I ?
advertisement

Applied Research and Analysis Directorate, Health Policy Branch
Direction de la recherche appliquée et de l’analyse, Direction générale de la politique de la santé
IS THE PRICE OF CANCER TREATMENT FALLING?
Alexandra Constant1, Marie-Chantal Benda1, Ruolz Ariste2 and Charles D.
Mallory1
(1) Health Demand and Supply Analysis Division, Applied Research and Analysis
Directorate, Health Policy Branch, Health Canada
(2) Canadian Institute for Health Information
February 13, 2006
Abstract
Rationale: Cancer care represents one of the most costly sectors of medical care. Rapidly
rising costs in medical care put in question the “sustainability” of the publicly funded health
care system. Given rapidly evolving medical technology, it is unclear whether it is higher
prices or greater utilization that contributes more to the increase in health care system costs.
Objectives: The goal of this study is to assess the impact of changing technology for cancer
treatments on health care costs in order to distinguish price changes from quality/quantity
changes.
Methodology: We estimate two types of price indexes: a service price index (SPI) that
reflects the price of particular treatments over time, and a cost-of-living index (COLI)
which measures an outcome-adjusted cost of treating a specific health problem and reflects
price variations by discounting any technological/quality effects. The two indexes are
estimated for the period 1995/96, 2001/02 and 2002/03 by combining data on cancer
patients admitted to hospitals participating in the Ontario Case Costing Initiative (OCCI)
with death data from the Canadian Cancer Registry (CCR).
Results: Hospital cost per patient increased moderately in Ontario for lung, breast, prostate
and colorectal cancer. The SPI rose at an average annual rate of 1.9% between 1995/96 to
2001/02. However, taking into account health outcomes from better health care technology,
it is clear that the price of cancer treatment is falling rapidly. The COLI fell by 2.6%
annually over the period. Although cancer prevalence is increasing, more effective
treatments justify the growth in total costs.
Conclusions: Recognition of the cost drivers in the total medical cost is important, as policy
implications would vary. Given that cost increases are attributable to the wider use of more
effective treatments, there is a net social benefit associated with the expenditure increase.
This study supports the growing international evidence that outcome-adjusted prices of care
for some major diseases are falling.
0
1. INTRODUCTION
Rapidly rising costs in medical care in Canada put in question the “sustainability” of the
publicly funded health care system. Expensive new technologies are one of the factors
identified as contributing to the noticeable increase in health care costs. Technology
affects the medical system in different ways. However, it is unclear whether it is higher
prices or greater utilization of the new technologies that contributes more to the increase
in health system costs. The unit cost of new technologies may be higher or lower than
that of the older technologies; however, they usually bring health improvements, which
are highly valued. As well, new technologies may lead more people to be treated for a
disease. When treatment is effective, giving access to more people is beneficial, but when
it is not effective, it may not be worthwhile. In the context of rapidly rising cost in the
medical sector, the key question addressed in this study is: Are increasing investments in
cancer care worth the cost?
From a global view, health has improved and medical spending has increased. Recent
studies, considering medical technologies at the disease level, show that the estimated
benefits of technological change are greater than or equal to the costs. Using the Cost-ofLiving Index, a quality-adjusted price index based on a cost-benefit analysis, Cutler et al.
(1998) showed that technological change in heart attack care in the US from 1983 to
1994 was easily worth the cost. Similar results are found in Canada by Ariste et al. (2006)
and in Switzerland by Renauld et al. (2004). Cutler and Meara (2000) examined costs and
benefits of new technologies available to treat infants between 1950 and 1990. As with
heart attack, they found a net benefit from new technologies. Berndt et al. (2005)
analysed changes in the treatment of depression in the US over the years 1991 to 1996.
