The Fit Between Stress Appraisal and Dyadic Coping in
advertisement

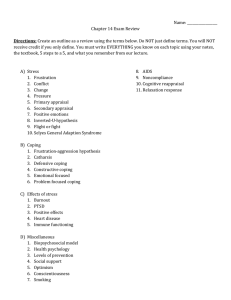
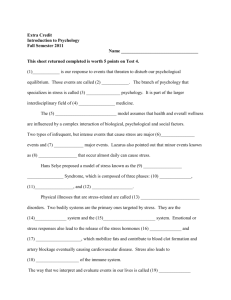
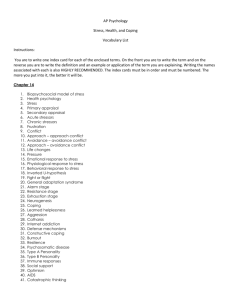
Journal of Family Psychology 2009, Vol. 23, No. 4, 521–530 © 2009 American Psychological Association 0893-3200/09/$12.00 DOI: 10.1037/a0015556 The Fit Between Stress Appraisal and Dyadic Coping in Understanding Perceived Coping Effectiveness for Adolescents With Type 1 Diabetes Cynthia A. Berg, Michelle Skinner, Kelly Ko, and Jorie M. Butler Debra L. Palmer University of Wisconsin–Stevens Point University of Utah Jonathan Butner Deborah J. Wiebe University of Utah University of Texas Southwestern Medical Center This study examined whether perceived coping effectiveness (PCE) was associated with better diabetes management and was higher when adolescents’ dyadic coping was matched to shared stress appraisals. There were 252 adolescents with Type 1 diabetes who completed stress and coping interviews where they appraised mothers’ and fathers’ involvement in stress ownership (mine, indirectly shared, directly shared with parent), in coping (uninvolved, supportive, collaborative, or controlling), and rated their effectiveness in coping. Adolescents completed assessments of depressive symptoms (Children’s Depression Inventory), self-care behaviors (Self-Care Inventory), and efficacy of disease management (Diabetes SelfEfficacy). Glycosylated hemoglobin levels were obtained from medical records. Higher PCE was associated with fewer depressive symptoms, self-care behaviors, and efficacy across age and, more strongly for older adolescents’ metabolic control. Appraisals of support or collaboration from parents were more frequent when stressors were appraised as shared. PCE was enhanced when dyadic coping with mothers (but not fathers) was consistent with stress appraisals (e.g., shared stressors together with collaborative coping). Stress and coping is embedded within a relational context and this context is useful in understanding the coping effectiveness of adolescents. Keywords: dyadic coping, diabetes, adolescence, stress and coping, parental involvement Adolescents with chronic illnesses such as Type 1 diabetes experience stressful events surrounding their illness (Beveridge, Berg, Wiebe, & Palmer, 2006; Seiffge-Krenke, 2001) and benefit from parental involvement (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997; Wiebe et al., 2005). Adolescents with diabetes report stressful events such as regulating highs and lows in blood glucose and problems in food intake and exercise (Beveridge et al., 2006). An assumption is that adolescents’ ability to deal effectively with such stressors is associated with enhanced psychosocial and diabetes adjustment, an assumption that has yet to be rigorously tested in the adolescent literature. Further, dyadic models of coping suggest that perceived coping effectiveness (PCE, evaluation of how well one’s coping strategies deal with the stressful event) is enhanced if (a) adolescents perceive mothers as involved in coping (Berg et al., 2007; Wiebe et al., 2005) and (b) this involvement in coping is consistent with adolescents’ stress appraisals of whether the stressor is something that is the adolescent’s alone or shared with the mother (Berg & Upchurch, 2007). Fathers’ involvement in adolescents’ coping has not yet been thoroughly examined, despite the importance of fathers providing support and monitoring of adolescents’ diabetes (Berg, Butler, et al., 2008; Wysocki & Gavin, 2006). In the present study, we examined whether PCE was enhanced when adolescents’ dyadic coping (e.g., parent is uninvolved or collaborative) was consistent with Cynthia A. Berg, Michelle Skinner, Kelly Ko, Jorie M. Butler, and Jonathan Butner, Department of Psychology, University of Utah; Debra L. Palmer, Department of Psychology, University of Wisconsin–Stevens Point; Deborah J. Wiebe, Department of Psychiatry, University of Texas Southwestern Medical Center. The project was supported by Grant Number R01DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. We thank the families who participated, the staff of the Utah Diabetes Center and Michael Swinyard’s practice, as well as the additional members of the ADAPT team (David Donaldson, Katie Fortenberry, Donna Gelfand, Dwayne Horton, Hai Le, Rob Lindsay, Jenni McCabe, Mary Murray, Peter Osborn, Marejka Shaevitz, Nathan Story, and Mike Swinyward). Portions of this work were presented at the meetings of the American Psychological Association, August, 2007. Address correspondence to Cynthia A. Berg, 380 S. 1530 E., Department of Psychology, University of Utah, Salt Lake City, UT 84112. E-mail: cynthia.berg@psych.utah.edu 521 522 BERG ET AL. their stress appraisals (e.g., stressor is mine or shared with the parent), comparing the involvement of mothers and fathers. Although the association between PCE and psychosocial adaptation has been examined in the adult literature, the child and adolescent literature largely excludes the measurement of perceived coping effectiveness (Grant et al., 2006), defining effectiveness as psychosocial adjustment. When adults cope with stress, PCE is associated with better psychological well-being (McCrae & Costa, 1986), lower stress reactivity (Brauer, 2001), and use of active coping strategies in health stressors (Zautra & Wrabetz, 1991). Perceived coping effectiveness may be particularly important for older adolescents, as they expand and build effective coping repertoires (Brotman-Band & Weisz, 1988; Grant et al., 2006), face new stressors, and employ more independent coping strategies (Rudolph, Dennig, & Weisz, 1995). For example, PCE may be associated with better psychosocial adjustment (e.g., lower depressive symptoms) as well as diabetes management (better