax: (412) 692-4838; E-mail: postep@msx.upmc.edu Research Objective: To evaluate the effect of nominal payments to offset incidental expenses (e.g., transportation) of attending regularly scheduled therapy appointments for low-income African-American patients with depressive disorders. Study Design: The study uses an interrupted time-series design: appointment adherence is tracked without monetary incentive during an initial twelve-week period, followed by a second twelve-week period of $10 payments at regularly scheduled therapy appointments (usually weekly, but at the discretion of the therapist), and a third twelve-week period of appointment adherence assessment without monetary payments. Baseline and exit surveys are conducted to collect demographics, information on attitudes and barriers to care, and to assess depression severity with the PHQ-9. Fifty subjects have been enrolled and are being monitored during a 36-week period of follow-up that begins at the time of study enrollment for each individual. Population Studied: Patients with coded billing diagnoses (either prevalent or incident) of major depression or depression NOS, who seek care at a community mental health center that serves a predominantly African-American neighborhood in Pittsburgh, Pennsylvania. Principal Findings: The subjects’ mean age is 47 years (standard deviation=9; range=28 to 69); 94% are AfricanAmerican; 86% are female; and 88% are currently prescribed psychoactive medication. The mean PHQ-9 score obtained during the baseline survey was 13.8, indicating on average a significant level of ongoing depression symptomatology. 72% of subjects travel to appointments via bus; the median oneway fare was $1.50. 78% report that their therapy sessions make them feel better, and 52% report that they would attend a therapy session to receive $10 even if the session was not helpful to them. Among follow-up accrued to date, data indicate that in the aggregate, subjects kept 66.8% of appointments in the baseline twelve-week period. Monetary payments during the second twelve-week period are associated with a halving of the nonattendance rate, as aggregate appointment adherence rose to 83.6%. Analysis of individual trends shows that relative to the first follow-up period, 65.4% of persons improved their attendance rate; 15.4% remained the same; and 19.2% had lower attendance rates in the second period. Among all of these subjects, the median absolute increase in appointment adherence is 21.4%. This improvement in individual appointment adherence is statistically significant (p< 0.0004 using a paired t-test). Additional data will be presented on adherence in the third period of follow-up. Conclusions: Nominal incentive payments can improve appointment adherence for therapy sessions among depressed, low-income African-American patients. The subjects are evenly split over whether they would attend a therapy session based on the incentive in the absence of a personal belief in its utility. Data on appointment adherence following the incentive period are currently being accrued. Implications for Policy, Delivery or Practice: Facilitating adherence to proven treatments for depressive disorders is central to improving outcomes for low-income AfricanAmericans with depression. Additional studies are needed to replicate, evaluate and implement both patient-level and provider-level incentives to improve quality of care. Primary Funding Source: Staunton Farm Foundation • Building Organizational Capacity in Substance Abuse Treatment Agencies Andrea Burling, Ph.D., Karen Shore, Ph.D., Mary Anne Lahey, Ph.D., Christine Timko, Ph.D., Thomas Burling, Ph.D., Edward Carlson, M.A., MFT Presented by: Karen Shore, Ph.D., Senior Research Scientist, , American Institutes for Research, 1791 Arastradero Road, Palo Alto, CA 94304; Tel: 650.843.8121; Fax: 650.858.0458; E-mail: kshore@air.org Research Objective: To build organizational capacity of substance abuse (SA) treatment agencies, through comprehensive organizational assessments and identification of specific capacity building projects. Study Design: The Building Effective Substance Abuse Treatment (BEST) Initiative is a series of projects funded by the Charles and Helen Schwab Foundation. To date, there have been two phases to the initiative. The first involved 12 SA agencies in San Mateo County, CA and the second involved 6 agencies in other San Francisco Bay Area counties. The Foundation’s program officer identified agencies for potential inclusion. Each BEST agency participated in an assessment and planning (AP) process led by a multidisciplinary consulting team. The AP process for each agency involved a comprehensive, multimethod organizational assessment that included 1) an initial planning meeting with the agency executive director; 2) document collection and review; 3) a site visit involving multiple individual and group interviews; and 4) a provider selfassessment. Each agency was assessed in eight organizational system areas: purpose and goal attainment, clinical care and quality improvement, governance and leadership, staff development and human resources, structure and communication, business operations, infrastructure, and community context and connectedness. Each agency received an AP report summarizing their organizational strengths, problems or challenges, areas for improvement, and recommendations for appropriate organizational capacity building projects. Subsequent to the AP process, each agency submitted a proposal to the Foundation for funding of a specific capacity building project. Population Studied: 18 non-profit SA treatment agencies were studied. 