Their results showed that a shift from psychotherapy and tricyclic antidepressants to
selective serotonin reuptake inhibitors (SSRIs, such as Prozac) was accomplished at
virtually no net cost, and patients received more effective doses. Simultaneously,
diagnosis and treatment of depression doubled over the 1990s1, however benefits of
treatment in reduced time spent depressed exceeded the costs without taking into account
1
Statistic from the National Ambulatory Medical Care Survey
1
gains from patients’ being able to work and produce more. Cutler and McClellan (2001)
reported preliminary results of cost-benefit analysis for breast cancer from 1985 to 1996.
In this case, costs and benefits were found to be of about equal magnitude. Detection
technology and public awareness of the benefits of screening have resulted in an
increased detection of breast cancer in the earlier years, which may or may not be
valuable. Breast cancer progresses slowly and most of the time occurs in older women
who may die of other causes before their cancer becomes symptomatic. This may explain
why the benefits are not greater than the costs in breast cancer. The question remains as
to how valuable the treatment is in the marginal patients.
In Canada, cancer represents one of the most costly sectors of medical care and there
have been important advances related to prognosis, diagnosis, treatment and recurrence.
The goal of this study is to assess the impact of changing technology for cancer
treatments on health care costs in order to distinguish pure price changes from
quantity/quality changes. Addressing this issue is complex since price indexes used to
capture the rate of change in prices are not measured accurately, especially price indexes
for medical care services.
Following Cutler and al. (1998), we address this issue by estimating two price indexes.
The first is a service price index (SPI) that reflects the price of particular treatments over
time. The SPI assumes no productivity change in the government sector. Since about
70% of total healthcare expenditure in Canada comes from the public sector, this zero
productivity growth assumption means that quality changes or welfare gains are assumed
away in most healthcare services. In the SPI, all the productivity gains are assumed to be
a pure price movement. Because the SPI does not intrinsically adjust for outcomes, we
use a second index, the Cost-of-Living Index (COLI) or quality-adjusted price index,
which focuses on patient welfare and reflects price variations by discounting any
technological/quality effect. The COLI measures how much a patient would be willing to
pay or would have to be compensated to accept changes in medical treatments and prices
over time in order to keep the same level of utility. From this index, we will see if the
benefits of new cancer technologies are worth the costs. Also, the comparison between
2
the SPI and COLI will provide an estimate of indicate the magnitude of the bias in the
SPI. The policy implications will be different depending on whether the increased
expenditures arises from price changes (this means more and more resources may be
allocated inefficiently to the medical sector) or from changes in utilisation. There could
be net social benefits associated with the total cost increases.
The remainder of the paper is structured as follows. In the next section we discuss the
data sources. In Section 3, we model the aggregate Service Price Index and the Cost-of
Living Index. Section 4 presents summary statistics and Section 5 the results. Section 6
concludes.
2. DATA SOURCES
Three datasets are used in this study. First, we use cross-sectional data from the Ontario
Case Costing Initiative (OCCI) database, which is maintained by the Ontario Ministry of
Health and Long-Term Care. The database contains cost data for 1994/95, 1995/96 and
1998/99 to 2003/04 on acute inpatients, day surgery and ambulatory care patients from
twelve hospitals across Ontario. Information about each patient’s demographic
characteristics (age, sex), administrative characteristics (patient id, admission/discharge
date), clinical characteristics (diagnostic codes, procedures codes), and financial
information (direct and indirect costs) are provided. Costs are assigned by functional
centers, which are divisions/units of a hospital (e.g. pharmacy, ICU, diagnostic imaging).
These costs could include salaries, compensation and benefits, drug prices, leasing costs,
depreciation of equipment used at the functional center, etc. We consider patients whose
main diagnosis is lung, breast, colorectal or prostate cancer, which are the ones with the
highest incidence rate in Canadian population. In 2005, 56% of estimated new cases are
attributable to these four cancers2.
From 1994/95 to 2001/02, diseases are classified according to the 9th international
classification code (ICD-9/CM), and later years are under the newer ICD-10-CA/CCI.