adherence, self-efficacy for diabetes management, and metabolic control) in adolescence (Band & Weisz, 1990). The ability to deal effectively with stressful life events surrounding chronic illness may be enhanced when close relationship partners are viewed as actively engaged in coping, consistent with recent dyadic approaches to stress and coping (Berg & Upchurch, 2007; Revenson, Kayser, & Bodenman, 2005). In adolescents coping with diabetes, collaborative coping (where adolescents and mothers pool resources and jointly problem solve together) has been associated with fewer depressive symptoms (Berg et al., 2007), better glucose control, and adherence (Wiebe et al., 2005), greater parental involvement (Wiebe et al., 2005) and greater parental acceptance (Berg, Schindler, & Maharajh, 2008). In married couples, collaborative coping has been associated with better coping effectiveness (Berg, Wiebe et al., 2008) and higher global self-efficacy (Coyne & Smith, 1991; Kuijer et al., 2000). However, not all research indicates that collaborative coping is associated with better psychosocial adjustment. For instance, wives whose husbands were recovering from a myocardial infarction reported greater distress with more active engagement with husbands (Coyne & Smith, 1991). The lack of benefit to active engagement may have occurred because of a mismatch between dyadic coping and stress appraisal (Manne & Zautra, 1989). Dyadic coping may be associated with PCE to the extent that it fits with how the stressful event is appraised in relation to others (Berg & Upchurch, 2007; Lyons et al., 1995). Stress appraisal in the present study refers to how individuals appraise the ownership of the stressful event (e.g., mine, shared with others). Initial work on dyadic coping viewed stressors as potentially appraised as the person’s alone (e.g., the adolescent’s stressor) as well as the property of a dyadic unit (the adolescent’s and the mother’s shared stressor) (Acitelli & Badr, 2005; Lyons et al., 1995). Families frequently appraise Type 1 diabetes as shared within the family rather than as the adolescent’s issue alone (Beveridge et al., 2006; Hauser et al., 1993). Berg and Upchurch (2007) posit that dyadic coping will be more frequent when stressors are appraised as shared versus appraised as the adolescent’s alone. Further, PCE may be best when collaborative coping occurs together with one’s own appraisal of the stressor as shared and less effective when one appraises the stressor as his or hers alone. The importance of the fit between stress appraisal and dyadic coping for PCE could differ for adolescents’ perceptions of mothers’ and fathers’ involvement. Little research has focused on fathers’ involvement in the coping efforts of their children (Kliewer, Fearnow, & Miller, 1996; SeiffgeKrenke, 2002). However, fathers play an important role in their children’s lives in general (Bumpus et al., 2006) and in the context of chronic disease, especially during adolescence (Berg, Butler, et al., 2008; Laffel et al., 2003; Palmer et al., 2009; Wysocki & Gavin, 2006). Adolescents may perceive mothers to be more involved in their coping efforts than fathers as mothers are more likely to participate in everyday caregiving behaviors (Phares, Lopez, Fields, Kamboukos, & Duhig, 2005). Thus, we compared adolescents’ perceptions of the involvement of mothers and fathers in coping. The goal of the study was to explore whether PCE was associated with better diabetes adjustment and whether PCE was enhanced when adolescents’ dyadic coping was fit to stress appraisal. Adolescents described the two most stressful events of the week dealing with their diabetes, and three coping strategies they used to deal with each event. They then appraised the dyadic nature of each coping strategy (parent uninvolved, supportive, collaborative, or controlling), and stress appraisal (mine, indirectly or directly shared with parent), and how well they handled each event (PCE). First, we established that PCE was associated with multiple indicators of adjustment to diabetes (i.e., self care behaviors, depressive symptoms, self-efficacy, metabolic control). Second, we examined the link between stress appraisal and dyadic coping. We hypothesized that collaborative coping would occur more frequently in the context of shared stress appraisal. Third, we examined whether a greater link between shared stress appraisal and collaborative coping was associated with greater perceived efficacy in dealing with the stressful event. Method Participants Participants included 252 adolescents (M age ⫽ 12.49 years, SD ⫽ 1.53, 53.6% females) diagnosed with Type 1 diabetes mellitus, their mothers (M age ⫽ 39.64 years, SD ⫽ 6.34) and 188 fathers (M age ⫽ 42.08 years, SD ⫽ 6.32) recruited from a university/private partnership clinic (76%) and a community-based private practice (24%), that followed similar treatment regimens and clinic procedures. Eligibility criteria included that adolescents were between 10 and 14 years of age, had diabetes more than 1 year (M ⫽ 4.13 years, SD ⫽ 3), and were able to read and write either English or Spanish. For each adolescent, one mother and one father were eligible to participate (74% of fathers par- STRESS APPRAISAL AND DYADIC COPING ticipated). Adolescents were required to be living with their participating mother, to facilitate modeling changes in mother-child relationships over time in the larger project. Step-mothers or adoptive mothers (3.2%) were eligible if they had lived with the adolescent for at least 1 year. If both a biological father and a step- or adoptive father were eligible, we recruited the father that adolescents reported was most involved in their diabetes management. Most (74.6%) participating fathers were biological, with the remainder being step-fathers or adoptive