20 were invited to participate in the first two phases of BEST and 1 declined in each phase. Principal Findings: The AP process revealed a variety of strengths in the participating SA agencies, as well as a variety of needs. Some of the most common agency strengths included a shared sense of mission within each agency; passionate, committed staff; and solid relationships with their communities. Some of the most common problems concerned purpose and goal attainment and governance and leadership systems (e.g., little or no strategic planning, inactive/ineffective Boards of Directors, overly centralized decision making); data/quality management systems (e.g., multiple data systems that could not communicate with one another, poor or non-existent systems for tracking client process and outcome measures of quality); human resource systems (e.g., low staffing levels, low salaries, difficulties in recruiting and retaining staff ); and clinical care systems (e.g., insufficient agency and/or community resources to address client needs such as mental health). Conclusions: Funding to address organizational and infrastructure needs are rarely available to non-profit SA treatment agencies. While they have passionate, dedicated, and hardworking staff providing services to many who are in great need, these agencies face significant challenges and problems in multiple organizational system areas. Implications for Policy, Delivery or Practice: Non-profit SA treatment agencies can enhance their organizational functioning and capacity by engaging in organizational assessments via self-assessments and/or with the assistance of consultants. Increased funding should be made available to assist these agencies with these assessments, as well as the design and implementation of capacity building projects. Primary Funding Source: Charles and Helen Schwab Foundation • Do Pleasing Pictures Have a Healing Effect on Seriously Ill Patients? Kazue Takayanagi, M.D., Ph.D., Tatsuo Kumazaki, Director of Hospital Presented by: Kazue Takayanagi, M.D., Ph.D., Associate Professor, Health Services Administration, Nippon Medical School, 1-1-5, Bunkyo-ku, Sendagi, Tokyo, 113-8602; Tel: 81.3.3822.2131; Fax: 81-3-3822-8144; E-mail: taka-y@nms.ac.jp Research Objective: We investigated the healing potential of viewing pleasing pictures in patients with terminal illness. Study Design: A focus group, consisting of one art curator, two hospital decorators, two nurses, and one doctor, chose 120 pictures out of 9000 in the art catalogues of the hospital. Six factors - brightness of color, sharpness of line, content, abstractness, landscape quality and action - were analyzed for each picture. On this basis, 30 pictures were selected: 10 as pleasing, 10 as neutral and 10 as not pleasing. Patients themselves assessed the 30 pictures as pleasing, neutral and not pleasing. They then chose one pleasing picture to observe for 15 minutes. A Profile of Mood test (POMS) was administered2), and pulse, blood pressure, chromogranin A in the saliva, and NK cell activity in the blood were measured, both before and after observation of the selected picture. Population Studied: Thirty-five private patients with terminal illness (average age 60.9 years ± 13.5), in the university hospital of Nippon Medical School, participated in the study. Informed consent was obtained from all the participants. Principal Findings: The pictures characteristically chosen by the patients as pleasing were representational landscape or nature paintings with bright colors, gentle lines and a positive content. Abstract or action pictures with dark colors, harsh lines and a negative content were not selected. The patients particularly favored landscape pictures with a water motif. When analyzed using the t-test, Profile of Mode Score (POMS) showed significant decreases in tension -anxiety, depression (p<0.01), anger (p<0.001), fatigue (p<0.005), and confusion (p<0.05), and borderline significance for increased vigor (p=0.052). Pulse and blood pressure fell significantly (p<0.05), as did concentration of salivary chromogranin A (p< 0.05). Twenty-five patients permitted blood samples to be taken. These revealed no significant difference in NK activity before and after observing the picture, due to extreme variability of response (before 100%; after 113.2±77.3%, range 21.3 to 420.0%). An increase in NK cell activity occurred after looking at the picture in 10 patients who had chosen a picture with a natural and gentle landscape, while serum NK cell activity decreased in 14 patients who had chosen a picture which had emotional message. Examples are Botticelli’s “Birth of Venus ” and F.E.Church’s “Sunset”. NK activity is not always increased by the most pleasing picture, although POMS and Chromogranin A improved. Conclusions: Pictures of landscapes with bright colors and gentle lines were most often selected as pleasing by patients in this study. Looking at pleasing pictures altered psychological state, and may reduce sympathetic