Postprandial activation of hemostatic factors: Role of dietary fatty acids
advertisement

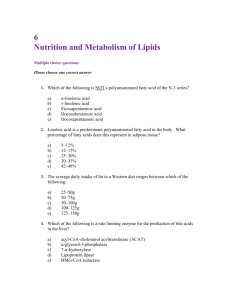
ARTICLE IN PRESS Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 www.elsevier.com/locate/plefa Review Postprandial activation of hemostatic factors: Role of dietary fatty acids Asim K. Duttaroy Department of Nutrition, Faculty of Medicine, University of Oslo, POB 1046 Blindern, N-0316 Oslo, Norway Received 20 October 2004; accepted 30 March 2005 Abstract Intake of dietary fat is an important determinant of the plasma concentration of triacylglycerol-rich lipoproteins, and the degree of alimentary lipemia is reported to have effects on hemostatic status including platelet function. Although association between the amount of dietary fat intake, lipemic response and certain cardiovascular disease (CVD) risk factors (VIIa and PAI-1) has been reported, the significance of the fatty acid composition of ingested fat for the postprandial lipid concentrations and the hemostatic factors is still unclear. Accumulating evidence suggests a relationship between dietary fatty acids and emerging hemostatic CVD risk factors, although much of this evidence is incomplete or conflicting. In order to improve our knowledge in this area, sufficient sample size in future studies are required to take into account of the genetic variation (gene polymorphisms for VII, PAI-1), sex, physical activity, stage of life factors, and sufficient duration to account for adaptation for definitive conclusions. r 2005 Elsevier Ltd. All rights reserved. 1. Introduction The roles of dietary fat in the etiology of cardiovascular disease (CVD) have been extensively studied [1–3]. In view of these studies, dietary fat intakes currently been recommended to help prevent CVD are based mainly on the well-known effects of different dietary fatty acids on plasma lipids. Both the postprandial and fasting plasma lipids are thought to be associated with CVD [2]. In fact, evidence continues to accrue for disturbances in coagulation, fibrinolysis and platelet behavior in hyperlipidemic states, which together might constitute a prothrombotic state [4–10]. Both the amount and composition of dietary fat may affect the hemostatic system (Fig. 1). The magnitude of the postprandial lipemic response appears to play a role in the etiology and progression of CVD and a slow return to the postabsorptive state may be specifically associated with an increased risk of CVD [11,12]. There is increasing evidence that an elevated concentration of Tel.: +47 22 85 15 47; fax: +47 22 85 13 41. E-mail address: a.k.duttaroy@medisin.uio.no. 0952-3278/$ - see front matter r 2005 Elsevier Ltd. All rights reserved. doi:10.1016/j.plefa.2005.03.003 triacylglycerol-rich lipoproteins in the postprandial state may be responsible for atherogenesis by activating hemostatic factors [13,14]. This issue has added importance because several hemostatic and fibrinolytic factors are known CVD risk factors [15–18]. The coagulation, fibrinolytic, and platelet activating systems are complex and interact extensively with each other [19,20] and therefore subtle changes in the balance between these factors in hyperlipidemia can promote CVD [21,22]. Many of the key reactions require participation of biomembranes, suggesting that dietary lipids, to the extent that they influence lipid composition of the membranes and/or affect levels of plasma lipoproteins, may have an important regulatory role in the activation of the hemostatic system. Not surprisingly, considerable effort has been expended to determine if dietary fatty acids can influence CVD risk through effects on the hemostatic process. It has become increasingly clear that not all the effects of dietary fatty acids on CVD risk can be explained by the effects of fatty acids on traditional lipid/lipoprotein risk factors. Therefore, a better understanding of the relationship between diet and hemostasis is essential in order to ARTICLE IN PRESS 382 A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 Fig. 1. Interaction of dietary lipids with hemostatic factors: dietary lipids can affect both the postprandial lipemic response as well as activation of the hemostatic factors including platelet function. These effects may depend on the amount and composition of dietary lipids. develop therapeutic interventions that maximally reduce CVD risk. Dietary lipids play important roles in the development of CVD, as they regulate several processes such as membrane fluidity, membrane receptor expression and function, eicosanoid synthesis, fasting and postprandial plasma levels of lipids, and blood platelet function by modifying cell membrane fatty acid composition, and gene expression. However, the mechanisms involving transient activation of hemostatic system during postprandial lipemia are not understood. This review primarily addresses the roles of dietary fatty acids on immediate transient perturbations in circulating lipoprotein and their relationships with the hemostatic factors, including platelet response after a meal. 2. Dietary fatty acids and their hyperlipidemic response Dietary fat is composed principally of triacylglycerol, which after digestion and absorption stimulates the production of chylomicrons [2,13,23–29]. An intake of 40–50 g of fat in a meal results in significant lipemia in healthy adults, with consecutive fat-containing meals enhancing the lipemia [30]. Therefore, limiting fat intake to approximately 30 g on each eating occasion may minimize postprandial lipemia. The magnitude of the postprandial lipemic response, however, is determined by several factors such as amount and composition of fat intake, fasting plasma triacylglycerol concentration, age, lifestyle, and habitual dietary fat composition [31]. Impaired clearance of chylomicron remnants is associated with increased risk of atherosclerosis and CVD [2,11,23–25,32–35]. A key factor in postprandial lipid metabolism is the activity of the lipoprotein lipase, which plays a role in the clearance of chylomicrons derived from dietary fat [36]. The quantity, degree of saturation, and chain length of fatty acids are suggested to affect lipoprotein lipase activity [37]. The regulation of triacylglycerol-rich lipoproteins hydrolysis by lipoprotein lipase is, however, not fully understood. It was suggested that the adipose tissue is the site of a set of mechanisms involved in the regulation of lipoprotein lipase [13,38]. Cholesterol ester transfer protein (CETP) also plays an important role in this regard as it exchanges cholesteryl esters and triacylglycerol between triacylglycerol-rich lipoproteins and HDL and LDL particles[38–41]. CETP activity in the late postprandial phase may determine to what extent impaired clearance of plasma triacylglycerol-rich lipoproteins is atherogenic [41]. An increase in CETP activity is suggested to be associated with the degree of lipemia, as seen in dyslipemic plasma. Fasting CETP activity has been shown to be affected by dietary fatty acid composition [42]. Postprandial studies indicated an increase in CETP activity after intake of fatty meals, the increase being higher after polyunsaturated fatty acid than after monounsaturated fatty acid intakes [43]. Several proteins in the adipose tissue responsible for lipid metabolism are regulated by nuclear hormone receptors, peroxysome proliferator-activated receptors (PPARs), liver X receptors (LXRs), retinol X receptor (RXR), hepatic nuclear receptor a (HNFa, sterol regulatory element binding protein 1c (SREBP1c) that use lipids such as fatty acids, sterols, as their ligands [44–47]. Phenotype analyses of knock-out