fathers. Approximately half (50.8%) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI). Mothers of adolescents on MDI reported physicians recommended an average of 4.14 insulin injections (SD ⫽ 1.81, range: 0-10) and 5.53 blood glucose checks per day (SD ⫽ 1.70, range: 1-11). Of the qualifying individuals approached, 66% agreed to participate in the study, the first wave of a 3-year longitudinal study (see Berg, Butler, et al., 2008 for further details concerning sample selection). Families were largely White (94%) and middle class: most (73%) reported household incomes averaging $50,000 or more annually, 51% of mothers and 58% of fathers reported education levels of 2 years of college or beyond, and an average Hollingshead index (1975) value of 42.04 indicating a medium business, minor professional, technical status. Procedure The study was approved by the appropriate Institutional Review Board, with parents providing informed consent and adolescents providing written assent. During recruitment at their diabetes clinics, participants were scheduled for a laboratory appointment and received questionnaires to be completed individually before their appointment. In the laboratory, adolescents completed questionnaires that were time-sensitive (e.g., CDI) and participated in a digitally recorded interview regarding stress and coping. The measures reported here contain only a subset of those included in the larger study (e.g., parental well-being, parental involvement) and there is no overlap between the results reported in this study and other papers from this larger study (Berg, Butler et al., 2008; Palmer et al., 2009). Measures Stress and coping interview. The stress and coping interview was a structured interview designed to elicit two detailed descriptions of adolescents’ diabetes stressful events that happened in the last week and stress appraisals and dyadic coping. Consistent with our previous protocol (Berg et al., 2007; Wiebe et al., 2005), adolescents were first asked to report one thing that they did each day to remind them of the past week’s events. They then reported the two most stressful events of the past week regarding their diabetes. If adolescents could not think of a stressful event dealing with diabetes, they were prompted with examples concerning problems that a friend with asthma experienced; if they still could not think of a diabetes event, they de- 523 scribed the most stressful event of the week. Adolescents overwhelmingly described diabetes stressors (96.2% of adolescents’ first stressors, 89.3% of the second). We included all stressors in the analyses as the analyses reported below were unchanged when the results were restricted to only diabetes stressors. These stressors were similar to our past work with adolescents in the same age group (Beveridge et al., 2006) and included problems with metabolic control, food management, exercise management, testing, forgetting diabetes supplies, and management away from home. Adolescents were then asked to describe three coping strategies (thoughts, actions, feelings) they used to manage or cope with each stressful event. For adolescents who did not spontaneously mention three strategies, they were prompted twice with “what else did you do, think or feel.” If they had difficult thinking of a strategy they were prompted with examples of strategies that a person with asthma might use to deal with a stressful event (85.5% of adolescents mentioned three strategies for the first stressful event and 78.3% for the second stressful event). These coping responses included a range of actions (e.g., took insulin, gave a shot, called mom), thoughts (e.g., went over what I’m supposed to do in my head), and emotions (e.g., tell myself to calm down). This process was repeated for the second stressor. Dyadic stress appraisal. Following adolescents’ descriptions of stressful events and coping strategies, they were asked to appraise each event in relation to their mother and then to their father. They were asked to first think about how their mother was involved in each of the two stressful events, choosing one of the following phrases to describe each event: (a) stress is mine (my mother does not think about the stress and isn’t affected by it) indicating individual appraisal, (b) My stress affects my mother (it is my stress but I know that it affects my mother) indicating indirectly shared appraisal, or (c) stress is ours (it is something that is shared with my mother) indicating directly shared appraisal. Dyadic coping. For each coping strategy that adolescents described as using to deal with the stressor, adolescents were given four categories and then asked to categorize their mothers’ and then their fathers’ involvement as uninvolved (I worked alone), supportive (mother/ father provided emotional support, encouraged, changed plans on account of me), collaborative/worked together (mother/father and I worked together), or controlling (my mother/father told me what to do). Proportions of uninvolved, supportive, collaborative, and controlling coping were calculated across the three strategies adolescents mentioned for each stressful event. For example, if an adolescent reported that mother was collaborative for all coping strategies, he or she received a score of 1 for collaborative/worked together and a score of 0 for supportive or uninvolved. Perceived coping effectiveness. After describing each stressful event, adolescents rated one item asking how well they handled the event (1 ⫽ very badly to 5 ⫽ very good). 