E-Communication vs. the Phone Payment Issues in Non-Visit Based Communication
advertisement
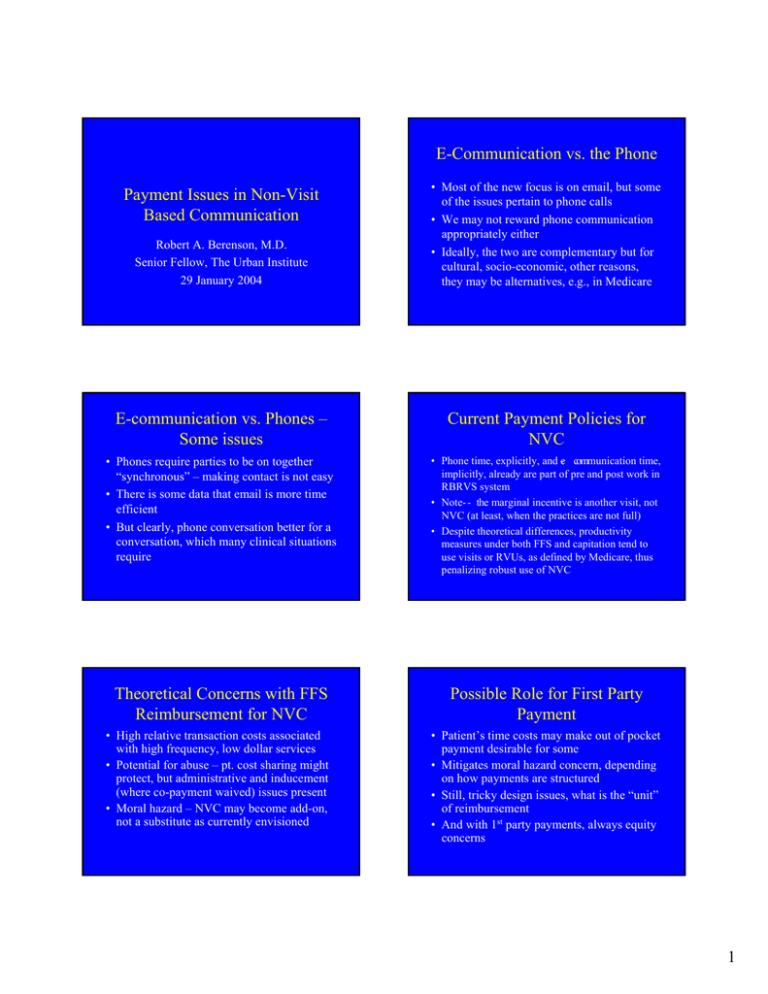
E-Communication vs. the Phone Robert A. Berenson, M.D. Senior Fellow, The Urban Institute 29 January 2004 • Most of the new focus is on email, but some of the issues pertain to phone calls • We may not reward phone communication appropriately either • Ideally, the two are complementary but for cultural, socio-economic, other reasons, they may be alternatives, e.g., in Medicare E-communication vs. Phones – Some issues Current Payment Policies for NVC • Phones require parties to be on together “synchronous” – making contact is not easy • There is some data that email is more time efficient • But clearly, phone conversation better for a conversation, which many clinical situations require • Phone time, explicitly, and -e communication time, implicitly, already are part of pre and post work in RBRVS system • Note- - the marginal incentive is another visit, not NVC (at least, when the practices are not full) • Despite theoretical differences, productivity measures under both FFS and capitation tend to use visits or RVUs, as defined by Medicare, thus penalizing robust use of NVC Theoretical Concerns with FFS Reimbursement for NVC Possible Role for First Party Payment Payment Issues in Non-Visit Based Communication • High relative transaction costs associated with high frequency, low dollar services • Potential for abuse – pt. cost sharing might protect, but administrative and inducement (where co-payment waived) issues present • Moral hazard – NVC may become add-on, not a substitute as currently envisioned • Patient’s time costs may make out of pocket payment desirable for some • Mitigates moral hazard concern, depending on how payments are structured • Still, tricky design issues, what is the “unit” of reimbursement • And with 1st party payments, always equity concerns 1 Increasing Recognition By Private Payers “E-consultation” • Based on pilots some insurers have started reimbursing for an alternative to an office visit – use an intermediary platform, with safeguards re privacy, clinical information, documentation, etc. • AMA CPT panel has recently provided a reimbursement code for e-communication • Insurers still have to decide whether to pay • Prominent insurers which pay for an econsultation include: Blue Shield of Cal., BC/BS of Mass, Horizon BC/BS of N.J. • Although still not widespread, anecdotally in some places, e.g, Southern Cal., more widespread than commonly appreciated • In FFS reimbursement, expansion beyond a structured “consultation” will be hard Implications of Full Range of Internet-based Applications • Many of the potential uses are for administrative purposes and should not require additional payments – should be cost-effective if any scale in practice • Many of the applications should apply to non-physicians, e.g., disease management (phone as well), but no easy way to reimburse in FFS Payment Options for NVC • Voluntary subscription for ecommunication (and associated services) • Fee-for-service payment for defined NVCs • Increase value of current E&M services • Capitation for professional services • Condition-specific care management fee • Pay for performance Potential Uses for Email • Administrative – Rx refills, appointments, test results, etc. • Clinical – – – – – – Q’s and A’s about a condition, treatment, etc. Report