tone, in patients with terminal illnesses. Observation of the picture did not necessarily enhance immunity, especially if impressive pictures were chosen . Pictures for the rooms of seriously ill patients should be chosen to enhance their physiological and psychological well-being. Implications for Policy, Delivery or Practice: Pictures for the rooms of seriously ill patients should be chosen as a landscape or nature paintings with bright colors, gentle lines and a positive content, but not with emotional message. Primary Funding Source: University • Adopting New Approaches to Addiction Treatment: What Matters to Clients and Counselors? Cindy Thomas, Ph.D., Dennis McCarty, Ph.D., Marilyn Daley, Ph.D., Traci Reickmann, Ph.D., Brett Fuller, Ph.D. Presented by: Cindy Thomas, Ph.D., Senior Scientist, Schneider Institute for Health Policy, Brandeis University, 415 South Street, MS 035, Waltham, MA 02454; Tel: 781.736.3921; Fax: 781-736-3905; E-mail: cthomas@brandeis.edu Research Objective: The federal government has devoted considerable resources to developing new medications to treat addictions. Little information is available, however, on how members of treatment communities view new pharmacological approaches, and intend to adopt them as part of treatment plans. Our objective is to examine attitudes and beliefs of clients in treatment and providers toward new treatment medications, and identify factors associated with their intention to incorporate them into treatment, in order to enhance efforts to promote adoption. Study Design: A survey was administered to small groups of counselors and clients in addictions treatment (programs selected based on size, willingness to participate, and location), to determine predictors of intention to recommend and/or use four current or potential pharmacological approaches to treatment: methadone, buprenorphine, clonodine, and ibogaine, an alternative substance that is classified as a nutritional supplement. Data were analyzed using descriptive statistics to identify differences between modalities and clients versus counselors, and multivariate regression analyses to develop models to predict the intention to use each of the above pharmacotherapies in the future. Population Studied: We surveyed 377 addictions treatment counselors, and 1083 clients in treatment for opiate addiction in Massachusetts and Oregon. Treatment modalities represented were: methadone programs, other outpatient programs, and residential programs. Principal Findings: Preliminary analysis indicates that counselors were more receptive than were clients toward three of the four medications, while clients were more receptive to use of an alternative nutritional supplement. Half of clients at this time said they were unlikely to take buprenorphine; a third of counselors said they were unlikely to recommend it currently. Attitudes toward various medications in addiction treatment vary considerably by the type of treatment setting: outpatient programs appeared more receptive than methadone clinics or residential programs to adopting new pharmacological treatments such as buprenorphine. After controlling for treatment setting, attitudes and subjective norms had more influence on clients’ and counselors’ intent to use these new medications, than did demographic characteristics, or beliefs about the particular medication’s attributes. Peer support is crucial for both counselors and clients when designing a treatment plan: when clients make a decision about taking a new pharmaceutical, the counselors are the individuals whose advice they trust most, followed by friends and family members. Counselors are most influenced by patients’ individual needs and the influence of coworkers, rather than by clinical supervisors. Conclusions: Providers and clients are interested in new and emerging treatments that will improve effectiveness of treatment. However, they are strongly influenced by peers and social norms in their intentions to adopt these therapies. In encouraging counselors to consider incorporating new medications into treatment, an approach that includes the input of peers who have had successful experience with such medications will be important, rather than a top-down-only approach. Additionally, educational programs and interventions have to be tailored to specific modalities of therapy, and supported by provider organizations. Implications for Policy, Delivery or Practice: The results of this study are of considerable value when designing interventions to promote use of new pharmacological and other treatments in addiction. In the past, some medications such as naltrexone were not widely adopted by providers and clients, in part due to features of the medication itself, but in part due to the (often “top-down”) approaches taken to encourage adoption. This study is particularly important considering the recent FDA approval of buprenorphine in office practice, and current federal efforts to promote its use. We identify those influences that are greatest in leading to the intention to use buprenorphine, both from the provider and the patient perspective. Primary Funding Source: NIDA • Social Support in the Pain-Depression Relationship Shana Traina, M.A., Grace Park, M.P.H., Harold E. Paulus, M.D., Weng Kee Wong, Ph.D., Catherine MacLean, M.D., Ph.D. Presented