or transgenic mice pointed out the respective role of the orphan nuclear receptors and their heterodimeric partner RXR. These transciptional regulations have several targets: the P450 cytochromes involved in the bile acid synthesis Cyp7a1 and Cyp8b1; the intestinal bile acid binding protein, CETP and phospholipid transfer protein, both involved in the HDL catabolism; the ABC cholesterol transporters, proteins for fatty acid transport, and oxidation [48,49]. At present, important information is lacking as to how postprandially derived fatty acids affect expressions of genes through these nuclear receptors that may influence the postprandial activation of the hemostatic factors. Moreover, very little information is available on the roles of nuclear transcription factors which may lead to an effective fatty acid trapping by the adipose tissue that may prevent some of the undesirable effects resulting from elevated plasma non-esterified fatty acid concentrations. In the near future, the identification and study of new target genes in the adipose tissue by transcriptomic or proteomic analyses will allow a better understanding of lipid homeostasis in physiological as well as pathophysiological conditions. In metabolic studies, variable effects of individual fatty acids on plasma lipid and lipoprotein levels have been observed [30,50]. Postprandial studies have also focused on comparisons of the effect of a single fatty meal on the lipemic responses of CVD patients and healthy individuals [51]. The results of postprandial studies have often proved inconsistent, possibly due to differences in experimental design, such as meal composition and the ARTICLE IN PRESS A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 background diets, and type of volunteer. Specifically, saturated fatty acids, with 12–16 carbon atoms tend to increase plasma total and LDL cholesterol levels, whereas stearic acid, 18:0, does not have a cholesterolraising effect, but may lower HDL cholesterol, and increase Lp(a) concentration [52]. The prevalence of stearic acid, 18:0, in the Western diet is likely to increase with the introduction of synthetic fats designed to have minimal effect on plasma cholesterol concentration; its influence on hemostasis remains uncertain [32,53]. A higher increase in triacylglylcerol-rich lipoproteins was observed after consumption of the test fat containing myristic acid, 14:0, than after those containing palmitic acid, 16:0, or lauric acid, 12:0 [38], but the data are not entirely consistent [5,54]. There is general agreement that butter fat (which contains short-chain and medium-chain saturated fatty acids), but not fats containing long-chain saturated fatty acids, result in higher postprandial lipemic responses than consumption of monounsaturated fatty acids and polyunsaturated fatty acids [54,55]. Among the cholesterol-raising saturated fatty acids, myristic acid, 14:0, appears to be more potent than lauric acid, 12:0, or palmitic acid, 16:0, Stearic acid, 18:0) is unique amongst the saturated fatty acids of similar chain length because it is considered to have little or no effect on plasma cholesterol concentration [56–58]. Oleic acid, 18:1n-9, is an effective hypocholesterolaemic agent and, as one of the key components in the increasingly advocated Mediterranean-style diet, has been hailed as a potential tool in the prevention of CVD [59,60]. Claims have been made of both beneficial and detrimental alterations in hemostasis when diets are supplemented with, or contain large amounts of, oleic acid [33,60]. Trans fatty acids appear to increase LDL cholesterol levels compared with oleate [61]. Linoleic acid, 18:2n-6, has cholesterol-lowering effects [62], whereas n-3 long-chain polyunsaturated fatty acids (LCPUFA) decrease the incidence of postprandial lipemia [36,63]. A background diet containing excess of n-3 LCPUFA decreases postprandial lipemia by stimulating lipoprotein lipase expression and decreasing very low-density lipoprotein (VLDL) synthesis [36,64]. However, no such effects were observed in case of alpha linolenic acid, 18:3n-3 [65]. Diet and/or drug treatments that lower the level of triacylgylcerol-rich lipoproteins in the fasted state also tend to have a beneficial effect on postprandial lipoprotein levels. To date, however, firm conclusions of how specific fatty acids influence postprandial response have not been reached [66–69]. 3. Structure of triacylglycerols on postprandial lipemic response The positional distribution of fatty acids in triacylglycerols varies greatly among fats and oils of different origin. The lipases in the digestive tract hydrolyze the 383 fatty acids in the sn-1 and sn-3 positions, whereas the long-chain fatty acids in the sn-2 position predominantly remain in this location and are absorbed as 2-monoacylglycerols [70]. Because the long-chain saturated fatty acids can form insoluble soaps with Ca2+ and Mg2+ in the gut, stearic acid, 18:0, and palmitic acid, 16:0, are better absorbed if situated in the sn-2 position than if situated in the sn-1 and sn-3 positions [71]. Furthermore, saturated fatty acids in the sn-2 position of dietary triaclylcglycerols have been shown to slow down the clearance of chylomicrons in animals. The 2-monoacylglycerols may remain on the chylomicron surface, causing changes in the physical properties of the surface layer. Therefore, the positional distribution of saturated fatty acids may influence lipid metabolism postprandially [25]. Because triacylglycerols with saturated fatty acids in the sn-2 position may be absorbed more efficiently and cleared from circulation more slowly than triacylglycerols with saturated fatty acids in the sn-1 and sn-3 positions, feeding these dietary triacylglycerols may result in a more pronounced postprandial lipemia. However, several studies [13,29,66] found no significant differences in plasma lipids after meals with triacylglycerols of different positional distributions. The fatty acid composition of a diet has an effect on the fatty acid composition of VLDL triacylglycerols and consequently possibly also on the positional distribution of fatty acids in VLDL triacylglycerols [28,71,72]. The relationship between triacylglycerol molecular structures in dietary fats, chylomicrons, and triacylglycerols provides new means for understanding the effects of fatty acid positional distribution on human lipid metabolism [70]. 4. Postprandial lipemia and cardiovascular disease Postprandial triglyceridemia may represent a procoagulant state involving disturbances of both blood coagulation and fibrinolysis, in particular due to elevation of the plasma levels of activated factor VII (FVIIa) and plasminogen activator inhibitor (PAI-1) [9,10,73,74]. Disturbances of the hemostatic system therefore may, at least in part, account for by the link between hypertriglyceridemia and coronary heart disease. Experimental results and clinical trial data suggest that plasma accumulation of remnant lipoproteins is not just an associated feature of an atherogenic lipoprotein profile but triacylgylcerol-rich lipoproteins remnants themselves contribute to the pathogenesis of atherosclerosis [22,75]. The Northwick Park Heart Study was a prospective study in which FVII levels were found to be strongly associated with coronary risk. This study showed that elevated factor VII levels were related to fatal myocardial infarctions but not to nonfatal myocardial ARTICLE IN PRESS 384 A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 infarctions [76]. The Atherosclerosis Risk in Communities Study, a prospective study of hemostatic factors and the prevalence of coronary heart