PC & Prevention 3/29/11 1
advertisement

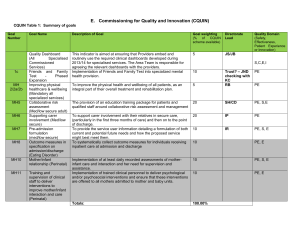
PC & Prevention 3/29/11 1 PC & Prevention 3/29/11 2 PC & Prevention 3/29/11 3 PC & Prevention 3/29/11 4 PC & Prevention 3/29/11 5 PC & Prevention 3/29/11 Increasing recognition that there are systematic differences in health across different population subgroups, i.e., inequity in health, has led to an expanded view of influences on health. In this view, health is viewed as both an average of individuals in the population and the way in which health is distributed in the population. In populations, community and policy contexts have a major role in influencing more proximal influences on health in communities and on individuals in communities. These societal influences operate differently in the various subgroups of the population. It is these factors, rather than those at the community and individual level, that primarily influence distribution of health within the population rather than average of levels of health such as those that are commonly in use in health statistics. Political contexts determine the nature of policies, which, in turn, influence the characteristics of communities: environmental; levels of income and their distribution, e.g., income inequality; power and status relationships; behavioral and cultural characteristics; and health system characteristics. Because they are all influenced by the political context, they potentiate or interact with each other and more directly (through unknown individual characteristics and exposures) influence both health levels as well as distributions of health in individuals, both of which also are affected by demographic characteristics and historical health disadvantage i.e., the tendency of good or poor health to persist for long periods of time in defined geographic areas.1 continued on IH 6891 bn 6 PC & Prevention 3/29/11 continued from IH 6891 an There are only a handful but increasing number of studies concerning the influences of such characteristics on various health needs.2 A focus on influences on the health of populations does not assume a particular pattern of risks among individuals in that population. In this diagram, the individual risk factors are less salient than community and policy characteristics in a political context. Conventionally the province of public health, interventions at these levels have emphasized the extent to which societal factors can be modified to prevent the occurrence of ill health. Thus, prevention is a major thrust of pubic health efforts. Less common is consideration of the extent to which characteristics of these levels contribute to worsening of health where it has already been compromised. In the most recent 20 years, the salience of such activities has become more visible as, for example, the role of health policy in facilitating or interfering with the practices of pharmaceutical companies in marketing retroviral medications for HIV/AIDS. In this sense, the “determinants of disease” and their progression are societal (rather than social), and they operate primarily to alter rates of discomfort, disability, and death rather than occurrence (incidence) of ill health. The other important characteristic of a focus on populations is that it explicitly requires consideration of distributions in the population, i.e., equity in health, as well as average levels of ill health. 1. Cossman JS, Cossman RE, James WL, Campbell CR, Blanchard TC, Cosby AG. Persistent clusters of mortality in the United States. Am J Public Health 2007; 97(12):2148-2150. 2. Starfield B. Pathways of influence on equity in health. Soc Sci Med 2007; 64(7):1355-1362. 7 PC & Prevention 3/29/11 Source: WHO Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Geneva, Switzerland: World Health Organization, 2008. This diagram was proposed by the WHO Commission on the Social Determinants of Health. As such, it focuses on pathways through which inequity in health (“distribution of health and wellbeing”) is achieved. The diagram does not specifically distinguish macro political and economic forces from the policies they engender, nor does it show an impact of individual and community factors (except for the health system) on distribution of health. Its major emphasis appears to be in the reverse direction: that unequal distribution of health influences individual and social phenomena. 