2
Canadian Cancer Society/National Cancer Institute of Canada (2005), Canadian Cancer Statistics
2005, Toronto, Canada, table 1, p.19
3
The classification for cancer disease in ICD-10 is somewhat similar to ICD-9: codes for
malignant neoplasm of lung and breast were subdivided to increased specification on the
site of the neoplasm, while codes for malignant neoplasm of prostate and colorectal
remain unchanged. However, the classification for procedure codes (CCI) is very
different. In order to achieve data comparability, we use the converted diseases codes
ICD-10 to ICD-9 provided by the Canadian Institute for Health Information (CIHI) to
OCCI for the years 2002 and 2003; however results must be interpreted with caution.
The last two sources are from the Canadian Cancer Registry (CCR) and National Cancer
Incidence Reporting System (NCIRS), which are maintained by Statistic Canada. Most of
the data come from provincial and territorial cancer registries. CCR database tracks
patients with tumors diagnosed in more than one province and territory, and its records
are linked to death certificates. The CCR database contains information on both the
individual with the cancer and the characteristics of the cancer from 1992 to 2002, while
NCIRS collected slightly different data from1969 to 1991.
3. MODELLING AGGREGATED SERVICE PRICE INDEX (SPI) AND COST-OF-LIVING
INDEX (COLI)
The SPI is defined as the amount of money necessary to purchase the same basket of
health care services over time. Following Cutler et al. (2001), we form a SPI by taking
into account the vector of all medical treatments available to treat lung, breast, prostate
and colorectal cancer. The Laspeyres SPI is the relative cost of a fixed set of treatments
over time:
SPI
=
p (t1 ) c(t 0 )
*
p (t 0 ) c(t 0 )
= α
p (t1 )
p (t 0 )
(1)
where:
p(t0): the vector of transaction prices for these treatments at the beginning of the period;
p(t1): the vector of transaction prices for these treatments at the end of the period;
c(t0): the vector of all medical care available for these four cancers in the base period;
α : the vector of the share of each treatment in total costs in the base period.
4
Since Canadian hospitals are not-for-profit organizations, we assume that profits are nil.
Therefore, average treatment costs for cancer patients are used as a proxy for average
transaction prices. Keep in mind that OCCI database is used only to calculate in-hospital
costs of cancer treatments. As well, health care providers are frequently paid on the basis
of aggregated bundles of services (for example, capitation in a given Diagnostic Related
Group), given that it is appropriate to price an aggregated set of services.
In order to measure the aggregated SPI, cancer patients are classified into six broad
categories, depending on the major procedure they received3. The first category,
Diagnostic Procedures Only (DP), includes patients who were admitted to the hospital
for only diagnostic procedures, such as diagnostic radiology (X-ray, ultrasound, biopsy,
etc) and exploratory procedures (physical exam, blood test, urine test, etc). The second
category, Diagnostics Procedures and Others (DPO), includes patients whose major
procedure was diagnostic but received subsequent procedures. The third category
includes patients whose major procedure was a Surgical Procedure (SP), which means
any operative procedures such as excision, incision, removal, mastectomy, lobectomy,
etc. Chemotherapy (C), the fourth category, includes injection or infusion of cancer
chemotherapeutic substance, hormone and other therapeutic agent4. The fifth category
includes patients who received Radiotherapy (R) as the major procedure. The last
category, No Procedure (NP), includes patients who were admitted to the hospital but did
not receive any procedure. This case could happen for patients in terminal phase;
pharmacy and social network are examples of functional centers who have reported costs.
Given the OCCI database, we assume that all costs during the stay of a patient are
attributable to the main diagnosis and to the principal procedure reported. This
assumption overstates the cost of the categories.
As already mentioned, the SPI assumed that all the productivity gains are simply pure
price movements. For this reason, we use the COLI, which focuses on patient welfare and
3
Procedures codes are classified according to the International Classification of Diseases 9th revision
Clinical Modification (ICD-9-CM) for all years under study.