by: Shana Traina, M.A., Health Services Researcher, Medicine/Rheumatology, UCLA, 1000 Veteran Avenue Room 32-59, Los Angeles, CA 90095; Tel: 310.825.9071; Fax: 310.206.1227; E-mail: straina@mednet.ucla.edu Research Objective: To describe the relationship of pain, depression, and social support in patients with rheumatoid arthritis, or RA. Study Design: Ongoing observational cohort study of patients with early RA. At baseline and approximately every six months, patients complete mail surveys that include a depressed mood index, the Center for Epidemiologic Studies Depression Scale or CES-D; a physical function scale, the Health Assessment Questionnaire or HAQ; a pain component using a visual analog scale or VAS; and a social support index, the Lubben Social Network Scale. Demographics such as age, gender, ethnicity, and level of education were also collected. Baseline data were analyzed to describe the relationship of pain, depression, and social support in early RA patients. Data from 322 study patients were analyzed using Student’s t-tests, chi-square tests, and linear regression models. After baseline data were subset above and below the median on age, disease activity score, disease duration, income, and HAQ, t-tests were used to compare the means of Lubben, CES-D, and pain. Population Studied: Subjects were recruited through a network of community-based rheumatologists in the Western United States. Eligibility criteria for enrollment were fulfillment of the 1987 revised ACR criteria for RA, symptom onset within one year and no prior therapy with disease-modifying antirheumatic drugs, or DMARDs. Subjects have been recruited on a rolling basis since 1993 and prospectively followed for an average of 3.5 years with a range of 2 to 10 years. The average subject age is 50.3 years, 77 percent are female, and 76 percent are Caucasian, with an average education level of 13 years. Principal Findings: Depression scores were worse among patients under age 50 than among older patients, 17.3 vs. 13.5 CES-D units, p = 0.01, respectively. Pain scores were worse among patients with disease duration less than six months than among patients with a longer disease duration, 55.0 vs. 63.7 mm, p = 0.02, respectively. Depression scores were better, 11.0 vs. 19.8, and pain scores were better, 44.8 vs. 71.2 mm, among patients with better physical function scores, that is HAQ below 1.25. Social support and depressed mood were inversely correlated. Higher depression scores are associated with more pain, worse physical function, and lower social support. Conclusions: Social support may mediate the paindepression relationship in early RA patients. Those who exhibited more depressed mood were also likely to have less social support and have more pain. Younger patients were more depressed than older patients, and people with better function were less depressed and reported less pain than people with worse function. Implications for Policy, Delivery or Practice: Providing social support to RA patients may help to improve their pain, function, and depression. • Community-Based Participatory Research: A Systematic Review of Research Quality, Community Involvement and Intended Outcomes Meera Viswanathan, Ph.D., Alice Ammerman, Dr.P.H., Eugenia Eng, Dr.P.H., Gerald Gartlehner, M.D., Kathy Lohr, Ph.D. Presented by: Meera Viswanathan, Ph.D., Research Analyst, Health, Social and Economics Research, RTI International, 3040 Cornwallis Road, RTP, NC 27513; Tel: 919.316.3930; Fax: 919.541.7384; E-mail: viswanathan@rti.org Research Objective: AHRQ commissioned the RTI-UNC Evidence-Based Practice Center to conduct a systematic evidence review on community-based participatory research (CBPR) approaches to improved health. This paper focuses on two questions covered by the systematic review: 1) How has CBPR been implemented to date with regard to the quality of research methodology and community involvement? 2) What is the evidence that CBPR efforts have resulted in the intended outcomes? Study Design: We employed well-established methods of evidence review. We generated a list of search terms for our systematic search strategy. We then searched standard electronic databases for all years: MEDLINE®, Cochrane Collaboration resources, Psycinfo, and Sociofile. We conducted hand-searches of the reference lists of relevant articles and sought additional citations from a panel of experts. We abstracted information from individual or groups of articles pertaining to each study into standardized forms, and transferred the information onto evidence tables. We also created quality rating forms to assess each study’s research methods and adherence to CBPR principles of community collaboration. Population Studied: We included peer-reviewed reports on CBPR studies that: were published in English language; conducted in the United States and Canada; and included at least one community collaborator. We included in our review a total of 123 articles that make up 60 studies. Principal Findings: We classify studies according to whether or not they intended to implement and evaluate interventions, and by study design. We summarize research design, methods and community involvement in research for all 60 studies. Further, for the smaller subset of studies that had completed and fully evaluated interventions, we