TRANSITIONS IN LONG TERM CARE Building Bridges: Making a Difference in Long -
advertisement

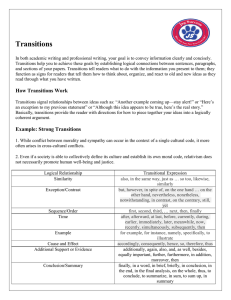
TRANSITIONS IN LONG TERM CARE Building Bridges: Making a Difference in Long-Term Care AcademyHealth Colloquium Sponsored by The Commonwealth Fund Mary D. Naylor, PhD, RN Marian S. Ware Professor in Gerontology University of Pennsylvania School of Nursing Objectives • Demonstrate that health care quality among elders receiving LTC can be enhanced by: – avoiding preventable acute care transitions; and, – improving transitions across acute + LTC when needed. • Propose a research agenda to inform needed changes • Offer policy recommendations to prevent or enhance care transitions Mrs. Anderson: A Case Study Number (in millions) Mrs. Anderson: One among the fastest growing age group (85 and older) in the U.S. Figure 2-2, Nursing Staff in Hospitals and Nursing Homes: Is it adequate? Institute of Medicine, 1996. SOURCE: Bureau of the Census, 1993a. Mrs. Anderson: One of ~15% of NH residents with multiple preventable hospitalizations each year Figure 3-2, Priority Areas for National Action: Transforming Health Care Quality. Institute of Medicine, 2003. Source: Gerard Anderson, Ph.D. Blurred Boundaries, No Connections, Cultural Clashes Acute • short-term services dominated by medical model • providers choose + deliver services • high tech • limited family involvement • Payor: Medicare vs. LTC • long-term health, social and housing services • providers help with ADLs + IADLs • low tech • family equal partners • Payor: Medicaid Initiatives to Integrate Acute + LTC • Multiple models (federal, state, provider) • Effective for a few, but do not address needs of many • Hampered by: – different goals, services – fragmented financing – lack of knowledge and skills – questions re: economic value Lessons Learned from Integration Efforts • Need for increased experimentation with care coordination focused on: – high risk groups receiving acute + LTC services – managing transitions across existing acute + LTC structures Lessons Learned from Integration Efforts (con’t) • Need for care coordination characterized by: – interdisciplinary teams guided by “point person” – evidence-based protocols – information systems – care delivery that spans traditional “silos” – quality control with single point of accountability – flexible benefits and funding Transitions of Elders Between Acute and LTC: State of the Science • Limited research re: patterns of use, reasons, unique challenges and effects of transitions • Knowledge of transitions among chronically ill elders has implications for those receiving LTC Major Findings • Number and nature of transitions • Factors associated with preventable acute care transitions • Factors associated with breakdowns in care across settings • Human and economic consequences Research Agenda • Examine over time number, reasons, unique challenges (for elders and caregivers) and effects of acute care transitions (targetcommunity-based elders) • Identify profile of elders at highest risk for transitions and poor outcomes • Explore factors associated with + and – outcomes Summary • Transitions of elders b/t acute + LTC are increasing at a rapid rate. • High proportions of acute care transitions may be preventable. • Poor and costly outcomes are the norm. • Few studies have explored elders’ and caregivers’ unique issues re: acute + LTC transitions TRANSITIONAL CARE: Transitional Care • Transitional care – broad range of time limited services and environments designed to ensure health care continuity and avoid preventable poor health outcomes among high risk populations as they move from one level of care to another or across settings. Innovations in Transitional Care: State of the Science • Limited research re: benefits + costs of innovations designed to prevent acute care transitions • Findings from interventions targeting chronically ill elders transitioning from hospital to home have helped to define core elements of effective transitions Major Findings • Innovations designed to: –avoid preventable acute care transitions –improve transitions between acute + LTC • Core elements of effective transitions across settings Methodological Challenges • Studying multidimensional interventions in complex settings • Determining the core elements of interventions • Defining severity and risk adjustment measures • Identifying the most sensitive and influential measures • Examining impact of the context of care Challenges to Adoption of Proven Interventions • Defining the best context for services • Securing financial and other incentives that promote… – adoption of “best practices” by LTC – collaboration between hospitals + LTC in improving care transitions • Changing the culture of current practice Measuring the Quality of Transitions in Care • Lack of measures, a major barrier to improving quality • Promising recent efforts • Ongoing challenges: – defining appropriate process and outcome measures – identifying accountable providers and organizations Research Agenda • Define population best served • Compare benefits + costs of alternative models • Identify most efficacious elements of interventions • Design and test quality measures + other incentives • Evaluate “real world” applications of evidence-based models Summary • Nurse led, multidimensional, multidisciplinary interventions have demonstrated great promise. • Core elements are emerging. • Translation of evidence is key. • Future research should emphasize avoiding preventable acute care transitions. Policy Implications • Financial and other incentives needed to: – assure adequate #s of prepared staff – develop integrated information systems – encourage delivery of health services within LTC to avoid preventable transitions – promote use of evidence-based models – reward high quality Policy Implications (con’t) • Integration of robust measures into information systems and national performance standards is priority • Increased research support to address knowledge gaps is essential