5
reflects properly price variations by discounting any technological and quality effect. The
COLI measures how much patients would be willing to pay or would have to be
compensated to accept changes in medical treatments and prices over time.
Following Cutler et al. (1998) the COLI is derived as follows. Consumers have a series of
diseases, indexed by s. If a consumer gets sick, he receives health care cs(t), a vector of
constant quality care. The expected welfare (W) of a representative consumer i in period t
is:
S
Wi (t ) = ∑ π s (t ) * Wi {H i [s, c(t )], Yi − pi (t ).c s (t ) − Ti (t )} ,
(2)
s =1
where πs(t) is the probability that the individual has disease s at time t;
H is the health status of the person. It is a function of the disease and the effects of health
care received;
Yi is the income (assumed to be constant over the time interval);
pi(t) is the vector of prices of health care for the consumer i at time t;
Ti(t) represents lump-sum payments (taxes, insurance premiums) for health care.
Spending in health care is given by the expression (p.c + T), so that the second argument
of the utility function (Y – (p.c + T)) represents consumption of non-health care goods.
This welfare function assumes no changes in disease incidence with time. However, new
diseases may enter the set of possible illnesses and other existing diseases may be
reduced or eliminated due to changes in lifestyles or policy leverage. We circumvent
these effects by estimating price indexes for treating a single disease.
It is
straightforward to apply similar methods to other diseases and then aggregate them to a
medical care price index. Alternately, one can use a sample of diseases. The welfare
function becomes:
W (t ) = W {H [c(t )], Y − p(t ).c(t ) − T (t )}
(3)
4
In ICD9-CM, the procedure classification for chemotherapy is used when the coder lacks the information
necessary to code the term to a more specific category, therefore we might not have captured all
chemotherapy procedure under our fourth category.
6
As in Fisher and Shell [10], we define the cost-of-living (COL) as the amount consumers
would be willing to pay (or would be willing to accept) to have today’s health care and
today’s prices versus base period health care and base period prices. The change in the
COLI between to and t1, denoted (K), is the amount of compensation required to equalize
utility in these two states. It is implicitly defined from:
W {H [c(t1 )], Y − p(t1 ).c(t1 ) − T (t1 ) − K } = W {H [c(t 0 )], Y − p(t 0 ).c(t 0 ) − T (t 0 )}.
(4)
Applying a Taylor’s expansions around t0, and after re-arranging terms, we have:
WH H c
dc − d ( p.c + T ) ,
Wz
where z represents non-medical consumption.
K=
(5)
In this setting, welfare changes are a function of changes in medical treatments, their
expected health outcomes, and their costs over time. The first term on the right-hand side
of equation (5) is the health benefit resulting from changes in health care, expressed in
constant dollars. The second term is the change in the cost of health care. In Canada, the
change in costs is predominantly a change in taxes and insurance premiums paid. If K is
positive, the agent is better off in period t1 than in period t0 and conversely. The question
is: How do these changes in technology, outcomes and costs affect the price of treating
cancer?
Once we have measure the benefits and the costs, we can convert these estimates into a
price index, by scaling them by the cost of reaching the baseline level of utility in the
base year 1995. Baseline resources involved in providing for the patients are the net
consumption in 1995, which is approximated by the initial income (Y0). Thus, the
Laspeyres COL index (COLI) between period t0 and period t1 is given by the difference
of the initial value of the index (which is always 1) and the change in the COLI (K)
scaled by the initial income (Y0).
