Pulmonary Mucormycosis presenting as a lung mass in Renal Transplant... Michael Prochaska, MD, Shefali S. Ballal, MD, Yulan...
advertisement

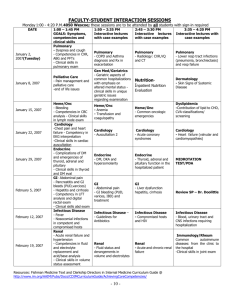
Pulmonary Mucormycosis presenting as a lung mass in Renal Transplant patient– A Case Report Michael Prochaska, MD, Shefali S. Ballal, MD, Yulan Gong, MD, Beth Mapow, DO Department of Pathology, Drexel University College of Medicine, Philadelphia, PA, USA Background Discussion, con’t Mucormycosis is a highly invasive fungal infection caused by fungi in the recently proposed subphylum mucoromycotina and order mucorales 1. It most commonly affects immunocompromised hosts, particularly those with hematologic malignancies and solid transplant recipients2. The mortality has been reported to range between 50% and 80% in cases of localized disease and as high as 98% for disseminated disease 3. Case Presentation We present a 64 year old man who was admitted in January 2015 for progressive shortness of breath and exercise intolerance over a course of 3 months. His past medical history is significant for coronary artery disease and diabetes mellitus. The patient had undergone a renal transplant in February 2013 for end stage renal disease secondary to diabetes mellitus with subsequent episodes of rejection. Chest radiography on admission demonstrated a right upper lobe lung lesion. A subsequent CT chest scan without contrast showed a new gas containing spiculated mass in right upper lobe measuring 2.3 x 3.0 x 2.7 cm. The patient underwent CT guided biopsy of the lesion. Initial adequacy assessment revealed fungal elements and necrosis. The fungal elements were confirmed to be morphologically consistent with mucorales species on histology (Figs1,2). The patient was started on amphotericin B and aggressive surgical debridement and resection of the cavitary lung lesion was recommended. The patient underwent a right upper lobectomy in February 2015. Histology showed lung parenchyma with necrotizing granulomas and angioinvasive fungal organisms morphologically consistent with mucorales species (Figs 3,4). In spite of adequate medical therapy, the patient became clinically unstable and expired shortly thereafter. Discussion Mucor was first described by Paltauf in 1885 4. They are broad, non septated hyphae with right angle branching with predilection for blood vessels causing thrombosis and ischemia 5. Invasive fungal infection including mucormycosis following renal transplant occur in 1-2% of patients in developed countries. The disease manifests at a median of six months posttransplant and is associated with high dosage immunosuppressive therapy6. Figure 1: H&E showing broad non septated mucorales hyphae Figure 2: GMS stain highlighting mucorales hyphae Pulmonary mucormycosis findings on CT scan include lung nodules, cavitation with pleural effusion, and bronchopneumonia7. However the radiographic signs of pulmonary mucormycosis are nonspecific and can be difficult to distinguish from other infections. Hence tissue biopsy is the gold standard for obtaining a diagnosis of pulmonary mucormycosis8. Pulmonary mucormycosis occurs after inhalation of fungal sporangiospores which may spread locally or disseminate systemically. Angioinvasive infections often result in infarction of the affected tissue. Invasion of the large mediastinal vessels can lead to massive hemoptysis which could occasionally be fatal9. The predisposing factors for mucormycosis include ketoacidosis, uncontrolled diabetes mellitus, renal failure, solid tumors, immunosuppressive therapy and solid organ transplantation10. Our patient had multiple risk factors including diabetes mellitus, renal transplant and immunosuppressive therapy. A combination of surgical excision and anti-fungal therapy has been shown to be optimal treatment for mucormycosis along with correction of the underlying condition2,7. Despite aggressive treatment, invasive mucormycosis carries a high mortality rate with the overall mortality for pulmonary mucormycosis being 76%3. Conclusion Figure 3: Section of the lung showing a necrotic brown mass Figure 4: H&E showing fungal hyphae invading the bronchus It is important that clinicians maintain a high degree of suspicion for pulmonary mucormycosis in case of immunocompromised patients. In our case, high clinical suspicion and early radiographic intervention along with tissue diagnosis were crucial in identifying mucormycosis. The patient was actively treated with antifungal and surgical therapy. However the patient’s comorbid conditions contributed to his demise. References 1.Kwon-Chung KJ. Taxonomy of fungi causing mucormycosis and entomohthoramycosis(zygomycosis) and nomenclature of the disease: molecular mycologic perspectives. Clin Infect Dis 2012: 54 (Suppl 1): S8-S15. 2.Hamilos G, Samonis G, Kontoyiannis DP. Pulmonary mucormycosis. Semin Respir Crit Care Med 2011; 32: 693702 3.Roden MM, Zaoutis TE, Buchanan WL et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis 2005; 41: 634-53 4.Pastor –Pons E, Martinez-Leon MI, Alvarez-Bustos G et al: Isolated renal mucormycosis in two patients with AIDS. Am J Roentgenol, 1996; 166(6):1282-84 5.Scully C, OP de Almeida, Sposto MR: The deep mycoses in HIV infection Oral Dis, 1997; 3(Suppl.1):S200-7 6.Einollahi B, Lessan-Pezeshki M, Pourfarziani V et al: Invasive fungal infections following renal transplantation: A review of 2410 recipients. Ann Transplant, 2008; 13(4):55-58 7.Walsh TJ, Gamaletsou MN, McGinnis MR et al: Early Clinical and Laboratory Diagnosis of Invasive Pulmonary, Extrapulmonary, and Disseminated Mucormycosis (Zygomycosis). Clin Infect Dis, 2012; 54(Suppl): S55-60 8.Spellberg B, Edwards J, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev 2005;18:556-69 9.Muqeetadnan M, Rahman A, Amer S, Nusrat S et al. Pulmonary Mucormycosis: An Emerging Infection. Case Reports in Pulmonology. Volume 2012, Article ID 120809, 1-3 10.A. Mohammadi, A. Mehdizadeh, M. Ghasemi-Rad, H.Habibpour, and A. Esmaeli, “Pulmonary mucormycosis in patient with diabetic ketoacidosis: a case report and review of literature,” T¨uberk¨uloz ve Toraks, vol. 60, no. 1, pp. 66–69, 2012.