Competency Assessment for Population-focused Public Health Practice Susan J. Zahner, DrPH, RN
advertisement

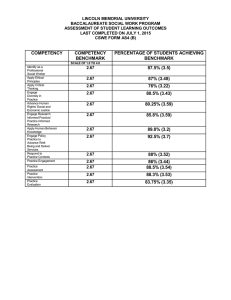
Competency Assessment for Population-focused Public Health Practice Susan J. Zahner, DrPH, RN Jeffrey B. Henriques, PhD Paul M. Schwartz, MS, RN Public Health Systems Research Washington, DC June 7, 2008 Funded by US DHHS/PHS/HRSA, Division of Nursing # D11HP07731-01 Background Statutes emphasize core functions and essential services Changes in practice require new knowledge, skills and attitudes Core competencies for public health professionals published/adapted No standard competency assessment method No prior competency assessment of PHN in Wisconsin Linking Education and Practice for Excellence in Public Health Nursing Statewide academic-practice partnership Improve competency for populationfocused PHN practice • Improved education for students • Improved orientation • Continuing education Baseline assessment Funded by US DHHS/PHS/HRSA, Division of Nursing # D11HP07731-01 Study methods • • UW-Madison IRB approval Self-reported competency assessment instrument (Issel, Baldwin, Lyons, & Madamala, 2006) • • • • • ACHNE/Essential Services (2000) Reliability/validity Length Web-delivered (Websurvey@UW) Cross-sectional baseline survey Competency assessment instrument Stem: “How competent do you feel with your knowledge or skills in each of the following areas?” •9 domains •65 items Response: 1 = I need to be taught about this 2 = I do or can do this with help 3 = I do or can do this 4 = I do this with ease 5 = I do this and teach it to others Issel, Baldwin, Lyons, & Madamala, 2006 Competency assessment instrument domains (item #) • • • • • • • • • Monitoring community health status (13 items) Informing, educating, and empowering populations at risk (4 items) Mobilizing community partnerships (13 items) Policy and planning skills (6 items) Enforcement of laws and regulations (4 items) Linking people to services (4 items) Ensuring a competent workforce (12 items) Evaluating health services (9 items) Researching innovative solutions (6 items) Issel, Baldwin, Lyons, & Madamala, 2006 Survey administration • Wisconsin Health Alert Network • PHN Group email list • Removed state-level PHN addresses • N=471 • Email invitation to participate • Reminder emails at 2 and 3 weeks • April-September 2007 Participant demographics • Mean age • • • Managers 40.0 45.0 50.0 55.0 Full-time staff Years Part-time staff • • Response rate = 63.5% (299/471) Female (97.8%) White, non-Hispanic (97%) Part-time staff (n=76) Full-time staff (n=153) Managers (n=42) Years in public health Managers Full-time staff Part-time staff 0.0 10.0 20.0 Years 30.0 Highest degree earned 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Graduate degree Baccalaureate degree Part-time staf f Full-time staf f Managers Scale reliability 6 Research 9 Evaluate 12 Workforce Link 4 Enforce 4 6 Policy 13 Partner 4 Inform 13 Monitor 0.8 0.85 0.9 Cronbach's Alpha 0.95 1 Mean responses by domain Linking 3.59 (0.78) Informing 2.83 (0.83) Mobilizing 2.78 (0.73) Ensuring 2.78 (0.72) Enforcing 2.70 (0.89) Researching 2.47 (0.72) Monitoring 2.44 (0.76) Planning 2.31 (0.78) Evaluating 2.24 (0.77) n= 296-299 1 2 3 4 5 Mean responses by domain and type of respondent ^ Linking Informing *^ Mobilizing Ensuring * Enforcing *^ Researching *^ Monitoring *^ Part-time staff Full-time staff Managers * Planning *^ Evaluating 1 2 3 4 5 Significance at alpha <.05 via one-tailed Tukey B post-hoc comparison: * = Managers/full-time ^ = Full-time/part-time Limitations-sample Group email list incomplete and voluntary Under-representation of PHN by region of state Limited generalizability Limitations-instrument Self-assessed perceptions versus observed competency Response category “5” may not reflect the same concept as “1 – 4” responses “doing with help” Discussion WI PHN workforce is: • • • Well educated Experienced Aging Discussion Competency low in most domains Higher perceived competency in traditional areas of practice Higher perceived competency in managers compared to staff Higher competency in full-time compared to part-time staff Discussion Competency assessment instrument: Reliable Length Compare with other competency assessment tools Use by other public health professionals Conclusion Change in practice for staff PHN toward more systems-level activity based on essential services will require additional training and support to achieve perception of competency Next steps • LEAP Project activities • Academia/practice regional learning collaboratives • Orientation program • Continuing education • Follow-up survey • Comparison with Illinois References Issel, L. M., Baldwin, K. A., Lyons, R. L., & Madamala, K. (2006). Self-reported competency of public health nurses and faculty in Illinois. Public Health Nursing, 23(2), 168-177. Public Health Functions Steering Committee. (1994). The public health workforce: An agenda for the 21st century. Full report of the Public Health Functions Project. Washington, DC: U.S. Department of Health and Human Services, Public Health Service. Quad Council of Public Health Nursing Organizations. (2004). Public health nursing competencies. Public Health Nursing., 21(5), 443-452. Wisconsin Department of Health & Family Services. (2005). Public Health Profiles for Wisconsin. Retrieved October 22, 2007, from http://dhfs.wisconsin.gov/localdata/pubhlthprofiles.htm Questions? Contact: Susan Zahner, DrPH, RN Associate Professor UW-Madison H6/246 CSC 600 Highland Avenue Madison, WI 53792-2455 608-263-5282 sjzahner@wisc.edu