COLI = 1 −
K
Y0
(6)
7
4. SUMMARY STATISTICS
Table 1 summarizes the characteristics of cancer patients in 1995/96, 2001/02 to
2003/045. There are 1,966 observations in 1995/96, 4,599 observations in 2001/02, 6,423
in 2002/03 and 5,813 observations in 2003/04. The increase in the sample size is mainly
attributed to the increase in reporting hospitals in the OCCI database and not to a sharp
increase in the incidence of cancer. The proportion of males increased across the four
periods from 47.2% to 55.2%. Cancer is more common among patients between 60 and
79 years old, even with the large increase of patients aged between 50 to 59. The average
real cost (GDP deflator, 2001=100) in the treatment of the four cancers increased
annually at 1.7% from 1995/96 to 2001/02, then increased by 16% from 2001/02 to
2002/03 and 11.5% from 2002/03 to 2003/04. Although, we used the converted diseases
codes ICD-10 to ICD-9, the new classification may explain a part of the large increase in
cost in 2002/03 and 2003/04. We can’t assess how the changing classification code
affects the costs. However, even with the large increase, our key question remains: Is the
benefit from new technologies in cancer treatments higher than the cost?
Table 1: Average Real Cost and Characteristics of all four cancer patients
Year
1995/96
2001/02
2002/03
2003/04
Real Cost Number of % of
Age Distribution (%)
($ 2001)
cancer
male 10/19 20/29 30/39 40/49 50/59 60/69 70/79 80/89 90+
6,471
1,966
47.2 0.3 3.5 9.9 15.9 28.2 27.8 12.9 1.7
7,177
4,599
51.6 0.02 0.4 2.7 10.4 21.9 28.7 25.6 8.9 1.5
8,333
6,423
54.1 0.02 0.3 2.1 8.6 20.8 30.6 26.2 10.4 1.0
9,292
5,813
55.2 0.02 0.3 2.1 8.4 21.1 30.4 26.0 10.7 1.0
Note: Years 1995/96 and 2001/02 are classified according to ICD-9, while 2002/03 and 2003/04 are
originally classified according to ICD-10, but than converted into ICD-9.
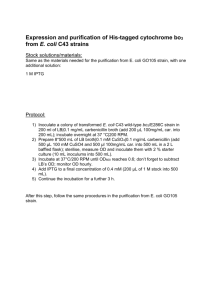
Graph 1 shows the real average cost (GDP deflator, 2001=100) of each treatment
categories for all four cancers. Over the period studied, prices increased for all categories,
except for radiotherapy where the price decreased annually by 8.8%. It should also be
remarked however, that the base year for radiology was the smallest observation in the
dataset, with 16 cases. Between 1995/96 and 2001/02, chemotherapy prices decreased at
an annual rate of 3.6%, however it increased substantially over the subsequent years.
5
Appendix 1 presents average real cost and characteristic for each cancer over the period study.
8
Graph 1: Average real cost of patients for treatment categories from 1995/96 to 2003/04.
16,000
Average real costs (GDP deflator, 2001=100)
14,000
12,000
10,000
8,000
6,000
4,000
Diagnostic procedures only
Diagnostic procedures & others
Surgical procedures
2,000
Chemotherapy
Radiotherapy
No procedure
0
1995/96
2001/02
2002/03
2003/04
Years
Table 2 presents the utilization (%) of the six categories of treatments. Across the years,
there is a net increase in the use of diagnostic procedures and radiotherapy, while the use
of surgical procedures and patients admitted to hospital without procedure decreased.
However, as we know a combination of treatments is often used for effectively
controlling and treating the cancer, given that these categories are probably more
complementary treatments.
Table 2: Utilization of Treatment Categories for all four cancers (%)
Category of
Treatments
1995/96
2001/02
2002/03
Diagnostics Only
7.9
6.3
8.0
Diagnostics & Others
3.1
2.7
3.2
Surgical Procedures
77.7
78.5
74.8
Chemotherapy
1.1
3.2
1.7
Radiotherapy
0.8
3.9
2.8
No Procedure
9.4
5.3
9.5
2003/04
10.9
3.5
73.7
1.5
3.4
7.0
9
5. RESULTS
To build the aggregated SPI, we use the year 1995/96 as our base period, which means
that the index equals 100 and we present the index for the three last year available
2001/02, 2002/03 and 2003/04. From equation (1), the aggregated SPI for the six
treatment categories altogether is rewritten:
SPI 95−t1
= α DP
where α c =
p DP , t1
p DP ,95
TC c ,95
TC Cancer ,95
+ α DPO
p DPO , t1
p DPO ,95
+ α SP
p SP , t1
p SP ,95
+αC
pC , t1
pC ,95
+αR
p R , t1
p R ,95
+ α NP
p NP , t1
p NP ,95
,
for c = DP, DPO, SP, C , R, NP and TC = Total Cost ,
t1 = 2001/02, 2002/03 and 2003/04, and DP = Diagnostic Procedures Only, DPO =
Diagnostic Procedures & Others, SP = Surgical Procedure, C = Chemotherapy, R =
Radiotherapy, NP = No Procedure.
