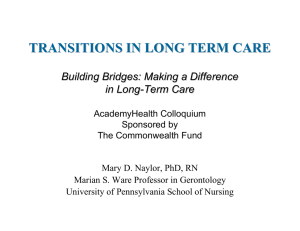
Transitions in Long-Term Care: The Policy Implications 2007 Policy Seminar
advertisement

Transitions in Long-Term Care: The Policy Implications Building Bridges: Making a Difference in Long-Term Care 2007 Policy Seminar Sponsored by The Commonwealth Fund AcademyHealth Washington, D.C. Mary D. Naylor, Ph.D., R.N. Marian S. Ware Professor in Gerontology University of Pennsylvania School of Nursing Goals Make the case that health care quality among elderly long-term care (LTC) recipients who require acute care services may be enhanced by: –avoiding preventable acute hospitalizations; and, –improving transitions to and from hospitals when such transfers are needed Goals Offer policy recommendations to prevent avoidable hospitalizations and enhance necessary care transitions Propose a research agenda to inform future changes in standards of care Number (in millions) Elders 85 and Older: One among the fastest growing age groups in the U.S. SOURCE: Nursing Staff in Hospitals and Nursing Homes: Is it adequate?, 1996; page 33. Acute Hospitals vs. LTC short-term services dominated by medical model providers choose + deliver services high tech limited family involvement Payor: Medicare long-term health, social and housing services providers help with ADLs +IADLs low tech family equal partners Payor: Medicaid Transitions between LTC and Acute Care Hospitals Nature of Problems Poor communication Negative effects of hospitalization Inadequate Gaps discharge planning in care during transfers Consequences High rates of acute clinical events Serious unmet needs Poor satisfaction with care High hospital readmission rates Clinical Barriers to Addressing Problems with Transitions Providers’ resources Limited Dearth knowledge, skills and use of palliative care of quality performance measures Non-Clinical Barriers to Addressing Problems with Transitions Regulatory Financial challenges constraints Pressures from families and health care administrators The Search for Solutions Related Areas of Inquiry Efforts LTC to fully integrate acute and Transitional care interventions targeting chronically ill elders Innovative care models Lessons from Integration Efforts Described the unique issues and challenges confronting acutely ill, frail elders Highlighted the benefits of avoiding preventable hospitalizations Lessons from Integration Efforts Suggested value of: –Early identification of acute care needs –Increased access to selected primary, acute and palliative care services within LTC –Flexible funding and benefits Care Models Designed to Avoid Preventable Hospitalizations Evercare Hospital The at Home Day Hospital Palliative Care Program in LTC Mrs. Anderson: A Case Study Lessons Learned from Transitional Care Interventions Identified individual and system barriers to effective transitions Highlighted importance of multidimensional strategies targeting problems common during “hand-offs Lessons Learned from Transitional Care Interventions Suggested value of: –Nurse-led, interdisciplinary teams –Streamlined care delivery –Information systems that span settings –Quality measures and other incentives Care Models Designed to Improve Care Transitions Care Transitions “Coaching” Intervention Advanced Practice Nurse (APN) Transitional Care Model Mr. Jenkins: A Case Study Policy Recommendations Leutz’s Conceptual Framework Linkage Coordination Full Integration Key Assumptions The financing and delivery of acute and LTC will continue to be characterized by a patchwork of public and private services and funding Key Assumptions There is an adequate evidence base to justify: – increasing access to primary care, management of common conditions and palliative care within LTC; and, – use of nurse directed interdisciplinary teams, guided by evidence-based transitional care protocols Proposed Structures, Incentives to Enhance Coordination of Care Delivery Design, testing and integration of quality measures and monitoring systems Development of information systems that span settings Proposed Structures, Incentives to Enhance Coordination of Care Delivery Preparation of current + future providers emphasizing… – geriatrics – palliative care – interdisciplinary team care – advance care planning – transitional care/care coordination Dissemination of “best practices” Proposed Structures, Incentives to Improve Coordination of Care Benefits Create incentives to foster adoption of evidence-based models of on-site primary or palliative care and transitional care Modify Medicare’s Hospice benefit to minimize barriers for use within LTC Research Agenda Describe impact of transitions Identify most effective and efficient models to: – avoid preventable hospitalizations – improve care coordination, continuity and transitions Define financial and other incentives to optimize quality and cost outcomes