524 BERG ET AL. Indices of Adjustment to Diabetes Depressive symptoms. The Children’s Depression Inventory (Kovacs, 1985) indicated the extent to which the child experienced depressive symptoms in the past 2 weeks. This 27-item scale has high internal consistency and testretest reliability and is sensitive to difficulties in managing diabetes (e.g., Grey et al., 2001). Reliability in the present study was excellent (␣ ⫽.84). Self report of self-care behaviors. Adolescents individually completed a 16-item Self Care Inventory (adapted from La Greca et al., 1990) to assess adherence to the diabetes regimen over the preceding month. The scale was adapted to reflect current diabetes regimens (e.g., calculating insulin doses based on carbohydrate content of meals or snacks) by a certified diabetes educator. Reliability in the present study was excellent (␣ ⫽.85). Self-efficacy. The Self-Efficacy for Diabetes Management Scale (Iannotti et al., 2006) was used as convergent validation for the measure of PCE. It assesses the adolescent’s confidence in being able to manage diabetes across ten problematic situations. Items were rated from 1 ⫽ not at all sure to 10 ⫽ completely sure and averaged (␣ ⫽.81). Metabolic control. Children’s glycosylated hemoglobin (HbA1c) levels were obtained from clinic visits. HbA1c represents average blood glucose levels over the preceding three months (higher indicates poorer metabolic control) and was obtained using the Bayer DCA2000. Results Descriptive Statistics Adolescents categorized mothers most frequently as sharing their stressful event (40.4% and 32.6% for first and second stressful event, respectively), followed by mine (31.4% and 40.8%), and then indirectly sharing (28.2% and 26.6%). In contrast, adolescents appraised their stressor in relation to their father to be largely “mine” (53.3% and 61.4%), followed by indirectly shared (28.6% and 22.3%) and finally shared (18.1% and 16.3%). Adolescents perceived their mothers were most likely uninvolved, followed by collaborative and then supportive in their coping efforts. Similarly, adolescents perceived their fathers as most likely uninvolved, followed by collaborative and supportive. Strategies were infrequently categorized as controlling (3% for mother’s involvement and 1% for fathers’ involvement) and thus were not analyzed further. To analyze parent differences in dyadic coping, three repeated measures ANOVAs (one for each coping category) were conducted with parent (mother, father) and stressor number (first vs. second) as within subject variables. Significant parent differences were found for all coping categorizations: uninvolved F(1, 214) ⫽ 122.0, p ⬍ .01, collaborative F(1, 214) ⫽ 19.2, p ⬍ .01, and supportive coping F(1, 214) ⫽ 69.7, p ⬍ .01. As can be seen in Table 1 (containing means and standard deviations of variables), adolescents appraised mothers to be less uninvolved, more collaborative, and more supportive than fathers in their coping. Intercorrelations of the same Table 1 Means and SDs of Study Variables Study variable Mean SD Mother collaboration Stressor 1 Mother collaboration Stressor 2 Mother support Stressor 1 Mother support Stressor 2 Mother uninvolved Stressor 1 Mother uninvolved Stressor 2 Father collaboration Stressor 1 Father collaboration Stressor 2 Father support Stressor 1 Father support Stressor 2 Father uninvolved Stressor 1 Father uninvolved Stressor 2 PCE Stressor 1 PCE Stressor 2 CDI Self-care Self-efficacy HbA1c .36 .28 .22 .17 .38 .52 .25 .22 .09 .08 .65 .68 3.8 3.7 5.4 3.9 6.7 8.4 .29 .30 .28 .29 .36 .38 .29 .29 .20 .19 .37 .36 .80 .84 5.2 .58 1.7 1.6 dyadic coping categories across the two stressful events (e.g., collaboration on Stressor 1 with collaboration on Stressor 2) revealed quite low correlations (range: .10, p ⬎ .05 to .33, p ⬍ .05 for mothers, .30 to .53, for fathers all ps ⬍ .05). PCE and Diabetes Outcomes To examine whether PCE was associated with adjustment, a series of multiple regressions was conducted with PCE, age of adolescent, and the interaction of PCE by age as independent variables (each effect was first centered at its mean and then interactions calculated; Aiken & West, 1991), and adherence, depressive symptoms, self-efficacy, and HbA1c as dependent variables. Given correlations between PCE on Stressor 1 and Stressor 2 (r ⫽ .37, p ⬍ .01), these two measures were combined for the analyses below. The results remain the same when analyzed separately by event. Higher PCE was associated with higher adherence F(229) ⫽ 7.8,  ⫽ .23, p ⬍ .01, R2 ⫽ .09, lower depressive symptoms F(229) ⫽ 15.1,  ⫽ ⫺.34, p ⬍ .01, R2 ⫽.12 and higher self-efficacy, F(227) ⫽ 10.2,  ⫽ .23, p ⬍ .01, R2 ⫽ .08. No interactions were found between PCE and age for these variables (p ⬎ .05). Finally, better metabolic control (lower HbA1c) occurred for adolescents with higher PCE, F(229) ⫽ 7.0,  ⫽ ⫺.20, p ⬍ .01, R2 ⫽ .07, but this was modified by an interaction between PCE and age ( ⫽ ⫺.14, p ⬍ .01, R2 change ⫽ .02). PCE was associated with lower HbA1c, but this association was stronger among older versus younger adolescents. These analyses support our hypothesis that PCE would be associated with better diabetes adjustment. Relation Between Stress Appraisal and Dyadic Coping To address whether stress appraisal was associated with dyadic coping, ANOVAs were conducted separately for STRESS APPRAISAL AND DYADIC COPING Stressor 1 and 2, with stress appraisal as the independent variable and the proportion of each dyadic coping measure as the dependent variable (see Table 2). We used separate ANOVAs to facilitate comparisons across stressor appraisal, rather than calculating multiple dummy codes and analyzing both stressors with repeated measures regression. These analyses indicated that when adolescents viewed stressors as their own, they viewed both mothers and fathers as more uninvolved for each stressor. In contrast, when adolescents viewed the stressor as either indirectly or directly shared, they were more likely to see their mothers and fathers as involved via supportive and collaborative coping. In 10 of the 12 