Table 3 presents aggregated SPI. The aggregated SPI rose at an average annual rate of
1.9% from 1995/96 to 2001/02, which is similar to the price increase for all goods and
services in the economy. With the newer ICD-10, the SPI increased by 7.5% between
2001/02 and 2002/03, and the year after, it grew by 12.5%, which means that the same
basket of cancer treatments is much more expensive. We observe that the second year
under ICD-10 also presents a large increase, which make us think that the effect of the
new classification on costs is small.
However, the conversion table or the new
classification may still affect the results.
Table 3: Aggregated Service Price Index (fixed basket Laspeyres)
Years
Index
Annual growth rate
1995/96 (ICD-9)
100
2001/02 (ICD-9)
112.4
1.9%
2002/03 (ICD-10)
120.8
7.5%
2003/04 (ICD-10)
135.9
12.5%
Since the SPI fixed basket has the disadvantage of keeping the basket of goods fixed, this
version of the Laspeyres index presents an upward bias because all productivity gains are
10
(9)
assumed to be simply pure price movements. To incorporate quality adjustments over
time, we measure the COLI. This index focus on patient welfare (which means treatment
outcome-utility) and measures how much patients would be willing to pay or would have
to be compensated to keep the same level of utility and accept changes in medical
treatments and prices over time.
Whereas the COLI is a cost and benefit approach, the key question is about estimating the
benefits of health care. Several approaches may be used. We use the incidence and death
from CCR and NCIRS databases to compute mortality rate by age category based on 5
years prevalence and turn it into change in life-expectancy in order to estimate the
expected benefits of cancer treatments in Ontario for years 1995, 2001 and 2002. Due to
data limitations, the expected benefits for the year after 2002 is not calculated and as well
quality of life is not taken into account, therefore, benefits of cancer treatments are
partially accounted.
Table 4 presents the expected benefit of changing technologies of cancer treatments.
According to our data, death rate for the four types of cancer declined over time, and lifeexpectancy (LE) for cancer patients improved from 7 years 2 months in 1995/96 to 8
years 8 months in 2001/02, and to 10 years 9 months in 2002/036. The key issue about
improvement in life expectancy is whether it could be explained by improved
technologies in health care or other factors such as behavior changes (e.g. people are
more conscientious and do earlier diagnosis tests), improved socioeconomic status, public
health interventions, etc. Following the previous analyses of COLI in the health care
sector already referred to, we assume that 30% of gain in LE in cancer is due to better
health care technology. This implies that benefit of changing technologies of cancer
treatments is estimated about 6 months from 1995 to 2001, and about 1 year and 1 month
from 1995 to 2002.
6
Appendix 2 shows the life expectancy in 1995, 2001 and 2002 for each cancer.
11
Table 4: Expected benefit of changing technologies of cancer treatments.