8 PC & Prevention 3/29/11 Sources: Clark DW, MacMahon B. Preventive Medicine. Boston, MA: Little, Brown & Company, 1967. Nightengale EO, Cureton M, Kalmar V, Trudeau MB. Perspectives on Health Promotion and Disease Prevention in the United States. Washington, DC: Institute of Medicine, National Academy of Sciences, 1978. National Public Health Partnership. Preventing Chronic Disease: A Strategic Framework. Background Paper. Melbourne, Australia: National Public Health Partnership, 2001. Bentzen N. WONCA Dictionary of General/Family Practice. Copenhagen, Denmark: Laegeforeningens Forlag, 2003. 9 PC & Prevention 3/29/11 10 PC & Prevention 3/29/11 11 PC & Prevention 3/29/11 Sources: Russell LB. Preventing chronic disease: an important investment, but don't count on cost savings. Health Aff 2009;28:42-5. Cohen JT, Neumann PJ, Weinstein MC. Does preventive care save money? Health economics and the presidential candidates. N Engl J Med 2008;358:661-3. 12 PC & Prevention 3/29/11 Interventions that differ widely in cost effectiveness are often equally prioritized, and sometimes interventions of higher cost are prioritized above those with lower cost. Profitability to those who market these interventions sometimes skews recommendations for guideline adherence, e.g., hypertension prevention versus treatment of heart disease. Source: Russell LB. Preventing chronic disease: an important investment, but don't count on cost savings. Health Aff 2009;28:42-5. 13 PC & Prevention 3/29/11 In this chart, the proportions across the preventive measures and across the interventions add to 100; the chart shows what proportions are cost saving, of different degrees of cost effectiveness, and those that actually worsen health. Only about 70% of all recommended interventions are cost effective at conventional levels (less than $50,000 per QALY), 10 to 15% are borderline, and the rest (about 20%) cannot be justified either by cost or by evidence of benefit. Preventive interventions are no more likely to be justified by cost effectiveness than are treatments for existing conditions. Source: Russell LB. Preventing chronic disease: an important investment, but don't count on cost savings. Health Aff 2009;28:42-5. 14 PC & Prevention 3/29/11 15 PC & Prevention 3/29/11 Source: Lawton BA, Rose SB, Elley CR, Dowell AC, Fenton A, Moyes SA. Exercise on prescription for women aged 40-74 recruited through primary care: two year randomised controlled trial. BMJ 2009;337:a2509. 16 PC & Prevention 3/29/11 17 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 18 PC & Prevention 3/29/11 Sources: Schilling FH, Spix C, Berthold F et al. Neuroblastoma screening at one year of age. N Engl J Med 2002; 346(14):1047-1053. Miller AB. Commentary: implications of the frequent occurrence of occult carcinoma of the prostate. Int J Epidemiol 2007; 36(2):282-284. Barry MJ. Screening for prostate cancer--the controversy that refuses to die. N Engl J Med 2009;360:1351-4. 19 PC & Prevention 3/29/11 Source: Mitka M. Guideline supports long-term use of medication to lower prostate cancer risk. JAMA 2009;301:1753-4. 20 PC & Prevention 3/29/11 21 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 22 PC & Prevention 3/29/11 Sources: Kendrick M. Should women be offered cholesterol lowering drugs to prevent cardiovascular disease? No. BMJ 2007;334:983. Cosford PA, Leng GC. Screening for abdominal aortic aneurysm. Cochrane Database of Systematic Reviews 2007; Art. No. CD002945. DOI: 10.1002/14651858.CD002945.pub2. 23 PC & Prevention 3/29/11 Source: Gallacher J. Commentary: Type A behaviour and heart disease: no less inscrutable in Japan. Int J Epidemiol 2008;37:1406-7. 24 PC & Prevention 3/29/11 Source: van den Hoogen PC, Feskens EJ, Nagelkerke NJ, Menotti A, Nissinen A, Kromhout D. The relation between blood pressure and mortality due to coronary heart diseases among men in different parts of the world. N Engl J Med 2000; 342(1):1-8. 25 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 26 PC & Prevention 3/29/11 27 PC & Prevention 3/29/11 This example of risks for tuberculosis in Russia indicates how powerful individual risks may not be most appropriate for interventions to reduce the occurrence of a disease in populations. Source: Coker R, McKee M, Atun R, Dimitrova B, Dodonova E, Kuznetsov S, Drobniewski F. Risk factors for pulmonary tuberculosis in Russia: case-control study. BMJ 2006; 332: 85-7. 