cases, the difference between indirect and shared appraisals was not significant using Scheffe post-hoc comparisons. Thus, all further analyses were collapsed across indirect and shared. These analyses confirm that there is a link between stress appraisal and dyadic coping. Fit Between Stress Appraisal and Dyadic Coping Predicting PCE The third aim examined whether PCE was higher when there was a greater fit between stress appraisal and dyadic coping; that is, whether stress appraisal interacted with dyadic coping to predict PCE. Because stressors were nested within individuals, and adolescent appraisals of mother and father were nested within family, we used multivariate hierarchical linear models with application to matched pairs (HMLM2; Raudenbush, Bryk, Cheong, & Congdon, 2000). This procedure simultaneously estimated models for adolescents’ appraisals of mothers and fathers, and allowed us to test for differences in regression weights across parent (see also Berg et al., 2008). Using collaboration as an example, the independent variables were stress appraisal for each stressor and the proportion of coping 525 strategies appraised as collaborative, and the interaction of stressor appraisal and collaborative coping. Similar models were analyzed with uninvolved and supportive coping as independent variables. Stress appraisal was dummy coded (1 ⫽ shared or indirect, ⫺1 ⫽ mine) and the proportion of coping strategies (collaborative, uninvolved, or supportive) were centered around their mean to create interaction terms (Aiken & West, 1991). Models were initially conducted to test whether the stressor appraisal ⫻ coping interaction was modified by age or gender; no significant effects were found, so we present the reduced model. In addition, length of diagnosis was used as a covariate in all models, but was not included in the final models because it did not alter the results. The model using collaborative coping revealed that there was a significant interaction between stressor appraisal and proportion of collaborative coping for Stressor 1, but the effect was not significant for Stressor 2 (see Table 3). A test of whether the interaction effect was different across Stressor 1 and Stressor 2 revealed no significant differences, 2(1) ⫽ 2.56, p ⬎ .10. Because this test was not significant, we conducted a pooled test of the coefficient across stressors, which was significant, 2(1) ⫽ 4.36, p ⬍ .05. As can be seen in Figure 1, greater use of collaborative coping was only associated with greater PCE when adolescents perceived that the stressor was indirectly or directly shared with their mother. When the stressor was appraised as individual, greater use of collaborative coping was associated with poorer PCE. A similar model was used to analyze the proportion of uninvolved coping. A significant interaction between stressor appraisal and uninvolved coping occurred only for Stressor 1, but the interaction was not significantly different across Stressors 1 and 2, 2(1) ⫽ 1.68, p ⬎ .10. The pooled Table 2 ANOVAs of Stress Appraisal Predicting Strategy Categorizations Mine Stress appraisal Teen’s perceptions of mother Stressor 1 1. Uninvolved 2. Collaborative 3. Supportive Stressor 2 1. Uninvolved 2. Collaborative 3. Supportive Teen’s perceptions of father Stressor 1 1. Uninvolved 2. Collaborative 3. Supportive Stressor 2: Stressor categorizations 1. Uninvolved 2. Collaborative 3. Supportive Indirect Shared Mean SE Mean SE Mean SE F df .61a .27a .11a .04 .03 .03 .32b .42b .22a,b .04 .03 .03 .25b .38b .31b .03 .03 .03 28.58ⴱⴱ 5.97ⴱⴱ 11.49ⴱⴱ 2, 241 2, 241 2, 241 .74a .18a .07a .03 .03 .03 .45b .40b .15a .04 .04 .03 .30c .33b .33b .04 .03 .03 40.97ⴱⴱ 12.5ⴱⴱ 22.19ⴱⴱ 2, 230 2, 233 2, 230 .84a .13a .03a .03 .03 .02 .49b .39b .12b .04 .03 .03 .38b .39b .22b .03 .04 .03 45.5ⴱⴱ 26.66ⴱⴱ 15.92ⴱⴱ 2, 223 2, 223 2, 223 .81a .15a .02a .03 .03 .01 .51b .37b .12b .05 .04 .03 .40b .31b .25c .05 .05 .03 32.3ⴱⴱ 12.93ⴱⴱ 24.68ⴱⴱ 2, 212 2, 212 2, 212 Note. Means sharing same subscripts were not significantly different from one another. ⴱⴱ p ⬍ .01. 526 BERG ET AL. Table 3 HMLM Coefficients for Models Examining Fit of Stressor Appraisal and Dyadic Coping-Adolescents’ Appraisals of Mothers’ Involvement Perceived coping effectiveness I. Collaborative strategies Intercept Stressor appraisal (SA) Collaborative strategies (CS) SA ⫻ CS II. Uninvolved strategies Intercept Stressor appraisal (SA) Uninvolved strategies (US) SA ⫻ US III. Supportive strategies Intercept Stressor appraisal (SA) Supportive strategies (SS) SA ⫻ SS ⴱⴱ Stressor 1 Stressor 2 Coeff SE Coeff SE 3.64ⴱⴱ .01 ⫺.01 .15ⴱⴱ .06 .05 .05 .05 3.68ⴱⴱ ⫺.03 .09 .02 .06 .06 .06 .06 3.60ⴱⴱ .03 .03 ⫺.15ⴱⴱ .06 .06 .05 .05 3.66ⴱⴱ ⫺.04 ⫺.09 ⫺.05 .07 .06 .06 .06 3.63ⴱⴱ .01 ⫺.07 .07 .06 .06 .06 .06 3.68 ⫺.03 .08 ⫺.03 .06 .05 .06 .06 p ⬍ .01. test of the coefficient across stressors was statistically significant, 2(1) ⫽ 6.03, p ⬍ .05. Greater use of uninvolved coping was associated with greater PCE when adolescents perceived that the stressor was theirs alone (Figure 2). However, when the stressor was viewed as shared, greater use of uninvolved coping was associated with poorer PCE. Analyses conducted on supportive coping yielded no significant interactions (ps ⬎ .05). A similar set of analyses was conducted for teen’s appraisals of father’s involvement. In analyses for collaborative, uninvolved and supportive coping, no significant interaction was found between stressor appraisal and strategy categorizations (p ⬎ .05). Discussion PCE in managing diabetes stressors was associated with depressive symptoms, self-efficacy for diabetes management, adherence, and metabolic control. Consistent with the Developmental Contextual Model (Berg & Upchurch, 2007), dyadic coping was more frequent in stressors viewed as shared. Further, results indicated