self- care information Monitoring chronic conditions Provide educational resources As a substitute for a visit Voluntary Subscription • Payment lies outside of insurance – could be FFS but more likely monthly payment for set of communication services • Market-based solution, without need to standardize and regulate • Patients and payers may view this as “double payments” – • Concern about tiering, equity of access 2 Pay FFS for Defined NVCs Pay for Defined NVCs (cont.) • Some insurers are now paying for a defined “e-consultation” • But applies to relatively small portion of potential NVCs, and not phones • Doesn’t require major change • Can try to assure that new payment only for substitute services, not add-ons • Amenable to incremental expansion • There are difficult boundary issues • Relatively high transaction costs • Limiting NVC payments to substitute services may limit potential, which may lie as much in frequent interactions for patients with chronic conditions • Concern about driving behavior to certain forms of e- communication • Equity concerns, by age and socio - economic class Increase Value of Current E&M Services to Accommodate NVC Increasing Value of E&M (cont.) • Phone time already part of E&M RVUs • Could resurvey either avg. practice or practices that use more NVCs to recalibrate RVU weights • Could use alternative fee schedules for practices that use more or less of NVC • This is the most straightforward approach (unless distinguishing among practices) Capitation • Decision to use NVC -- when and how – lies with the practice • Reduces unique FFS problems, incl. moral hazard, transaction costs, F&A • But capitation is declining • Capitation is permissive but passive, i.e., medical groups still use productivity measures that would penalize NVC • BUT, THE MARGINAL INCENTIVE IS TO DO ANOTHER REIMBURABLE VISIT AND NOT THE NVC • No way to assure that the value of NVCs built into the rates are being provided • Modifying RVUs to achieve desired M.D. behavior change would be new departure Condition-Specific Care Management Fee • Modified form of capitation – essentially a monthly management fee that would require adherence to a set of processes • Could be targeted initially to care for patients with multiple chronic conditions • No preference for the form of NVC, as with capitation • And NVC only one part of the package 3 Care Management Fee (cont.) Pay for Performance • Would the care management fee actually be used as intended? – gets us into a pay for performance or practice oversight situation • If properly applied, only subset of practices could qualify (but could serves as a stimulus to practice redesign?) • Would only applies to part of a practice – assumes some internal cross subsidies • Could pay more for NVC structural processes measures, i.e, distinguishing among practices • Could pay for outcomes that might be better achieved with broader use of NVC • Reserves extra payments for those practices that earn the extra payments • Little experience with pfp for physicians Pay for Performance (cont.) • Paying for NVC structure and process raises program integrity/ accountability issues • Paying for proximate outcomes, again, is a very indirect way for promoting NVC – would the payments be enough and would the practices cross subsidize? • As with all pfp, concern about tiering, i.e., the “rich get richer” at the poor’s expense 4