Years
Death rate
Life Expectancy
Gains in LE since 1995 from
new technologies (30%)
1995/96
13.5%
7 years 2 months
---2001/02
11.0%
8 years 8 months
6 months
2002/03
8.3%
10 years 9 months
1 year 1month
2003/04
N/A
N/A
N/A
In order to estimate the COLI for cancer, we have to convert these life expectancy gains
into dollar values. We denote the value of a year of life as V, the additional length of life
in cancer patients as L, the additional length of life due to new technologies in cancer as l,
and the real discount rate as r; then the present value of remaining life Ω is given by:
Ω=
V *l
(1 + r )L
(8 )
The value of the LE gain is based on the value of a year of additional life for cancer
patient V and 3% discount rate. Our benchmark assumption is $50,000, which is an
average figure for the value of an additional year of life for an individual with an illness.
But three others scenarios are simulated: with a value of life-year of $10,000, $25,000
and $75,000. Then, we need to compare this additional value of life with the change in
cost of treating cancer.
Table 5 shows the COLI for cancer for the year 2001/027. Based on a 3% discount rate,
benefits from an additional year of life gained due to improved treatment over the period
worth $21,986, while the change in cost is less than $1,000. Thus, the willingness to pay
is evidently positive. Then, we turn this willingness to pay into a price index by scaling it
by the cost of reaching the baseline level of utility in 1995/96. We assume the baseline
level utility equal to the annual net consumption, which we assume is $25,000 for a
cancer patient. This yields to an amount of $145,016 in present values for the entire
expected survival period. The second last row shows the COLI index for 2002/03 and the
7
Appendix 3 displays the detail components of COLI for cancer in 2002/03.
12
last row indicates the average annual change in the COLI between 1995/96 and 2002/03.
Using the benchmark assumption, the COLI fell by 2.6% annually. Whatever the value of
a life-year is, the index is falling in each case.
Table 5: Cost-of-living index (COLI) for cancer in 2001/02 (1995/96 = 100)
Value of longevity (Benefits) for a
OCCI Real AC
baseline value of life-year of
$ 2001
Life
Year
Expectancy $10,000 $25,000 $50,000 $75,000
AC
Change
6,471
1995/96 7yrs 2m
4,397
10,993
21,986
32,979
7,177
706
2001/02 8yrs 8m
3,691
10,286
21,280
32,273
Willingness To Pay
Y0= $145,016
COLI=(1-K/Y0) *100
97.5
92.9
85.3
77.7
Annual Change in
-0.43%
-1.22%
-2.61%
-4.11%
COLI
Table 6 summarizes the COLI according to our benchmark assumption and the annual
growth rate during the period under study. From 1995/96 to 2001/02, the annual growth
rate decreased by 2.6% and from 2001/02 to 2002/03 it decreased by 20%. This large
decrease is due to the lower death rate in 2002 giving a large life expectancy
improvement. These results clearly indicate that taking into account health outcomes,
price of cancer treatment is falling rapidly. Although cancer prevalence is increasing,
more effective treatments justify the growth on total costs.
Table 6: Cost-of-Living Index (baseline value of life year $50,000)
Years
Index
Annual growth rate
1995/96 (ICD-9)
100
2001/02 (ICD-9)
85.3
-2.6%
2002/03 (ICD-10)
68.1
-20.2%
5. CONCLUSION
Technological change in cancer care is worth the cost. Technology increases spending,
but the health benefits more than justify the added costs. Through the Cost-of-living
index, we showed that the net benefits of new technologies are largely positive over the
period studied, even with the newer ICD-10/CCI that might have overstated the costs. As
well, the low (negative) value of COLI compared with the SPI suggests that the usual
13
way to calculate indexes has an upward bias. Our results support the growing
international evidence that outcome-adjusted costs of care for some diseases are falling.
This study has limitations relative to data used. We only had access to hospital cost and
an important assumption was made, all costs during the stay are attributable to the main
diagnosis and to the principal procedure reported by the physician. Next steps would be
to develop data and a methodology that take into account either comorbidities or change
in quality of life. Although hospital costs represent 74% of the direct costs associated
with cancer, a study to distinguish price change to quantity/quality change in the
pharmacy sector would be useful for a better understanding of the effect of new cancer
technologies.