that PCE was higher when dyadic coping with mothers was consistent with adolescents’ appraisals of stressful situations. Our results point towards the importance of examining adolescents’ appraisals of stressors, especially appraisals of how parents are involved in coping. PCE and Adjustment The results demonstrate the value of measuring appraisals in addition to global adjustment. Adolescents’ appraisals of 3.9 3.8 Perceived Coping Effectiveness 3.7 3.6 Mine Shared (Directly or Indirectly) 3.5 3.4 3.3 3.2 3.1 Low Collab High Collab Adolescents' Categorization of Mothers' Involvement Figure 1. Perceived coping effectiveness as a function of adolescents’ stress appraisal and collaborative coping with mothers. STRESS APPRAISAL AND DYADIC COPING 527 3.8 Perceived Coping Effectiveness 3.7 3.6 3.5 Mine Shared (Directly or Indirectly) 3.4 3.3 3.2 3.1 Involved Uninvolved Adolescents' Categorization of Mothers' Involvement Figure 2. Perceived coping effectiveness as a function of adolescents’ stress appraisal and uninvolved coping with mothers. higher PCE were associated with lower depressive symptoms, higher self-efficacy for diabetes management, better HbA1c, and better adherence. These findings lend support to the assumption in the literature that when adolescents effectively deal with specific stressful events, they experience better overall adjustment. The link between PCE and adjustment is consistent with the adult literature (Brauer, 2001; McCrae, & Costa, 1986; Zautra, Hamilton, & Yocum, 2000; Zautra & Wrabetz, 1991). Additionally, our study is consistent with the work of Band and Weisz (1990) that coping effectiveness is associated with better diabetesrelated outcomes. PCE was associated with adjustment similarly across age, with the exception of its associations with metabolic control. That is, although perceived coping effectiveness was associated with better metabolic control, this association was stronger for older adolescents. It is possible that older adolescents’ ability to cope effectively with diabetes stressors (many of which include regulating blood glucose) may have a direct physiological pathway to metabolic control. Alternatively, older adolescents may use HbA1c as a gauge for how well they are coping with daily stressors more so than younger adolescents. Our results do not point to overarching age differences in appraisals, in contrast to the literature indicating marked age increases in cognitive or emotion-focused coping strategies (Compas et al., 2001). Age differences may appear in a slightly older sample of adolescents, an issue that will be addressed in our longitudinal work with this sample. One limitation of the present study was its somewhat restricted age range. Stress Appraisal and Dyadic Coping and PCE Conceptualizations of dyadic coping across the life-span suggest that in addition to examining others’ involvement in coping, others may also be involved in how stressors are appraised (Berg & Upchurch, 2007). To our knowledge, our results are the first to demonstrate a link between stress appraisal and dyadic coping. For adolescents’ perceptions of both mothers and fathers, perceptions that parents shared their stressor were associated with greater collaborative and supportive involvement, and lower uninvolvement, in the strategies they used to cope with the stressful event. Although stress appraisals were linked to dyadic coping, stress appraisal and coping were not synonymous. Our results indicating the modest association between dyadic coping categories across the two stressful events suggests that dyadic coping occurs in response to specific contextual conditions and less a function of person characteristics. Results further indicate that PCE is associated with the appraisal of the stressful event, and that congruence between stress appraisals of stress and dyadic coping is associated with higher PCE (Berg & Upchurch, 2007; Lyons et al., 1995). We did not see simple associations between collaborative, supportive, or uninvolved coping predicting effectiveness. Past work would indicate that perceptions of collaborative coping are associated with positive adjustment in adolescents with diabetes (Berg et al., 2007; Wiebe et al., 2005) and PCE in patients coping with prostate cancer (Berg, Wiebe et al., 2008). It is 528 BERG ET AL. possible that cohort differences between our previous work and the present work may explain why we did not see this anticipated finding. A potential cohort factor could be rapidly changing medical technologies now available for insulin delivery (e.g., the increasing number of adolescents who manage their diabetes using an insulin pump), which may alter the role of parental involvement in adolescent diabetes management (Streisand, Swift, & Wickmark, 2005). When stressful events were viewed as shared with the mother, the presence of collaborative coping was associated with better PCE, whereas the presence of uninvolved coping was associated with lower PCE. Thus, stress appraisal may provide an important context for understanding the benefits of dyadic coping. Our results suggest that collaborative coping is not perceived as effective when adolescents appraise the stressful event as their own, potentially because such involvement may be perceived as intrusive and overprotective (Holmbeck et al., 2002). The lack of results for supportive coping here may be because of its lower frequency, especially when adolescents appraised their stressors as individual. The present results here on dyadic stress appraisal and coping extends research (Park, Armeli, & Tennen, 2004) on “goodness of fit” that typically assesses the fit between appraisals of controllability and type of strategy (i.e., primary versus secondary control; Lazarus & Folkman, 1984) to include the fit between stressor ownership and