28 PC & Prevention 3/29/11 Source: Nelson TF. Research Brief: The Prevention Paradox and a Public Health Approach to College Student Drinking ( http://www.sph.umn.edu/about/pubs/brief/home.html, accessed June 28, 2009). Minneapolis, MN: University of Minnesota School of Public Health, 2009. In a college population, about one-fifth of students report not drinking at all and about three in five report drinking only moderately. Nevertheless, about two in five alcohol-related injuries are in those relatively low drinkers. That is, although the likelihood of deaths associated with alcohol intake is lower in people who drink only lightly or moderately, these individuals combined account for a non-trivial proportion of such deaths in the population. These findings raise issues for policy makers. Should policy decisions about prevention be based on individual or population risk rates? Who should be responsible for carrying out prevention policy – clinical services or public health? 29 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 30 PC & Prevention 3/29/11 31 PC & Prevention 3/29/11 In both of these instances, routine treatment to increase survival of newborns through high concentrations of oxygen and hormone replacement therapy to prevent osteoporosis in postmenopausal women had rates of adverse effects (blindness in the first instance, and high rates of ischemic heart diseases in the second) that outweighed the benefits for which they were intended. 32 PC & Prevention 3/29/11 33 PC & Prevention 3/29/11 Source: Graboys TB. The economics of screening joggers. N Engl J Med 1979; 301(19):1067. The hazards of conducting routine screening in asymptomatic people can be considerable, as shown in this hypothesized example of the estimates of adverse events or death following from exercise stress testing in prospective joggers. One-tenth were estimated to have an abnormal stress test leading to angioplasty; almost two in five of these would have an abnormal finding on angioplasty, of whom about a tenth were estimated to die from complications of the procedure. Two thirds of these people would be found to have multiple-vessel disease and undergo surgery, with an associated 20 deaths per thousand and 40 post-operative infarcts per thousand. (This is equivalent to a 2% death rate and a 8% infarct rate.) That is, over 25 per ten-thousand prospective joggers screened for occult heart disease are estimated to have serious side effects of death ensuing from screening. Although the safety of surgical interventions has improved since these estimates were made, increasing intervention rates ( especially including the placement of stents instead of coronary artery bypass) have increased greatly. The example shows that preventive interventions can have rates of side effects that can approach or exceed the rates of poor outcome from the natural history of illness. 34 PC & Prevention 3/29/11 Source: McGlynn EA, Brook RH. Keeping quality on the policy agenda. Health Aff 2001; 20(3):82-90. 35 PC & Prevention 3/29/11 Adverse effects in the US now are estimated to account for more deaths than all other causes except for heart disease and cancer. In fact, deaths associated with adverse events far exceed the number of deaths associated with the third-leading disease cause of death (stroke). Sources: Leape LL. Unnecessary surgery. Annu Rev Public Health 1992; 13:363-383. McCarthy EG, Widmer GW. Effects of screening by consultants on recommended elective surgical procedures. N Engl J Med 1974; 291 (25):1331-1335. Phillips DP, Christenfeld N, Glynn LM. Increase in US medication-error deaths between 1983 and 1993. Lancet 1998; 351(9103):643-644. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998; 279(15):1200-1205. 36 PC & Prevention 3/29/11 Source: MacDorman MF, Mathews TJ, Martin JA, Malloy MH. Trends and characteristics of induced labour in the United States, 1989-98. Paediatr Perinat Epidemiol 2002; 16(3):263-273. These data from the United States indicate that unwarranted and excessive interventions lead to higher rates of preterm births and neonatal mortality. 37 PC & Prevention 3/29/11 Source: Carlberg B. Time to lower treatment BP targets for hypertension? Lancet 2009;374:503-4. 38 PC & Prevention 3/29/11 Source: Fisher ES, Welch HG. Avoiding the unintended consequences of growth in medical care: how might more be worse? JAMA 1999; 281 (5):446-453. This diagram indicates the caution required before deciding to conduct any intervention. It has been said that “a healthy person is one who has not had enough tests”. Whether preventive or therapeutic, any increase in testing leads to more diagnosis and more treatment – its intended purpose when there is likelihood of a health need. However, ailments that are occult may never progress to a harmful stage: interventions will discover pathology that need not be discovered. Their mere discovery may lead to an unnecessary cascade of other tests and interventions, each with its own chance of adverse effects, with consequent worry, discomfort, and/or disability. 