assess the quality of research and community participation and the nature of health outcomes. Conclusions: We classified studies according to whether or not they intended to implement and evaluate interventions, and by study design. We summarized research design, methods and community involvement in research for all 60 studies. Further, for the smaller subset of studies that had completed and fully evaluated interventions, we assessed the quality of research and community participation and the nature of health outcomes. Implications for Policy, Delivery or Practice: CBPR is a collaborative approach to research that combines methods of inquiry with community capacity-building strategies to bridge the gap between knowledge produced through research and what is practiced in communities to improve health. Although many researchers and practitioners offer definitions and principles for this approach, no clear consensus has emerged to move the field forward. Moreover, during a time when interest is growing rapidly for academic institutions, health agencies, and communities to form research partnerships, few guidelines exist as to how CBPR proposals should be evaluated and what resources are required to promote successful collaborative research efforts. This paper will help to establish the nature of the current literature. It will also assist academics, community participants and funders by identifying gaps in implementing this approach. Primary Funding Source: AHRQ, National Cancer Institute • Continuity of Anti-Psychotic Therapy under Capitation Financing in Colorado Neal Wallace, Ph.D., Joan Bloom, Ph.D., Teh-Wei Hu, Ph.D., Anne Libbey, Ph.D. Presented by: Neal Wallace, Ph.D., Assistant Professor, Public Administration, Portland State University, P.O. Box 751, Portland, OR 97207-0751; Tel: 503.725.8248; Fax: 503-725-8250; E-mail: nwallace@pdx.edu Research Objective: This study investigates the impact of Colorado’s Medicaid mental health capitation payment program on the continuity of anti-psychotic prescriptions among persons diagnosed with Schizophrenia. Loss of medication continuity has been found in studies of other public mental health capitation programs such as Tenncare (Ray et al, 2003) but creates somewhat of a quandary. Medication therapy, typically paid for outside of the capitation program, is protective of costly psychosocial interventions, and thus its continued, if not increased, use would be consistent with the financial incentives of these programs. In 1995, Colorado implemented a capitation payment program covering psychosocial treatments in part of the state while leaving some areas under existing Fee-For-Service (FFS) reimbursement. Prior studies by Bloom et al (1998,2001) and Cuffel et al (2001) found significant reductions psychosocial treatments after capitation without decrements in a wide range of measured clinical and social outcomes. Study Design: This study uses a difference in difference approach to evaluate the impact of capitation on antipsychotic prescription patterns compared to FFS. Antipsychotic continuity is measured as the probability of any use and the number of months with filled prescriptions in a period. Probability of any psychosocial treatment and cost of treatment given use are also measured along with change scores for the Schizophrenia Subscale of the Brief Psychiatric Rating Scale (BPRS). Explanatory variables include indicators for two capitation organizational models, one pre- and two post-capitation periods, and their interactions along with age, gender, ethnicity and prior treatment cost profile as subject controls. Population Studied: The study sample consists of 235 of Bloom’s original study subjects with a diagnosis of Schizophrenia but not enrolled in a medical HMO. Pharmacy claims were not consistently available for these subjects. Subjects are nearly equally distributed across the three models, similar in age and gender, but with some differences in ethnicity and prior treatment costs. During the precapitation period, over 95% of the subjects received some psychosocial treatment. Principal Findings: Probabilities of anti-psychotic use increased in both post-capitation periods for both organizational models relative to FFS. These effects were moderate to large but only one was statistically significant. Duration or intensity of anti-psychotic use, measured in months with filled prescriptions appeared unchanged. Effects were small and of mixed sign. In comparison and consistent with prior findings, subjects in both capitated areas had significantly decreased probabilities of psychosocial treatment use with deceases in treatment cost only in the MBHO areas. Difference scores for the Schizophrenia Subscale showed consistent, moderate positive effects but these did not reach statistical significance. Conclusions: Within the Colorado capitation program, continuity of anti-psychotic therapy was not impaired, despite significant decreases in the continuity and intensity of psychosocial treatments. Positive symptoms generally amenable to anti-psychotic therapy where also preserved. Capitation financing does not inherently risk loss of medication continuity by consumers. Implications for Policy, Delivery or Practice: Medication use appears to be a better process indicator of program success than psychosocial