disease, showed no association of coronary disease with FVII [77]. In this study, only elevated levels of fibrinogen, FVIII, and von Willebrand factor were identified as risk factors associated with coronary heart disease, but their measurement in healthy subjects did not seem to be beneficial beyond more established risk factors. In the Prospective Cardiovascular Munster study, FVIIc levels were elevated in patients who had coronary events, but, after multiple logistic regression analysis, FVIIc was not identified as an independent risk factor for coronary events [78]. The results of the Survival of Myocardial Infarction Long-Term Evaluation study demonstrated that a genetic propensity to high factor VII levels is not associated with a risk for myocardial infarction. Another prospective study, the Edinburgh Artery Study, also failed to confirm FVII as an independent predictor of coronary disease [79]. Factor VIIa is the first enzyme of the blood coagulation system and serves a priming function for triggering of the clotting cascade [80,81]. FVII circulates mainly in an inactive, single-chain form. The two-chain form, FVIIa, circulates at much lower concentration, but is many times more active than the single-chain form. The coagulant activity of factor FVII (FVIIc, total activity of FVII in plasma) was identified as an independent predictor of myocardial infarction in initially healthy middle-aged men, and particularly of fatal coronary events [82,83]. Both serum cholesterol and triglyceride concentrations correlated positively with the FVIIc level in this study. Addition of fat to diet has been consistently shown to cause a rapid conversion of the FVII zymogen into its active form (FVIIa), whereas the concentration of total protein is unaffected [9]. Postprandial activation of FVII is dependent on lipolytic activity and it is mainly supported by large triglyceride-rich lipoprotein of the VLDL class [23,84–86]. Since FVIIa–tissue factor (TF) complex is responsible for the initiation of the coagulation cascade, increased generation of FVIIa in the postprandial state would increase the potential for thrombin production in the event of plaque rupture [87]. When the vascular lumen is damaged, TF is exposed and then binds to the small amounts of circulating factors FVIIa and FVII. This facilitates conversion of FVII to FVIIa. FVIIa bound to TF in the presence of calcium and phospholipids facilitates the conversion of factor IX to factors IXa and X to factor Xa (Fig. 2) [88,89]. Aberrant TF expression triggers intravascular thrombosis in atherosclerosis, and other diseases. The plasma levels of FVII are determined by genetic and environmental factors [90,91]. Plasma FVII levels increase with age and are higher in females and in persons with hypertriglyceridemia [4,9,15,17,84,92–94]. Fig. 2. Factor VIIa and blood coagulation cascade. Activated factor VIIa is generated by tissue factor (TF). Ultimately, prothrombinase complex (FXa, Va, and platelets) which cleaves prothrombin to thrombin. Thrombin then generates fibrin polymers by proteolytic cleavage of fibrinogen, and also initiates platelet aggregation. FXa, activated factor X, FX , factor X, FVa, activated Factor V, PC, phosphatidylcholine, PS, phosphartidylserine. The relationship between diet and FVII is conflicting [8,19,35,53,86,95–99]. The high-fat meals led to variable increase in FVIIc and FVIIa. The degree of postprandial lipemia was correlated with the postprandial increase in FVIIc. Roche and Gibney suggested that FVIIc rose more rapidly with meals containing a high proportion of oleic acid [100]. However, Larsen et al. [101] found no differences in the postprandial response of plasma triacylglycerol and FVIIc following five meals containing 70 g fat provided by rapeseed, olive, sunflower, palm oils and butter. However, in that study the fat was administered over two meals. Mennen et al. reported increased FVIIa following 50 g fat test meals enriched with approximately 20 g palmitate or stearate or linoleate or linoleate and linolenate in elderly women [67]. Sanders and his colleagues [24,102,103] reported that that dietary oleate increased FVIIa to a greater extent than stearate or medium-chain triacylglycerols. However, we [66] did not find that 1,3 distearoyl-2oleolyl glycerol differed significantly from triolein with regard to its effects on plasma triacylglycerol or FVIIa at 3 h after a test meal in eight male subjects. Meals high in triacylglycerol containing palmitic, oleic, elaidic, linoleic and linolenic acids result in a postprandial increase in FVIIa nd that a low-fat meal leads to a fall in FVIIc. Randomized stearic acid-rich fats result in less postprandial lipemia and a lower postprandial increase in FVIIa, whereas unrandomized cocoa butter results in similar postprandial lipemia and increases in FVIIa compared with oleate [18]. Lindman et al. [104] reported that long-term Mediterranean-type diet favorably modified the fasting levels of FVII (FVIIag, and FVIIa) in individuals with 353Q genotype. FVII is coded by the ARTICLE IN PRESS A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 gene on band 13q34, closely located to the gene for factor X [88,90,105,106]. A strong contribution of the FVII genotype to FVII levels has been observed, and different FVII genotypes can result in up to several-fold differences in mean FVII levels [83,105,107,108]. The major proportion of FVII circulates in plasma in zymogen form, and the activation of the zymogen form results in cleavage of the peptide bond between arginine 152 and isoleucine 153. Thirty different mutations have been identified since the isolation of the FVII gene (F7). Approximately two-thirds of the mutations seem to affect the protease domain, indicating that loss of protease function is the most common cause of the clinical phenotype [109]. FVII activity is influenced by mutations of F7 and by allelic polymorphic variations of the gene. The R353Q polymorphism of the FVII gene has been reported to modify the plasma levels of FVIIc, FVIIa, and total FVII protein [110,111]. This polymorphism is characterized by a guanine to adenine substitution resulting in replacement of the amino acids arginine (R) by glutamine (Q) in codon 353 of FVII protein [112]. Individuals heterozygous or homozygous for the Q allele have been reported to have lower levels of FVII than individuals homozygous for the more common R allele [112]. 5. Plasminogen activator inhibitor-1 PAI-1 is the major physiological inhibitor of the plasminogen activators in the circulation and thereby the principal inhibitor of the fibrinolytic system [113]. Postprandial triglyceridemia has been observed in many, but not all, studies to increase PAI-1 plasma levels, which would further strengthen the chances of thrombotic occlusion of a vessel after rupture of an atherosclerotic plaque [7,32,74,114,115]. Elevated PAI-1 activity has also been shown to be associated with elevated fasting plasma triacylglycerol concentrations, obesity, and the insulin resistance syndrome, and the reduction in plasma triacylglycerol concentrations after weight loss and a fat-modified diet results in increased fibrinolytic activity [99,116]. Fig. 3 shows the relationship between PAI-1 and dietary lipids. The presence of a 4G allele at a common insertion–deletion polymorphism in the promoter of the PAI-1 gene has been associated with elevated plasma PAI-1 concentration and activity [117]. Carriers of the 4G allele may be at increased risk of ischemic heart disease, but this may be dependent on an interaction with other environmental factors. In one study, an increase in PAI-1 activity