dyadic coping. Our results indicate that the associations of the fit between stress appraisal and coping and PCE is only applicable for mothers, but not fathers. Appraisals of mothers’ and fathers’ involvement in both stress appraisal and dyadic coping revealed several differences. Consistent with the view of mothers as the primary caregiver in assisting children with practical and instrumental tasks (Phares et al., 2005), mothers were viewed as far more involved both in how the adolescent appraised stressful events and dyadic coping. Fathers were perceived to be predominantly uninvolved in adolescents’ coping. Fathers may play more of a distant role rather than being active in managing adolescents’ daily stressors (Faulkner, 1996), which may explain their lower influence in adolescents’ coping (Kliewer et al., 1996). Fathers’ greater uninvolvement in stress appraisal and coping may have led to the lack of interactions between adolescents’ appraisals and dyadic coping predicting PCE. The results should be considered in the context of some limitations. First, individuals were only asked about the two most stressful events of the week. Our work with married couples (Berg, Wiebe et al., 2008) suggests that greater sampling of stressful events across the daily lives of families may be beneficial in understanding appraisal and dyadic coping processes. Further, adolescents were the sole source of data and the results could be due, in part, to shared method variance. Further work with the present sample includes daily diary analyses of adolescents, mothers, and fathers, and will allow us to examine daily processes across reporters. Second, reports of stressful events were retrospective in nature and the amount of time between recall and the experience of the stressful event may have influenced both how parental involvement and PCE was perceived. Thus, we cannot interpret our results as indicating causal relationships. An alternative direction of causality is also plausible. For instance, adolescents who have greater PCE may invite parents into their stress and coping efforts, and perceive greater shared ownership and collaborative coping. Third, our conceptualization of dyadic coping was based on a categorical view of parental involvement; future work is needed to compare our categorical interview methods with more typical continuous rating scales. In addition, our categorization of dyadic coping is only one way in which to categorize coping and comparisons of our categorization to more typical stressors categories (e.g., problem-focused vs. emotion-focused or adaptive vs. not adaptive) would be fruitful. Fourth, participants were almost exclusively White with above average levels of socioeconomic status making it difficult to generalize findings to the general population. In general, the results indicate that stress and coping is embedded within the dyadic coping context. As adolescents manage stressors surrounding chronic illness, appraisal processes concerning the shared nature of stressors may provide a context for how effective dyadic coping will be. As in the adult literature, interventions that promote coping effectiveness may be a fruitful avenue for enhancing adolescents’ feelings of competence to manage illness-related stressors. Further, including parents, especially mothers, in these efforts may enhance both psychosocial and diabetesspecific adjustment by encouraging adaptive involvement (e.g. matching adolescents’ perceptions with parental involvement in coping). References Acitelli, L. K., & Badr, H. (2005). My illness or our illness? Attending to the relationship when one partner is ill. In T. A. Revenson, K. Kayser, & G. Bodenmann (Eds.), Emerging perspectives on couples’ coping with stress (pp. 121–136). Washington, DC: American Psychological Association. Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications. Anderson, B. J., Ho, J., Brackett, J., Finkelstein, D., & Laffel, L. (1997). Parental involvement in diabetes management tasks: Relationships to blood-glucose monitoring, adherence, and metabolic control in young adolescents with IDDM. Journal of Pediatrics, 130, 257–265. Band, E., & Weisz, J. R. (1990). Developmental differences in primary and secondary control coping and adjustment to juvenile diabetes. Journal of Clinical and Child Psychology, 19, 150 – 158. Berg, C. A., Butler, J., Osborn, P., King, G., Palmer, D., Butner, J., et al. (2008). The role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678 – 683. Berg, C. A., Schindler, I., & Marajh, S. (2008). Adolescents’ and Mothers’ Perceptions of the Cognitive and Relational Functions of Collaboration and Adjustment in Dealing with Type 1 Diabetes. Journal of Family Psychology, 22, 865– 874. STRESS APPRAISAL AND DYADIC COPING Berg, C. A., & Upchurch, R. (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133, 920 –954. Berg, C. A., Wiebe, D. J., Beveridge, R. M., Palmer, D. L., Korbel, C. D., Upchurch, R., et al. (2007). Mother-child appraised involvement in coping with diabetes stressors and emotional adjustment. Journal of Pediatric Psychology, 32, 995–1005. Berg, C. A., Wiebe, D. J., Bloor, L., Butner, J., Bradstreet, C., Upchurch, R., et al. (2008). Collaborative coping and daily mood in couples dealing with prostate cancer. Psychology and Aging, 23, 505–516. Beveridge, R. M., Berg, C. A., Wiebe, D. J., & Palmer, D. L. (2006). Mother and adolescent representations of illness ownership and stressful events surrounding diabetes. Journal of Pediatrics Psychology, 31, 818 – 827. Brauer, D. J. (2001). Common patterns of person-environment interaction in persons with rheumatoid arthritis. Western Journal of Nursing Research, 23, 414 – 430. Brotman-Band, E. B., & Weisz, J. R. (1988). How to feel better when it feels bad: Children’s perspectives on coping with