treatment patterns and is more consistent with outcomes. Psychosocial treatment can be selectively reduced without interfering with medication therapy. Further research on the conditions that allow this is warranted. Primary Funding Source: NIMH • Are Anxiety Disorders Underdiagnosed and Undertreated in Routine Psychiatric Practice? Joshua Wilk, Ph.D., Joyce West, Ph.D., M.P.P., William Narrow, M.D., M.P.H., Donald Rae, M.A., Lisa Countis, Darrel Regier, M.D., M.P.H. Presented by: Joshua Wilk, Ph.D., Research Scientist, Practice Research Network, American Psychiatric Institute for Research and Education, 1000 Wilson Boulevard, Suite 1825, Arlington, VA 22209; Tel: 703.907.8618; Fax: 703-907-1087; E-mail: jwilk@psych.org Research Objective: 1) To assess rates of detection and diagnosis of anxiety disorders in routine psychiatric practice; 2) To examine patterns of treatment of patients with anxiety symptoms or diagnoses. Study Design: 615 psychiatrists from a full range of clinical settings participated in the American Psychiatric Practice Research Network’s 1999 Study of Psychiatric Patients and Treatments (SPPT) generating nationally representative clinical data on 1,843 patients. Comparisons were also made with household respondents in the National Comorbidity Survey (NCS) who reported using specialty mental health services. Population Studied: 615 psychiatrists from a full range of clinical settings and household respondents in the National Comorbidity Survey (NCS) who reported using specialty mental health services Principal Findings: The prevalence of anxiety disorders reported by psychiatrists in routine practice was much lower than the prevalence found in self-reported specialty mental health service users ascertained through a structured household interview. Phobias were 22 times more likely to be diagnosed in the NCS sample compared to the SPPT sample. PTSD was diagnosed at 5 times the rate in the NCS sample compared to the SPPT sample, GAD at over 3 times the rate, and panic disorder at more than twice the rate. When SPPT patients with a DSM-IV anxiety disorder were combined with patients who had no reported anxiety disorder but with moderate or severe anxiety symptoms, the percentage in the SPPT sample increased from 23.8% to 54.7%, closer to the level of anxiety diagnoses in the NCS sample (68.1%). Over 10% of SPPT patients with panic disorder were receiving neither psychotherapy nor anti-anxiety medication (anti-anxiety medications were categorized broadly to include SSRIs and venlafaxine as well as conventional anxiolytics such as the benzodiazepines), while 8% of patients with PTSD were receiving neither anti-anxiety medication nor psychotherapy. 14% of patients with no anxiety diagnosis, but moderate to severe anxiety symptoms were not receiving psychotherapy or anti-anxiety medication. While over 75% of patients with generalized anxiety disorder or panic disorder were receiving anti-anxiety medications, less than two-thirds of patients with a phobia diagnosis and slightly over two-thirds of patients with PTSD were receiving these medications. The most commonly prescribed anti-anxiety medications included Alprazolam (16.7% of patients with anxiety disorders), Clonazepam (16.4%), and Paroxetine (15.9%). Conclusions: These findings suggest that anxiety disorders are underdiagnosed and sometimes undertreated in routine psychiatric practice. Further research is needed to examine associated factors or clinical rationale for the findings such as clinical significance, comorbidity, and prevailing standards of diagnostic assessment. Longitudinal research that includes an in depth assessment of treatment patterns, sequencing, and outcomes is needed to assess the extent to which not diagnosing and treating anxiety disorders and symptoms results in poorer outcomes. Implications for Policy, Delivery or Practice: Not diagnosing and treating anxiety disorders and symptoms could result in poorer outcomes and suggests the need for interventions, including increased screenings for anxiety disorders. Primary Funding Source: CSAT, American Psychiatric Foundation, the John D. and Catherine T. MacArthur Foundation, the Center for Mental Health Services • Can Pharmacy Data Identify Severely Mentally Ill Patients Needing Help with Adherence? Marcia Valenstein, M.D., M.S., Emily Woltmann, M.S.W., Janet Kavanagh, M.S., John Zeber, M.H.A., Patricia Schraner, M.S.W. Presented by: Emily Woltmann, M.S.W., Health Science Research Specialist, Severe Mental Illness Training Research and Evaluation Center (SMITREC), Ann Arbor Veterans Affairs Healthcare System, 2215 Fuller Court, Ann Arbor, MI 48105; Tel: 734.769.7100 Ext. 6259; E-mail: ewoltman@umich.edu Research Objective: Patients with schizophrenia and poor antipsychotic adherence are at increased risk for relapse and re-hospitalization. In organized healthcare systems, pharmacy data might be profitably used to identify patients who would benefit from adherence interventions. However, it is not clear if pharmacy data will be an accurate and efficient method for identifying at-risk patients. We examined whether patients who were flagged as poorly adherent by pharmacy data also appeared to be poorly adherent upon chart review. Study Design: Pharmacy data from two VAs were used to identify patients with