was reported 8 h after a test meal very high in butter fat in subjects carrying the 4G allele but not in those with the 5G/5G genotype [73]. Fibrinolytic activity increased from fasting values after high-oleate or high-palmitate meals and did not appear to be affected by postprandial 385 Fig. 3. Fibrinolytic pathway and dietary lipids. Fibrinolytic pathway can be activated by several processes, such as intrinsic, extrinsic, and exogenous pathways. PAI-1 can inhibit these processes. PAI-1 can be regulated by dietary fats. PAI-1, plasminogen activator inhibitor type 1, HMWK, high molecular weight kininogen, tPA, tissue plasminogen activator, FXIIa, activated factor XII. lipemia [7]. These observations are consistent with reports of circadian variations in fibrinolytic activity. This increase in fibrinolytic activity is consistent with the decline in PAI-1 activity after the oleate meal [18,24]. These findings suggest that postprandial lipemia induced by oils high in oleate or palmitate does not impair fibrinolytic activity. Kozima et al. [114] reported that PAI-1 antigen concentrations were elevated 8 h after the consumption of 100 g butter. Oakley et al. [24], using a crossover design, compared meals containing 95 g fat provided either by high-oleate sunflower or a mixture of oleate and medium-chain triacylglycerols or butter fat with a low-fat test meal and found that PAI-1 declined from fasting to the same extent with all the four treatments. Byrne et al. [73] reported an increase in PAI-1 activity after a high-fat meal (130 g) in subjects who had an in-dwelling catheter. In this study, PAI-1 activity increased after the test meal between subjects carrying the 4G allele and subjects homozygous for the 5G allele. PAI-1 activity was positively associated with fasting plasma triacylglycerol concentrations. These findings are consistent with the observation that weight loss associated with decreased energy intake and regular physical activity results in improvement in fibrinolytic activity. There are reports that PAI-1 activity in 5G/5G subjects is 40–50% lower than that in subjects who carry one or more 4G alleles. However, the diurnal variations appeared to be greater in subjects with one or more 4G allele. This could be an important source of confounding factors in studies assessing diet–genotype interactions with regard to PAI-1. Meta-analysis of published studies show that the PAI-1 promoter 4G variant is associated with a 30% higher risk of myocardial infarction than that in 5G/5G subjects [118], with little evidence of heterogeneity of effect in subjects from different countries who might be expected to have different dietary habits. ARTICLE IN PRESS 386 A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 6. Dietary fatty acids and platelet function Hyperactivity of platelets, and their adhesion and aggregation at the site of injury in atherosclerotic vessel walls, is critically important in the pathogenesis of CVD [119–121]. Platelet activity is thought to play a major role in the development as well as in the stability of atherosclerotic plaques. In support of the pathophysiological role of platelets, platelet-inhibitory drugs such as aspirin reduce the incidence of myocardial infarction, stroke and death from CVD in secondary prevention trials [122]. Various studies have shown that functional and biochemical parameters of platelets are affected by dietary fatty acids [123,124]. As mentioned earlier, the TF:FVIIa complex activates coagulation cascade which leads to fibrin formation. Although the production of fibrin is usually considered to be the main purpose, thrombin is also a potent platelet-aggregating agent [125]. Thus, postprandial activation of hemostatic factors may initiate platelet activation. Platelets are activated in postprandial lipemia by several mechanisms [6,126]. In vivo platelet activation in hypertriglyceridemic patients was reported by analysis of activationdependent platelet surface antigen, GP53 [127]. Plasma LDLs also activate platelets by modulating Na+ /K+ antiport activity [128]. Postprandial platelet aggregation response to ADP and collagen was lower in the butter intake group compared to those of the control [114]. Stearic acid, 18:0 and trans-fatty acid diets similarly affect platelet activation and endothelial PGI2 production [129]. Platelet aggregation response to collagen increased after both diets, while ADP-induced aggregation showed no diet-induced changes [129,130]. While oleic acid has neutral effect on platelet function [10,56], PUFAs inhibit both collagen and ADP-induced platelet aggregation, but no effect on arachidonic acid (AA)induced aggregation. AA provides adequate substrates for synthesis of circulating vasoactive factors such as prostacyclin (PGI2) (produced by endothelium) and thromboxane A2 (TXA2) (produced by platelets). The ratio of TXA2/PGI2 is an index of the relative activity of the opposing stimuli that modulate vascular tone and platelet activation. The ratio of TXA2/PGI2 in intervillous space could be involved in the mechanism of initiating platelet function. In general, it seems that in diseases where there is a tendency for thrombosis to develop, TXA2 production is elevated whereas PGI2 production may be either elevated or reduced. The opposite is found in some diseases associated with increased bleeding tendency. To serve as the substrate for synthesis of TXA2, AA is liberated from membrane phospholipids by phospholipases (Fig. 4). During activation, exogenous AA can also readily be taken up by platelets. Increased expression of fatty acid translocase (FAT) or CD36 in platelets enhances AA uptake, thus lead to increased TxA2 production [131]. PGI2 Fig. 4. Dietary lipids and platelet activation. Platelets can be activated by different agonists (thrombin, ADP, collagen, TXA2) via their respective receptors on platelet membrane surface. Activated phospholipase C (PLC) then cleaves phosphoinositol pyrophosphate (PIP2) to release diacylglycerol (DAG) and inositol triphosphate (IP3). This mobilizes Ca2+ which in turn activates phospholipase A2 (PLA2). PLA2 then cleaves phospholipids (PL) to liberate arachidonic acid, 20:4n-6 (AA) or eicosapentaenoic acid,20:5n-3 (EPA) to produce thromboxane A2 (from AA) or thromboxane A3 (from EPA). Prostacyclin (PGI2), produced from AA in endothelium, inhibits platelet aggregation through increasing cAMP levels in platelets via activation of its receptor-linked adenylate cyclase. strongly inhibits aggregation of platelets, an effect mediated by stimulation of receptor-linked adenylate cyclase which results in accumulation of cAMP [132]. Linoleic acid, 18:2n-6, rich diet increased PGI2 receptors in human platelets compared with stearate or oleate acid-rich diets without affecting platelet membrane fluidity [56]. An increased amount of dietary n-3 fatty acids reduces AA in tissue lipids by inhibiting its synthesis from its parent molecule, linoleic acid. In addition, eicosapentaneoic acid (20:5n-3) competitively inhibit the oxygenation of AA via the cyclooxygenase and lipoxygenase pathways. The replacement of TXA2 from AA with the less-potent TXA3 from EPA, leads to a marked shift in the TXA2–PGI2 balance which may act to produce an anti-aggregatory state. Modifying platelet aggregation and subsequent adhesion to the blood vessel affected by TXA2–PGI2 interactions suggests a mechanism, already partially realized, for preventing and treating circulatory diseases and tumor metastasis. Dietary fatty acids thus may affect platelet function by modulating AA levels in these cell membranes. 