everyday stress. Developmental Psychology, 24, 247–253. Bumpus, M. F., Crouter, A. C., & McHale, S. M. (2006). Linkages between negative work-to-family spillover and mothers’ and fathers’ knowledge of their young adolescents’ daily lives. Journal of Early Adolescence, 26, 36 –59. Compas, B., Connor-Smith, J., Saltzman, H., Thomsen, A., & Wadsworth, M. (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127, 87–127. Coyne, J. C., & Smith, D. A. F. (1991). Couples coping with a myocardial infarction: A contextual perspective on wives’ distress. Journal of Personality and Social Psychology, 61, 404 – 412. Faulkner, M. S. (1996). Family responses to children with diabetes and their influence on self-care. Journal of Pediatric Nursing, 11, 82–93. Grant, K. E., Compas, B. E., Thurm, A. E., McMahon, S. D., Gipson, P. Y., Campbell, A. J., et al. (2006). Coping with stress during childhood and adolescence: Problems, Progress, and Potential theory and research. Clinical Psychology Review, 26, 257–283. Grey, M., Davidson, M., Boland, E. A., & Tamborlane, W. V. (2001). Clinical and psychosocial factors associated with achievement of treatment goals in adolescents with diabetes mellitus. Journal of Adolescent Health, 28, 377–385. Hauser, S., DiPlacido, J., Jacobson, A., & Willett, J. (1993). Family coping with an adolescent’s chronic illness: An approach and three studies. Journal of Adolescence, 16, 305–329. Holmbeck, G. N., Johnson, S. Z., Wills, K. E., McKernon, W., Rose, B., Erklin, S., et al. (2002). Observed and perceived parental overprotection in relation to psychosocial adjustment in preadolescents with a physical disability: The mediational role of behavioral autonomy. Journal of Consulting and Clinical Psychology, 70, 96 –110. Iannotti, R. J., Schneider, S., Nansel, T. R., Haynie, D. L., Plotnick, L. P., Clark, L. M., et al. (2006). Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics, 27, 98 –105. Kliewer, W., Fearnow, M. D., & Miller, P. A. (1996). Coping socialization in middle childhood: Tests of maternal and paternal influences. Child Development, 67, 2359 –2357. 529 Kovacs, M. (1985). The children’s depression inventory (CDI). Psychopharmacology Bulletin, 21, 995–998. Kuijer, R. G., Ybema, J. F., Buunk, B. P., de Jong, G. M., Thijs-Boer, F., & Sanderman, R. (2000). Active engagement, protective buffering, and overprotection: Three ways of giving support by intimate partners of patients with cancer. Journal of Social and Clinical Psychology, 19, 256 –275. Laffel, L. M., Connell, A., Vangsness, L., Goebel-Fabbri, A., Mansfield, A., & Anderson, B. J. (2003). General quality of life in youth with type 1 diabetes: Relationship to patient management and diabetes-specific family conflict. Diabetes Care, 26, 3067–3073. La Greca, A. M., Follansbee, D., & Skyler, J. S. (1990). Learned helplessness in diabetic youths. Journal of Pediatric Psychology, 15, 581–594. Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer Publishing Company. Lyons, R., Sullivan, M., Ritvo, P., & Coyne, J. (1995). Relationships in chronic illness and disability. Thousand Oaks, CA: Sage. Manne, S. L., & Zautra, A. J. (1989). Spouse criticism and support: Their association with coping and psychological adjustment among women with rheumatoid arthritis. Journal of Personality and Social Psychology, 56, 608 – 617. McCrae, R. R., & Costa, P. T. (1986). Personality, coping, and coping effectiveness in an adult sample. Journal of Personality, 54, 385– 405. Palmer, D. L., Berg, C. A., Butler, J., Fortenberry, K., Murray, M., Lindsay, R., et al. (2009). Mothers’, fathers’, and children’s perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology, 34, 194 –204. Park, C. L., Armeli, S., & Tennen, H. (2004). Appraisal-Coping goodness of fit: A daily internet study. Personality and Social Psychology Bulletin, 30, 558 –569. Phares, V., Lopez, E., Fields, S., Kamboukos, D., & Duhig, A. M. (2005). Are fathers involved in pediatric psychology research and treatment? Journal of Pediatric Psychology, 30, 631– 643. Raudenbush, S. W., Bryk, A., Cheong, Y. F., & Congdon, R. (2000). HLM 5: Hierarchical linear and nonlinear modeling. Chicago: Scientific Software International. Revenson, T., Kayser, K., & Bodenmann, G. (2005). Couples coping with stress: Emerging perspectives on dyadic coping. Washington, DC: American Psychological Association. Rudolph, K. D., Dennig, M. D., & Weisz, J. R. (1995). Determinants and consequences of children’s coping in the medical setting: Conceptualization, review, and critique. Psychological Bulletin, 118, 328 –357. Seiffge-Krenke, I. (2001). Diabetic adolescents and their families: Stress, coping, and adaptation. New York: Cambridge University Press. Seiffge-Krenke, I. (2002). “Come on, say something, Dad!”: Communication and coping in fathers of diabetic adolescents. Journal of Pediatric Psychology, 27, 439 – 450. Streisand, R., Swift, E., & Wickmark, T. (2005). Pediatric parenting stress among parents of children with type 1 diabetes: The role of self-efficacy, responsibility, and fear. Journal of Pediatric Psychology, 30, 513–521. Wiebe, D. J., Berg, C. A., Palmer, D., Korbel, C., Beveridge, R., Swinyard, M., et al. (2005). Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology, 30, 167–178. 530 BERG ET AL. Wysocki, T., & Gavin, L. (2006). Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology, 31, 501–511. Zautra, A. J., Hamilton, N., & Yocum, D. (2000). Patterns of positive social engagement among women with rheumatoid arthritis. Occupational Therapy Journal of Research, 20, 21S– 40S. Zautra, A. J., & Wrabetz, A. B. (1991). Coping success and its relationship to psychological distress for older adults. Journal of Personality and Social Psychology, 61, 801– 810. Received July 3, 2008 Revision received January 26, 2009 Accepted January 27, 2009 䡲