39 PC & Prevention 3/29/11 40 PC & Prevention 3/29/11 Source: Thorpe KE, Florence CS, Howard DH, Joski P. The rising prevalence of treated disease: effects on private health insurance spending. Health Aff 2005; W5: 317-25 (http://content.healthaffairs.org/cgi/reprint/hlthaff.w5.317v1). With progressively decreasing thresholds for diagnosis of disease, and possibly with real increases in some diseases, the prevalence of diseases under treatment is increasing rapidly throughout the world. This chart shows the very large increases in prevalence of particular diseases in the US in the fifteen years between 1987 and 2002. As this information comes from populations with private insurance, the estimates of prevalence undoubtedly understate the true prevalence of disease in the entire population, as people without insurance have more illness. In five of the 10 conditions, the prevalence has more than doubled in the fifteen years; in the case of hyperlipidemia, the prevalence has increased over four-fold. Thus, at the same time that mortality rates have been increasing, the treated prevalence of major illnesses has been increasing. 41 PC & Prevention 3/29/11 Sources: Bodenheimer T, Berenson RA, Rudolf P. The primary care-specialty income gap: why it matters. Ann Intern Med 2007; 146(4):301-306. Tanne JH. US campaign aims to end industry gifts, speaking fees, and travel for doctors. BMJ 2007; 334(7590):385. The intensity of care provided to people over age 65 in the United States increased greatly over the five-year period from 2000-2005. As other studies have shown, excessive rates of interventions are associated with higher adverse event rates. 42 PC & Prevention 3/29/11 43 PC & Prevention 3/29/11 Source: Haug C. The risks and benefits of HPV vaccination. JAMA 2009;302:795-6. 44 PC & Prevention 3/29/11 Source: Fitzpatrick M. Swine flu: public health has become a public nuisance. Br J Gen Pract 2009;59:615. 45 PC & Prevention 3/29/11 46 PC & Prevention 3/29/11 Sources: Vasan RS, Sullivan LM, Wilson PW, et al. Relative importance of borderline and elevated levels of coronary heart disease risk factors. Ann Intern Med 2005;142:393-402. Kaplan RM, Ong M. Rationale and public health implications of changing CHD risk factor definitions. Annu Rev Public Health 2007;28:321-44. 47 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 48 PC & Prevention 3/29/11 Source: Thorpe KE, Howard DH, Galactionova K. Differences in disease prevalence as a source of the U.S.-European health care spending gap. Health Aff 2007;26:w678-86. 49 PC & Prevention 3/29/11 Source: Gervas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet 2008;372:1997-9. 50 PC & Prevention 3/29/11 Source: Medder JD, Kahn NBJ, Sussman JL. Risk factors and recommendations for 230 adult primary care patients, based on U.S. Preventive Services Task Force guidelines. Am J Prev Med 1992;8:150-3. 51 PC & Prevention 3/29/11 Source: Valderas JM, Starfield B, Forrest CB, Sibbald B, Roland M. Ambulatory care provided by office-based specialists in the United States. Ann Fam Med 2009;7:104-11. 52 PC & Prevention 3/29/11 Sources: Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care. Is there enough time for prevention? Am J Public Health 2003; 93(4):635-641. Ostbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med 2005; 3(3):209-214. 53 PC & Prevention 3/29/11 Sources: Bunker JP, Frazier HS, Mosteller F. Improving health: measuring effects of medical care. Milbank Q 1994; 72(2):225-258. Fleetcroft R, Cookson R. Do the incentive payments in the new NHS contract for primary care reflect likely population health gains? J Health Serv Res Policy 2006; 11(1):27-31. 54 PC & Prevention 3/29/11 55 PC & Prevention 3/29/11 56 PC & Prevention 3/29/11 Source: Australian Institute of Health and Welfare. Towards National Indicators of Safety and Quality in Health Care. (www.aihw.gov.au/publications/index.cfm/ title/10792, accessed October 5, 2009). Canberra, Australia: Australian Institute of Health and Welfare, 2009. 57 PC & Prevention 3/29/11 Sources: Lundgren B. Experiences from the Swedish determinants-based public health policy. Int J Health Serv 2009;39:491-507. Dahl E, Lie M. Policies to tackle health inequalities in Norway: from laggard to pioneer? Int J Health Serv 2009;39:509-23. 58 PC & Prevention 3/29/11 Sources: Starfield 2005 Brotman DJ, Walker E, Lauer MS, O'Brien RG. In search of fewer independent risk factors. Arch Intern Med 2005; 165(2):138-145. 59