7. Conclusions Dietary lipids are thought to influence the development of CVD via number of processes such as the hemostatic system and platelet function [9,133,134]. In the postprandial state, large triacylglycerol-rich particles can support the assembly and function of coagulation ARTICLE IN PRESS A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 complexes and seem to play a role in the activation of factor VII, PAI-1, and platelets, and thus may explain increased CVD risk associated with increased postprandial triglyceridemia. FVII coagulant activity modestly decreases with reductions in saturated fatty acid intake and thereby may contribute to the beneficial effects of low saturated fatty acid diets. Oleic acid exerts significant beneficial effects on atherosclerosis and thrombosis [34,55,56,135]. The thrombogenic state arises when an imbalance exists between procoagulant and profibrinolytic activity. FVII appears to play a major role in basal thrombin generation, whereas the generation of the fibrinolytic enzyme plasmin is regulated by PAI-1. Reports of postprandial increases in PAI-1 antigen and activity and the demonstration that triacylglycerol-rich VLDLs stimulate the expression and secretion of PAI-1 by endothelial cells in vitro may have clinical significance for this disorder. However, many studies investigating the postprandial effects of lipids suffer limitation that the fat load given is fairly large and unrepresentative of the typical fat content of a meal, meaning that extrapolation of results to real-life situations are not possible. Fundamental gains have been recently made in our understanding of postprandial lipid metabolism in health and disease; however, its relationships with the activation of hemostatic factors are not yet fully understood. In order to improve our knowledge in this area, sufficient sample size in future studies are required to take into account of the genetic variation (gene polymorphisms for VII, PAI-1), sex, physical activity, stage of life factors, and sufficient duration to account for adaptation for definitive conclusions. [8] [9] [10] [11] [12] [13] [14] [15] [16] [17] [18] References [1] M.U. Jakobsen, K. Overvad, J. Dyerberg, M. Schroll, B.L. Heitmann, Dietary fat and risk of coronary heart disease: possible effect modification by gender and age, Am. J. Epidemiol. 160 (2004) 141–149. [2] M. Lefevre, P.M. Kris-Etherton, G. Zhao, R.P. Tracy, Dietary fatty acids, hemostasis, and cardiovascular disease risk, J. Am. Diet. Assoc. 104 (2004) 410–419. [3] J.A. Jakubowski, N.G. Ardlie, F.J. Morgan, C.N. Chesterman, Further observations on the effects of dietary fatty-acid composition on platelet reactivity and blood-coagulation in man and the influence of methodology on findings, Atherosclerosis 41 (1982) 285–294. [4] V.L. Crawford, S.E. McNerlan, R.W. Stout, Seasonal changes in platelets, fibrinogen and factor VII in elderly people, Age Ageing 32 (2003) 661–665. [5] J.C. Hoak, Stearic-acid, clotting, and thrombosis, Am. J. Clin. Nutr. 60 (1994) S1050–S1053. [6] R. Knofler, T. Nakano, K. Nakajima, Y. Takada, A. Takada, Remnant-like lipoproteins stimulate whole blood platelet aggregation in vitro, Thromb. Res. 78 (1995) 161–171. [7] T.A. Sanders, T. de Grassi, J. Acharya, G.J. Miller, S.E. Humphries, Postprandial variations in fibrinolytic activity in middle-aged men are modulated by plasminogen activator [19] [20] [21] [22] [23] [24] [25] 387 inhibitor I 4G-675/5G genotype but not by the fat content of a meal, Am. J. Clin. Nutr. 79 (2004) 577–581. A. Silveira, Postprandial triglycerides and blood coagulation, Exp.Clin. Endocrinol. Diabetes 109 (2001) S527–S532. E.M. Bladbjerg, P. Marckmann, B. Sandstrom, J. Jespersen, Non-fasting factor VII coagulant activity (FVII:C) increased by high-fat diet, Thromb. Haemost. 71 (1994) 755–758. R. Freese, M. Mutanen, Postprandial changes in plateletfunction and coagulation-factors after high-fat meals with different fatty-acid compositions, Eur. J. Clin. Nutr. 49 (1995) 658–664. H.M. Roche, M.J. Gibney, The impact of postprandial lipemia in accelerating atherothrombosis, J Cardiovasc. Risk 7 (2000) 317–324. M. Saigo, S. Abe, M. Ogawa, S. Biro, S. Minagoe, I. Maruyama, H. Toda, K. Kiyonaga, Y. Atsuchi, M. Tahara, K. Mawatari, C. Tei, Plasma level of triglyceride-rich lipoprotein remnants is closely associated with the activation of coagulation factor VII in patients with myocardial infarction, Thromb. Res. 100 (2000) 9–17. L.K. Summers, B.A. Fielding, V. Ilic, P.T. Quinlan, K.N. Frayn, The effect of triacylglycerol-fatty acid positional distribution on postprandial metabolism in subcutaneous adipose tissue, Br.J. Nutr. 79 (1998) 141–147. C.M. Williams, P.A. Bateman, K.G. Jackson, P. Yaqoob, Dietary fatty acids and chylomicron synthesis and secretion, Biochem. Soc. Trans. 32 (2004) 55–58. K.G. Mann, Factor VII assays, plasma triglyceride levels, and cardiovascular disease risk, Arteriosclerosis 9 (1989) 783–784. P.M. Mannucci, Polymorphisms in the factor VII gene and the risk of myocardial infarction, N. Engl. J. Med. 344 (2001) 458–459. G.J. Miller, J.K. Cruickshank, L.J. Ellis, R.L. Thompson, H.C. Wilkes, Y. Stirling, K.A. Mitropoulos, J.V. Allison, T.E. Fox, A.O. Walker, Fat consumption and factor VII coagulant activity in middle-aged men. An association between a dietary and thrombogenic coronary risk factor, Atherosclerosis 78 (1989) 19–24. T.A. Sanders, F.R. Oakley, J.A. Cooper, G.J. Miller, Influence of a stearic acid-rich structured triacylglycerol on postprandial lipemia, factor VII concentrations, and fibrinolytic activity in healthy subjects, Am. J. Clin. Nutr. 73 (2001) 715–721. R.P. Tracy, Diet and hemostatic factors, Curr. Atheroscler. Rep. 1 (1999) 243–248. W. Koenig, Haemostatic risk factors for cardiovascular diseases, Eur. Heart J. 19 (Suppl C) (1998) C39–C43. F.M. Maggi, S. Raselli, L. Grigore, L. Redaelli, S. Fantappie, A.L. Catapano, Lipoprotein remnants and endothelial dysfunction in the postprandial phase, J. Clin. Endocrinol. Metab. 89 (2004) 2946–2950. F. Karpe, Mechanisms of postprandial hyperlipidaemia— Remnants and coronary artery disease, Diabet. Med. 14 (1997) S60–S66. M. Mukherjee, G. Dawson, K. Sembhi, V.V. Kakkar, Triglyceride dependence of factor VII coagulant activity in deep venous thrombosis, Thromb. Haemost. 76 (1996) 500–501. F.R. Oakley, T.A. Sanders, G.J. Miller, Postprandial effects of an oleic acid-rich oil compared with butter on clotting factor VII and fibrinolysis in healthy men, Am. J. Clin. Nutr. 68 (1998) 1202–1207. T.G. Redgrave, D.R. Kodali, D.M. Small, The effect of triacylsn-glycerol structure on the metabolism of chylomicrons and triacylglycerol-rich emulsions in the rat, J. Biol. Chem. 263 (1988) 5118–5123. ARTICLE IN PRESS 388 A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 [26] T.A. Sanders, S.E. Berry, G.J. Miller, Influence of triacylglycerol structure on the postprandial response of factor VII to stearic acid-rich fats, Am. J. Clin. Nutr. 77 (2003) 777–782. [27] J.T. Snook, S. Park, G. Wardlaw, R. Jandacek, D. Palmquist, M.S. Lee, J. Hoover, Chylomicron fatty acid composition and serum lipid concentrations in subjects fed caprenin or palm oil palm kernel oil as the major dietary fat, Nutr. Res. 16 (1996) 925–936. [28] K.M. Yli-Jokipii, U.S. Schwab, R.L. Tahvonen, J.P. Kurvinen, H.M. Mykkanen, H.P.T. Kallio, Triacylglycerol molecular weight and to a lesser extent, fatty acid positional distribution, affect chylomicron triacylglycerol composition in women, J. Nutr. 132 (2002) 924–929. [29] A. Zampelas, C.M. Williams, L.M. Morgan, J. Wright, P.T. Quinlan, The effect of triacylglycerol fatty-acid positional distribution on postprandial plasma metabolite and hormone responses in normal adult men, Br. J. Nutr. 71 (1994) 401–410. [30] T.A. Sanders, Dietary fat and postprandial lipids, Curr. Atheroscler. Rep. 5 (2003) 445–451. [31] E.J. Parks, Recent findings in the study of postprandial lipemia, Curr.Atheroscler.Rep. 3 (2001) 462–470. [32] T. Tholstrup, G.J. Miller, A. Bysted, B. Sandstrom, Effect of individual dietary fatty acids on postprandial activation of blood coagulation factor VII and fibrinolysis in healthy young men, Am. J.Clin. Nutr. 77 (2003) 1125–1132. [33] T.A. Sanders, G.J. Miller, T. de Grass, N. Yahia, Postprandial activation of coagulant factor VII by long-chain dietary fatty acids, Thromb. Haemost. 