schizophrenia/schizoaffective disorder who filled < 80% of the oral antipsychotics needed for continuous 12-month coverage (N=537). We reviewed medical charts to determine potential explanations for patients’ failure to fill antipsychotics, such as transferring care, starting longterm depots, patient death, or clinician discontinuation of medications. Population Studied: Patients were included in the study if they had a current diagnosis of schizophrenia or schizoaffective disorder and had at least two outpatient mental health visits in the previous 12 months the VA facilities. Principal Findings: Chart data indicated that approximately 33.5 % of all veterans flagged as poorly adherent (n=185), may have been “false positives”. These patients’ notes indicated they had formally transferred their psychiatric care, moved or lived out of state, had had their medications discontinued for clinical reasons, had been receiving depot antipsychotics for most of the year or were deceased. Of the 66.5% patients who were “true positives” for poor adherence, only16% were already receiving interventions to improve their adherence, such as supervised housing placement, community outreach, treatment with depot medications in response to recent poor adherence, or prescription of clozapine. Conclusions: Chart data indicated that approximately 33% of patients with an administrative diagnosis of schizophrenia who are flagged as poorly adherent by pharmacy data may have been adherent. The remaining 67% appear to be true positives. Few true positive patients were receiving strong interventions to improve adherence. Implications for Policy, Delivery or Practice: Pharmacy data may be a useful first screen for poor adherence but must be followed by chart review before outreach efforts are made. Primary Funding Source: VA, • Atypical Antipsychotics and Schizophrenia with Comorbid Substance Abuse John Zeber, M.H.A., Laurel Copeland, Ph.D., Frederic Blow, Ph.D., David Smelson, Psy.D. Presented by: John Zeber, M.H.A., Research Associate, HSR&D, Department of Veterans Affairs, 928 Rose Drive, Ann Arbor, MI 48103; Tel: 734.769.7100 Ext. 6260; Fax: (734) 7612617; E-mail: jzeber@umich.edu Research Objective: The advent of second generation, or atypical, antipsychotic medications has offered a wider and potentially more beneficial variety of treatment options for patients with schizophrenia. Recently these newer drugs have also been expanded for use in other psychiatric populations, with early promising results. Veterans with schizophrenia and a comorbid drug dependency are more expensive and challenging to treat than patients with only one psychiatric condition. These individuals tend to be less stable, especially in terms of medication compliance and inpatient utilization, compared to similar patients without a substance abuse diagnoses. However, atypical antipsychotics (AP) may help stabilize dopamine levels, diminish cravings, and be more efficacious than conventional drugs. We explore the effect of atypical APs among patients with dual diagnosis. Study Design: The VA’s National Psychosis Registry provided data on psychiatric and substance abuse diagnosis (schizophrenia, plus either cocaine or alcohol dependence) and the prescription of APs in FY99. Initial analyses examined the number of medications prescribed and compliance rates among 56,816 patients with and without a substance abuse diagnosis. Then, among just the veterans with a dual diagnosis (N=8,199), we examined differential effects of atypical or conventional APs on service utilization, compliance, and relapse (re-admission within 90 days). Population Studied: A national population of all veterans with schizophrenia alone, and individuals who also received a diagnosis for comorbid substance abuse. Principal Findings: Of the entire population of veterans with schizophrenia, 14 percent of patients were also diagnosed with comorbid substance abuse dependence. Compared to patients with schizophrenia alone, the dually diagnosed veterans were prescribed more APs (patients on two or more drugs: 37 percent vs. 25 percent), were nearly twice as medication non-compliant, and used significantly more healthcare services. They also more commonly received atypical APs (70 percent vs. 55 precent). Within just the more limited sample on dually diagnosed patients, the use of atypical antipsychotics was not associated with decreased inpatient use, nor did these patients experience better shortterm relapse rates. However, medication noncompliance rates were significantly lower (multivariate OR=.82, CI95 .74-.92). Conclusions: Compared with conventional APs, atypical antipsychotic agents appear to improve compliance for these difficult to treat and high-utilization patients, an important outcome given the generally poor adherence rates among this vulnerable population. Implications for Policy, Delivery or Practice: Atypical APs may prove to be particularly effective in the treatment of dual diagnosis patients to improve compliance, relieve substance abuse cravings, and potentially reduce psychiatric stays and relapses over a longer period. Further research should examine atypical APs and symptomology, focusing on the burden of illness from both schizophrenia and addiction. Primary Funding Source: VA • Efforts to Recruit Patients with Serious Mental