76 (1996) 369–371. [34] T. Tholstrup, P. Marckmann, J. Hermansen, G. Holmer, B. Sandstrom, Effect of modified dairy fat on fasting and postprandial haemostatic variables in healthy young men, Br. J. Nutr. 82 (1999) 105–113. [35] R. Wilson, K. Lyall, E.M. Millar, L. Smyth, C. Pearson, R.A. Riemersma, Do oxidized fatty acids activate coagulation factor VII during post-prandial lipemia in women?, Thromb. Haemost. 89 (2003) 654–659. [36] Y. Park, W.S. Harris, Omega-3 fatty acid supplementation accelerates chylomicron triglyceride clearance, J. Lipid Res. 44 (2003) 455–463. [37] C.M. Williams, Dietary interventions affecting chylomicron and chylomicron remnant clearance, Atherosclerosis 141 (1998) S87–S92. [38] T. Tholstrup, B. Sandstrom, A. Bysted, G. Holmer, Effect of 6 dietary fatty acids on the postprandial lipid profile, plasma fatty acids, lipoprotein lipase, and cholesterol ester transfer activities in healthy young men, Am. J. Clin. Nutr. 73 (2001) 198–208. [39] R.E. Morton, D.J. Greene, Suppression of lipid transfer inhibitor protein activity by oleate—A novel mechanism of cholesteryl ester transfer protein regulation by plasma free fatty acids, Arterioscl. Thromb. Vasc. Biol. 17 (1997) 3041–3048. [40] H.C.F. Oliveira, E.C.R. Quintao, ‘In vitro’ cholesteryl ester bidirectional flow between high-density lipoproteins and triglyceride-rich emulsions: effects of particle concentration and composition, cholesteryl ester transfer activity and oleic acid, J. Biochem. Biophys. Meth. 32 (1996) 45–57. [41] F. Syeda, C. Senault, B. Delplanque, B. Le Roy, A. Thaminy, D. Gripois, M.F. Blouquit, A. Ruelland, F. Mendy, C. Lutton, Postprandial variations in the cholesteryl ester transfer protein activity, phospholipid transfer protein activity and plasma cholesterol efflux capacity in normolipidemic men, Nutr. Metab. Cardiovasc. Dis. 13 (2003) 28–36. [42] J.E. Groener, E.M. van Ramshorst, M.B. Katan, R.P. Mensink, A. van Tol, Diet-induced alteration in the activity of plasma lipid transfer protein in normolipidemic human subjects, Atherosclerosis 87 (1991) 221–226. [43] S. Jansen, J. Lopez-Miranda, P. Castro, F. Lopez-Segura, C. Marin, J.M. Ordovas, E. Paz, J. Jimenez-Pereperez, F. Fuentes, F. Perez-Jimenez, Low-fat and high-monounsaturated fatty acid diets decrease plasma cholesterol ester transfer protein concentrations in young, healthy, normolipemic men, Am. J. Clin. Nutr. 72 (2000) 36–41. [44] H. Duez, J.C. Fruchart, B. Staels, PPARs in inflammation, atherosclerosis and thrombosis, J. Cardiovasc. Risk 8 (2001) 187–194. [45] C.S. Elangbam, R.D. Tyler, R.M. Lightfoot, Peroxisome proliferator-activated receptors in atherosclerosis and inflammation—an update, Toxicol. Pathol. 29 (2001) 224–231. [46] P.A. Grimaldi, The roles of PPARs in adipocyte differentiation, Prog. Lipid Res. 40 (2001) 269–281. [47] S.A. Khan, J.P.V. Heuvel, Reviews: current topics—role of nuclear receptors in the regulation of gene expression by dietary fatty acids (Review), J. Nutr. Biochem. 14 (2003) 554–567. [48] M. Ricote, A.F. Valledor, C.K. Glass, Decoding transcriptional programs regulated by PPARs and LXRs in the macrophage: effects on lipid homeostasis, inflammation, and atherosclerosis, Arterioscl. Thromb. Vasc. Biol 24 (2004) 230–239. [49] H. Bays, E.A. Stein, Pharmacotherapy for dyslipidaemia— current therapies and future agents, Expert Opin. Pharmacother. 4 (2003) 1901–1938. [50] D. Lairon, Nutritional and metabolic aspects of postprandial lipemia, Reprod. Nutr. Dev. 36 (1996) 345–355. [51] E.H. Temme, R.P. Mensink, G. Hornstra, Effects of medium chain fatty acids (MCFA), myristic acid, and oleic acid on serum lipoproteins in healthy subjects, J. Lipid Res. 38 (1997) 1746–1754. [52] A. Aro, M. Jauhiainen, R. Partanen, I. Salminen, M. Mutanen, Stearic acid, trans fatty acids, and dairy fat: effects on serum and lipoprotein lipids, apolipoproteins, lipoprotein (a), and lipid transfer proteins in healthy subjects, Am. J. Clin. Nutr. 65 (1997) 1419–1426. [53] K.A. Hunter, L.C. Crosbie, G.W. Horgan, G.J. Miller, A.K. Duttaroy, Effect of diets rich in oleic acid, stearic acid and linoleic acid on postprandial haemostatic factors in young healthy men, Br. J. Nutr. 86 (2001) 207–215. [54] T. Tholstrup, B. Vessby, B. Sandstrom, Difference in effect of myristic and stearic acid on plasma HDL cholesterol within 24 h in young men, Eur. J. Clin. Nutr. 57 (2003) 735–742. [55] C. Thomsen, O. Rasmussen, T. Lousen, J.J. Holst, S. Fenselau, J. Schrezenmeir, K. Hermansen, Differential effects of saturated and monounsaturated fatty acids on postprandial lipemia and incretin responses in healthy subjects, Am. J. Clin. Nutr. 69 (1999) 1135–1143. [56] K.A. Hunter, L.C. Crosbie, A. Weir, G.J. Miller, A.K. Duttaroy, A residential study comparing the effects of diets rich in stearic acid, oleic acid, and linoleic acid on fasting blood lipids, hemostatic variables and platelets in young healthy men, J. Nutr. Biochem. 11 (2000) 408–416. [57] F.D. Kelly, N.J. Mann, A.H. Turner, A.J. Sinclair, Stearic acidrich diets do not increase thrombotic risk factors in healthy males, Lipids 34 (Suppl) (1999) S199. [58] F.D. Kelly, A.J. Sinclair, N.J. Mann, A.H. Turner, L. Abedin, D. Li, A stearic acid-rich diet improves thrombogenic and atherogenic risk factor profiles in healthy males, Eur. J. Clin. Nutr. 55 (2001) 88–96. [59] F.H. Mattson, S.M. Grundy, Comparison of effects of dietary saturated, monounsaturated, and polyunsaturated fatty acids on plasma lipids and lipoproteins in man, J. Lipid Res. 26 (1985) 194–202. [60] F. Lopez-Segura, F. Velasco, J. Lopez-Miranda, P. Castro, R. Lopez-Pedrera, A. Blanco, J. Jimenez-Pereperez, A. Torres, J. Trujillo, J.M. Ordovas, F. Perez-Jimenez, Monounsaturated ARTICLE IN PRESS A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 [61] [62] [63] [64] [65] [66] [67] [68] [69] [70] [71] [72] [73] [74] [75] [76] fatty acid-enriched diet decreases plasma plasminogen activator inhibitor type 1, Arterioscl. Thromb. Vasc. Biol. 16 (1996) 82–88. N.M. de Roos, E.G. Schouten, M.B. Katan, Trans fatty acids, HDL-cholesterol, and cardiovascular disease. Effects of dietary changes on vascular reactivity, Eur. J. Med. Res. 8 (2003) 355–357. V. Wijendran, K.C. Hayes, Dietary n-3 and n-6 fatty acid balance and cardiovascular health, Ann. Rev. Nutr. 24 (2004) 597–615. H.M. Roche, M.J. Gibney, Long-chain n-3 polyunsaturated fatty acids and triacylglycerol metabolism in the postprandial state, Lipids 34 (Suppl) (1999) S259–S265. S. Khan, A.M. Minihane, P.J. Talmud, J.W. Wright, M.C. Murphy, C.M. Williams, B.A. Griffin, Dietary long-chain n-3 PUFAs increase LPL gene expression in adipose tissue of subjects with an atherogenic lipoprotein phenotype, J. Lipid Res. 43 (2002) 979–985. Y.E. Finnegan, A.M. Minihane, E.C. Leigh-Firbank, S. Kew, G.W. Meijer, R. Muggli, P.C. Calder, C.M. Williams, Plant- and marine-derived n-3 polyunsaturated fatty acids have differential effects on fasting and postprandial blood lipid concentrations and on the susceptibility of LDL to oxidative modification in moderately hyperlipidemic subjects, Am. J. Clin. Nutr. 77 (2003) 783–795. K.A. Hunter, L.C. Crosbie, A. Weir, G.J. Miller, A.K. Duttaroy, The effects of structurally defined triglycerides of differing fatty acid composition on postprandial haemostasis in young, healthy men, Atherosclerosis 142 (1999) 151–158. L. Mennen, M. de Maat, G. Meijer, P. Zock, D. Grobbee, F. Kok, C. Kluft, E. Schouten, Factor VIIa response to a fat-rich meal does not depend on fatty acid composition—a randomized controlled trial, Arterioscl. Thromb. Vasc. Biol. 18 (1998) 599–603. G.J. Miller, Effects of diet composition on coagulation pathways, Am. J. Clin. Nutr. 67 (1998) 542S–545S. V.V. Salomaa, I. Salminen, V. Rasi, E. Vahtera, A. Aro, G. Myllyla, Association of the fatty acid composition of serum phospholipids with hemostatic factors, Arterioscl. Thromb. Vasc. Biol. 17 (1997) 809–813. H. Mu, C.E. Hoy, The digestion of dietary triacylglycerols, Prog. Lipid Res. 43 (2004) 105–133. K. Yli-Jokipii, H. Kallio, U. Schwab, H. Mykkanen, J.P. Kurvinen, M.J. Savolainen, R. Tahvonen, Effects of palm oil and transesterified palm oil on chylomicron and VLDL triacylglycerol structures and postprandial lipid response, J. Lipid Res. 42 (2001) 1618–1625. K.M. Yli-Jokipii, U.S. Schwab, R.L. Tahvonen, J.P. Kurvinen, H.M. Mykkanen, H.P. Kallio, Chylomicron and VLDL TAG structures and postprandial lipid response induced by lard and modified lard, Lipids 38 (2003) 693–703. C.D. Byrne, N.J. Wareham, N.D. Martensz, S.E. Humphries, J.C. Metcalfe, D.J. Grainger, Increased PAI activity and PAI-1 antigen occurring with an oral fat load: associations with PAI-1 genotype and plasma active TGF-beta levels, Atherosclerosis 140 (1998) 45–53. L. Niskanen, U.S. Schwab, E.S. Sarkkinen, T. Krusius, E. Vahtera, M.I. Uusitupa, Effects of dietary fat modification on fibrinogen, factor VII, and plasminogen activator inhibitor-1 activity in subjects with impaired glucose tolerance, Metabolism 46 (1997) 666–672. M. Weintraub, G. Charach, I. Grosskopf, Disturbances in dietary fat metabolism and their role in the development of atherosclerosis, Biomed. Pharmacotherap. 51 (1997) 311–313. T.W. Meade, V. Ruddock, Y. Stirling, R. Chakrabarti, G.J. Miller, Fibrinolytic activity, clotting factors, and long-term [77] [78] [79] [80] [81] [82] [83] [84] [85] [86] [87] [88] [89] [90] [91] [92] [93] 389 incidence of ischaemic heart disease in the Northwick Park Heart Study, Lancet 342 (1993) 1076–1079. B.B. Duncan, M.I. Schmidt, S. Offenbacher, K.K. Wu, P.J. Savage, G. Heiss, Factor VIII and other hemostasis variables are related to incident diabetes in adults. The Atherosclerosis Risk in Communities (ARIC) Study, Diabetes Care 22 (1999) 767–772. R. Junker, J. Heinrich, H. Schulte, M. Erren, G. Assmann, Hemostasis in normotensive and hypertensive men: results of the PROCAM study. The prospective cardiovascular Munster study, J. Hypertens. 16 (1998) 917–923. A.J. Lee, F.G. Fowkes, G.D. Lowe, J.M. Connor, A. Rumley, Fibrinogen, factor VII and PAI-1 genotypes and the risk of coronary and peripheral atherosclerosis: Edinburgh Artery Study, Thromb. Haemost. 81 (1999) 553–560. C. Hoffman, A. Shah, M. Sodums, M.B. Hultin, Factor VII activity state in coronary artery disease, J. Lab. Clin. Med. 111 (1988) 475–481. R. Junker, J. Heinrich, H. Schulte, L.J. van de, G. Assmann, Coagulation factor VII and the risk of coronary heart disease in healthy men, Arterioscl. Thromb. Vasc. Biol. 17 (1997) 1539–1544. N. Yahia, T.A. Sanders, The influence of dietary fat on postprandial lipaemia and factor VII coagulant activity in human subjects, Proc. Nutr. Soc. 56 (1997) 489–496. D. Girelli, C. Russo, P. Ferraresi, O. Olivieri, M. Pinotti, S. Friso, F. Manzato, A. Mazzucco, F. Bernardi, R. Corrocher, Polymorphisms in the factor VII gene and the risk of myocardial infarction in patients with coronary artery disease, N. Engl. J. Med. 343 (2000) 774–780. d.S. Carvalho, E. Bruckert, P. Giral, C. Soria, J. Chapman, J. Truffert, F. Dairou, J.L. De Gennes, J.P. Caen, Coagulation factor VII and plasma triglycerides. Decreased catabolism as a possible mechanism of factor VII hyperactivity, Haemostasis 19 (1989) 125–130. J.H. Griffin, J.A. Fernandez, H. Deguchi, Plasma lipoproteins, hemostasis and thrombosis, Thromb. Haemost. 86 (2001) 386–394. A.S. Lindman, H. Muller, I. Seljeflot, H. Prydz, M. Veierod, J.I. Pedersen, Effects of dietary fat quantity and composition on fasting and postprandial levels of coagulation factor VII and serum choline-containing phospholipids, Br. J. Nutr. 90 (2003) 329–336. D. Kirchhofer, C. Eigenbrot, M.T. Lipari, P. Moran, M. Peek, R.F. Kelley, The tissue factor region that interacts with factor Xa in the activation of factor VII, Biochemistry 40 (2001) 675–682. J.C. Chan, Gene targeting in hemostasis. Factor VII, Front. Biosci. 6 (2001) D98–D104. P. Golino, The inhibitors of the tissue factor:factor VII pathway, Thromb. Res. 106 (2002) V257–V265. S.E. Humphries, A. Lane, S. Dawson, F.R. Green, The study of gene-environment interactions that influence thrombosis and fibrinolysis. Genetic variation at the loci for factor VII and plasminogen activator inhibitor-1, Arch. Pathol. Lab. Med. 116 (1992) 1322–1329. M. Pinotti, R. Toso, D. Girelli, D. Bindini, P. Ferraresi, M.L. Papa, R. Corrocher, G. Marchetti, F. Bernardi, Modulation of factor VII levels by intron 7 polymorphisms: population and in vitro studies, Blood 95 (2000) 3423–3428. d.S. Carvalho, E. Bruckert, C. Soria, J.P. Caen, Phospholipase C sensitive FVII activity and FVII antigen in hypertriglyceridemia, Nouv. Rev. Fr. Hematol. 31 (1989) 13–15. D. Li, A.J. Sinclair, Plasma coagulation factor VII activity and its correlates in healthy men, Asia Pac. J. Clin. Nutr. 12 (Suppl) (2003) S20. ARTICLE IN PRESS 390 A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 [94] L.I. Mennen, E.G. Schouten, D.E. Grobbee, C. Kluft, Coagulation factor VII, dietary fat and blood lipids: a review, Thromb. Haemost. 76 (1996) 492–499. [95] A.R. Folsom, J. Ma, J.H. Eckfeldt, E. Shahar, K.K. Wu, Plasma phospholipid fatty-acid composition and factor-Vii coagulant activity, Atherosclerosis 111 (1994) 199–207. [96] A.R. Hubbard, L.J. Parr, The effect of phospholipase C on plasma factor VII, Br. J. Haematol. 73 (1989) 360–364. [97] K.A. Mitropoulos, G.J. Miller, B.E. Reeves, H.C. Wilkes, J.K. Cruickshank, Factor VII coagulant activity is strongly associated with the plasma concentration of large lipoprotein particles in middle-aged men, Atherosclerosis 76 (1989) 203–208. [98] P.Y. Scarabin, L. Bara, M. Samama, G. Orssaud, Further evidence that activated factor VII is related to plasma lipids, Br. J. Haematol. 61 (1985) 186–187. [99] H.C. Simpson, J.I. Mann, T.W. Meade, R. Chakrabarti, Y. Stirling, L. Woolf, Hypertriglyceridaemia and hypercoagulability, Lancet 1 (1983) 786–790. [100] H.M. Roche, M.J. Gibney, Postprandial coagulation factor VII activity: the effect of monounsaturated fatty acids, Br. J. Nutr. 77 (1997) 537–549. [101] L.F. Larsen, E.M. Bladbjerg, J. Jespersen, P. Marckmann, Effects of dietary fat quality and quantity on postprandial activation of blood coagulation factor VII., Arterioscl. Thromb. Vasc. Biol. 17 (1997) 2904–2909. [102] T.A. Sanders, T. de Grassi, G.J. Miller, J.H. Morrissey, Influence of fatty acid chain length and cis/trans isomerization on postprandial lipemia and factor VII in healthy subjects (postprandial lipids and factor VII), Atherosclerosis 149 (2000) 413–420. [103] T.A. Sanders, T. de Grassi, G.J. Miller, S.E. Humphries, Dietary oleic and palmitic acids and postprandial factor VII in middleaged men heterozygous and homozygous for factor VII R353Q polymorphism, Am J. Clin. Nutr. 69 (1999) 220–225. [104] A.S. Lindman, J.I. Pedersen, E.M. Hjerkinn, H. Arnesen, M.B. Veierod, I. Ellingsen, I. Seljeflot, The effects of long-term diet and omega-3 fatty acid supplementation on coagulation factor VII and serum phospholipids with special emphasis on the R353Q polymorphism of the FVII gene, Thromb. Haemost. 