Illness into a Randomized Research Study John Zeber, M.H.A., Marcia Valenstein, M.D., M.S., Emily Woltmann, M.S.W., Janet Kavanagh, M.S., Patricia Schraner, M.S.W. Presented by: John Zeber, M.H.A., Research Associate, HSR&D, Department of Veterans Affairs, 928 Rose Drive, Ann Arbor, MI 48103; Tel: 734.769.7100; Fax: (734) 761-2217; Email: jzeber@umich.edu Research Objective: Despite an NIH mandate for increased participation of minorities and women in health stuides, these groups are often under-represented. This scenario may result from problems in recruitment and enrollment. These difficulties are particularly salient when research involves patients with serious mental illness (SMI), representing a challenge in the ability to contact these individuals and subsequent recruitment success. Patient characteristics that can influence recruitment efforts include gender, age, comorbid substance abuse, illness severity and social support. Differential recruitment and drop-out rates can introduce significant research bias, less reliability, and low generalibility regarding observed results. Within the VA, a veteran’s “period of military service” and level of service connectedness is an important predictor for successful recruitment. The objective of this study is to examine reasons for differential contact and recruitment success during a randomized trial to improve medication compliance. Recruitment efforts included telephoning patients or next of kin, and meeting patients at their clinic appointments. Study Design: Research staff attempted to recruit all patients identified as having a serious mental illness and poor antipsychotic adherence at three VA medical centers (two urban, one suburban site). Patients were initially contacted by letter, followed by a telephone call or being approached during their next clinical appointment. We used bivariate and multivariate logistic regression to analyze differences in staff’s “ability to contact” patients and refusal rates by location, diagnosis, patient demographics, medication compliance, and level of VA service-connection. Population Studied: Veterans with serious mental illness (schizophrenia or bipolar disorder) and poor antipsychotic adherence, meeting eligibility criteria for a multi-site RCT to improve medication compliance (N=241). Principal Findings: Study personnel were able to contact 76 percent of the identified patients. In multivariate analyses, researchers were significantly more likely to successfully contact married patients (OR: 2.55), those living in the suburban site (OR=1.71), and patients with a service-related disability (OR: 1.80). However, there were no differences in contact rates by race, diagnosis, or substance abuse comorbidity. Of the 183 patients contacted, 71 (39 percent) agreed to participate in the study. Patients with a bipolar rather than a schizophrenia diagnosis, lived in a suburban location, had lower medication adherence rates, and who had a service-related condition were more likely to agree (ORs: 3.07, 3.97, 2.17, and 2.32, respectively). There were no differences by race, marital status, substance abuse, or gender in the likelihood of participation. Conclusions: In this study, minority patients appeared as likely to participate as non-minority patients, with adjustment for urban location, service connection, and type of psychiatric diagnosis. However, other patient characteristics did influence the ability to contact these individuals and their likelihood of agreeing to participate in the research study. Implications for Policy, Delivery or Practice: Challenges may arise during contact attempts and subsequent recruitment efforts, with differences by patient characteristics. Once contacted, under-represented groups appear just as willing to participate in a health services study. However, recruitment in urban areas may require special outreach efforts to locate patients. Vulnerable SMI veterans may offer unique difficulties during the course of randomized projects. Researchers should devote attention to patient differences in ensuring appropriate representation and accurate interpretation of results. Primary Funding Source: VA Invited Papers Prescription Drugs & Behavioral Health Chair: Haiden Huskamp, Ph.D. Sunday, June 6 • 5:00 p.m.-6:30 p.m. • Panelists: Thomas Croghan, RAND; Patricia Deverka, Medco Health Solutions, Inc.; Benjamin Druss, Emory University; Stephen Soumerai, Harvard Medical School and Harvard Pilgrim Health Care; Julie Zito, University of Maryland, Baltimore (no abstracts provided) Invited Papers Challenges in Using Evidence-Based Practices in Substance Abuse Treatment Chair: Mady Chalk, Ph.D. Monday, June 7 • 2:00 p.m.-3:30 p.m. • Panelists: Kevin Hennessy, Substance Abuse and Mental Health Services Administration; Todd Molfenter, University of Wisconsin, Madison (no abstracts provided) Invited Papers Screening & Intervention for Alcohol & Drug Use Problems in Trauma Patients: If They Improve Public Health & Save Money, Then Why Don’t We Do Them? Chair: Harold Perl, Ph.D. Monday, June 7 • 4:00 p.m.-5:30 p.m. • Panelists: Lawrence Gentilello, UT Southwestern Medical School; Dan Hungerford, Centers for Disease Control and Prevention; Dennis Kelso, San Diego Health and Human Services Agency; Michael Sise, Scripps Mercy Hospital (no abstracts provided)