91 (2004) 1097–1104. [105] M.P. de Maat, F. Green, P. de Knijff, J. Jespersen, C. Kluft, Factor VII polymorphisms in populations with different risks of cardiovascular disease, Arterioscl. Thromb. Vasc. Biol. 17 (1997) 1918–1923. [106] K. Kain, A.J. Catto, J. Young, J. Bamford, J. Bavington, P.J. Grant, Coagulation factor VII activity, Arg/Gln353 polymorphism and features of insulin resistance in first-degree-relatives of South Asian patients with stroke, Thromb. Haemost. 88 (2002) 954–960. [107] L.I. Mennen, M.P. de Maat, G. Meijer, P. Zock, D.E. Grobbee, F.J. Kok, C. Kluft, E.G. Schouten, Postprandial response of activated factor VII in elderly women depends on the R353Q polymorphism, Am. J. Clin. Nutr. 70 (1999) 435–438. [108] X.L. Wang, J. Wang, R.M. McCredie, D.E. Wilcken, Polymorphisms of factor V, factor VII, and fibrinogen genes. Relevance to severity of coronary artery disease, Arterioscl. Thromb. Vasc. Biol. 17 (1997) 246–251. [109] F.H. Herrmann, K. Wulff, K. Auberger, V. Aumann, F. Bergmann, K. Bergmann, E. Bratanoff, D. Franke, M. Grundeis, W. Kreuz, H. Lenk, H. Losonczy, B. Maak, G. Marx, C. Mauz-Korholz, H. Pollmann, M. Serban, A. Sutor, G. Syrbe, G. Vogel, N. Weinstock, E. Wenzel, K. Wolf, Molecular biology and clinical manifestation of hereditary factor VII deficiency, Semin. Thromb. Hemost. 26 (2000) 393–400. [110] F. Green, C. Kelleher, H. Wilkes, A. Temple, T. Meade, S. Humphries, A common genetic polymorphism associated with [111] [112] [113] [114] [115] [116] [117] [118] [119] [120] [121] [122] [123] [124] [125] [126] lower coagulation factor VII levels in healthy individuals, Arterioscler. Thromb. 11 (1991) 540–546. F. Bernardi, P. Arcieri, R.M. Bertina, F. Chiarotti, J. Corral, M. Pinotti, H. Prydz, M. Samama, P.M. Sandset, R. Strom, V.V. Garcia, G. Mariani, Contribution of factor VII genotype to activated FVII levels. Differences in genotype frequencies between northern and southern European populations, Arterioscler. Thromb. Vasc. Biol. 17 (1997) 2548–2553. D. Green, M.A. Chamberlain, K.J. Ruth, A.R. Folsom, K. Liu, Factor VII, cholesterol, and triglycerides. The CARDIA Study. Coronary Artery Risk Development in Young Adults Study, Arterioscler. Thromb. Vasc. Biol. 17 (1997) 51–55. A. Hamsten, U. de Faire, G. Walldius, G. Dahlen, A. Szamosi, C. Landou, M. Blomback, B. Wiman, Plasminogen activator inhibitor in plasma: risk factor for recurrent myocardial infarction, Lancet 2 (1987) 3–9. Y. Kozima, T. Urano, K. Serizawa, Y. Takada, A. Takada, Impaired fibrinolytic activity induced by ingestion of butter: effect of increased plasma lipids on the fibrinolytic activity, Thromb. Res. 70 (1993) 191–202. H. Oda, M. Ohno, H. Ohashi, Coagulation and fibrinolysis factors in dialysis patients with and without ischemic heart disease, Adv. Perit. Dial. 16 (2000) 152–155. A. Asplund-Carlson, A. Hamsten, B. Wiman, L.A. Carlson, Relationship between plasma plasminogen activator inhibitor-1 activity and VLDL triglyceride concentration, insulin levels and insulin sensitivity: studies in randomly selected normo- and hypertriglyceridaemic men, Diabetologia 36 (1993) 817–825. S. Ye, F.R. Green, P.Y. Scarabin, V. Nicaud, L. Bara, S.J. Dawson, S.E. Humphries, A. Evans, G. Luc, J.P. Cambou, The 4G/5G genetic polymorphism in the promoter of the plasminogen activator inhibitor-1 (PAI-1) gene is associated with differences in plasma PAI-1 activity but not with risk of myocardial infarction in the ECTIM study. Etude CasTemoins de I’nfarctus du Mycocarde,, Thromb. Haemost. 74 (1995) 837–841. J.P. Ioannidis, E.E. Ntzani, T.A. Trikalinos, D.G. ContopoulosIoannidis, Replication validity of genetic association studies, Nat. Genet. 29 (2001) 306–309. S. Butenas, C. van’t Veer, K.G. Mann, ‘‘Normal’’ thrombin generation, Blood 94 (1999) 2169–2178. A.K. Duttaroy, Dietary components and human platelet activity, Platelets 13 (2002) 67–75. S. Goto, Understanding the mechanism of platelet thrombus formation under blood flow conditions and the effect of new antiplatelet agents, Curr. Vasc. Pharmacol. 2 (2004) 23–32. A.K. Duttaroy, M.J. Gordon, C. Kelly, K. Hunter, L. Crosbie, T. Knight-Carpentar, B.C. Williams, Inhibitory effect of Ginkgo biloba extract on human platelet aggregation, Platelets 10 (1999) 298–305. C.M. Nieuwenhuys, G. Hornstra, The effects of purified eicosapentaenoic and docosahexaenoic acids on arterial thrombosis tendency and platelet function in rats, Biochim. Biophys. Acta 1390 (1998) 313–322. G.J. Nelson, P.S. Schmidt, G.L. Bartolini, D.S. Kelley, D. Kyle, The effect of dietary docosahexaenoic acid on platelet function, platelet fatty acid composition, and blood coagulation in humans, Lipids 32 (1997) 1129–1136. A.K. Duttaroy, T.K. Ray, A.K. Sinha, Prostacyclin Stimulation of the Activation of Blood-Coagulation Factor-X by Platelets, Science 231 (1986) 385–388. D.A. Hyson, T.G. Paglieroni, T. Wun, J.C. Rutledge, Postprandial lipemia is associated with platelet and monocyte activation and increased monocyte cytokine expression in normolipemic men, Clin. Appl. Thromb. Hemost. 8 (2002) 147–155. ARTICLE IN PRESS A.K. Duttaroy / Prostaglandins, Leukotrienes and Essential Fatty Acids 72 (2005) 381–391 [127] F.H. de Man, R. Nieuwland, L.A. van der, F. Romijn, A.H. Smelt, J.A. Gevers Leuven, A. Sturk, Activated platelets in patients with severe hypertriglyceridemia: effects of triglyceridelowering therapy, Atherosclerosis 152 (2000) 407–414. [128] J.R. Nofer, M. Tepel, B. Kehrel, S. Wierwille, M. Walter, U. Seedorf, W. Zidek, G. Assmann, Low-density lipoproteins inhibit the Na+/H+ antiport in human platelets. A novel mechanism enhancing platelet activity in hypercholesterolemia, Circulation 95 (1997) 1370–1377. [129] A.M. Turpeinen, J. Wubert, A. Aro, R. Lorenz, M. Mutanen, Similar effects of diets rich in stearic acid or trans-fatty acids on platelet function and endothelial prostacyclin production in humans, Arterioscler. Thromb. Vasc. Biol. 18 (1998) 316–322. [130] A.M. Turpeinen, A.M. Pajari, R. Freese, R. Sauer, M. Mutanen, Replacement of dietary saturated by unsaturated fatty acids: effects of platelet protein kinase C activity, urinary content of 2,3-dinor-TXB2 and in vitro platelet aggregation in healthy man, Thromb. Haemost. 80 (1998) 649–655. 391 [131] H. Salah-Uddin, M.J. Gordon, I. Ford, N.N. Tandon, M. Greaves, A.K. Duttaroy, Surface expression of fatty acid translocase (FAT/CD36) on platelets in myeloproliferative disorders and non-insulin dependent diabetes mellitus: effect on arachidonic acid uptake, Mol. Cell. Biochem. 239 (2002) 203–211. [132] A.K. Duttaroy, A.K. Sinha, Purification and properties of prostaglandin E1/prostacyclin receptor of human blood platelets, J. Biol. Chem. 262 (1987) 12685–12691. [133] G.J. Miller, Dietary fatty acids and blood coagulation, Prostaglandins Leukot. Essent. Fatty Acids 57 (1997) 389–394. [134] A.K. Duttaroy, Insulin-mediated processes in platelets, erythrocytes and monocytes macrophages—effects of essential fattyacid metabolism, Prostaglandins Leukot. Essent. Fatty Acids 51 (1994) 385–399. [135] E.H.M. Temme, R.P. Mensink, G. Hornstra, Effects of diets enriched in lauric, palmitic or oleic acids on blood coagulation and fibrinolysis, Thromb. Haemost. 81 (1999) 259–263.