14
REFERENCES
Ariste, R., B. Belhadji, C.D. Mallory (2006), “Are health care prices really rising?
Evidence from heart attack treatment in Canada,” Unpublished paper, Canadian Institute
for Health Information and Health Canada.
Berndt, E.R., A.B. Busch, R.G. Frank, S-L. Normand (2005), “Real output in mental
health care during the 1990s,” Working Paper, National Bureau of Economic Research,
Cambridge.
Berndt, E.R., D.M. Cutler, R.G. Frank, Z. Griliches, J.P. Newhouse, and J.E. Triplett
(2001), “Price Indexes for Medical Care Goods and Services: An Overview of
Measurement Issues,” In: D.M. Cutler and E.R. Berndt, Medical Care Output and
Productivity, pp. 141-200, University of Chicago Press.
Canadian Cancer Society/National Cancer Institute of Canada (2005), Canadian Cancer
Statistics 2005, Toronto, Canada.
Cutler, D.M., M. McClellan (2001), “Is Technological Change In Medicine Worth It?,”
Health Affairs, September/October 2001, p. 11-29.
Cutler, D.M., M. McClellan, J. P. Newhouse, and D. Remler (1998), “Are Medical
Prices Falling? Evidence from Heart Attack Treatments,” Quarterly Journal of
Economics, November 1998, pp. 991-1024.
Cutler, D.M., and E. Meara (2000), “The Technology of Birth: Is It Worth It?,” In :
Frontiers in Health Policy Research, vol. 3, ed. A. Garber , pp. 33-67, Cambridge, Mass.:
MIT Press.
Fisher and Shell (1972), The economic theory of price indices, New York Academic
Press.
Jeanrenaud, C., H. Chevrou-Severac, J.B. Wasserfallen (2004), “L’accroissement des
dépenses en santé : hausse des coûts ou amélioration des prestations ?,” Unpublished
paper, Colloque du PNR-45 Etat Social, Berne.
15
APPENDIX 1
Real Cost and Characteristics of cancer patients
Age Distribution (%)
Real Cost Number % of
Cancer
Year
of
($ 2001)
male
cancer
10/19 20/29 30/39 40/49 50/59 60/69 70/79 80/89 90+
1995/96 7,799.87
225 63.1 0.9
7.1 16.4 36.4 31.1
7.1
0.9
2001/02 9,001.52
503 57.7 1.4
2.8
8.6 17.9 31.6 30.2
6.8
0.8
Lung 2002/03 10,701.17 1,843 56.6
0.1
0.3
1.2
6.5 17.8 32.5 31.8
9.6
0.4
2003/04 11,753.46 1,695 57.1
0.1
0.4
0.8
6.8 17.4 31.3 34.0
9.1
0.2
1995/96 3,435.06
613
0 0.5
7.3 20.7 22.5 22.5 19.1
6.4
1.0
2001/02 3,518.47
1242 0.4 0.4
6.3 20.4 26.4 21.7 18.3
5.9
0.6
Breast
2002/03 4,163.75 1,328 0.8 0.2
5.6 19.8 25.3 23.2 17.8
7.4
0.8
2003/04 4,656.73 1,065 0.9 0.2
5.8 20.2 26.5 21.1 17.6
7.7
0.9
1995/96 5,139.47
433 100 0.9
1.4 10.9 34.0 36.3 15.2
1.4
2001/02 4,973.72
1109 100 3.1 25.1 42.3 23.3
5.5
0.8
Prostate
2002/03 5,756.23 1,378 100 3.8 23.7 42.7 20.8
8.1
1.0
2003/04 5,877.66 1,251 100 0.1
2.9 26.9 43.9 18.0
7.4
0.1
1995/96 9,548.46
695 50.8 0.4
2.5
6.5 13.0 26.9 29.1 19.0
2.7
Colo- 2001/02 10,656.44
1745 55.6
0.1
0.5
1.8
8.5 17.7 24.2 30.9 13.8
2.6
rectal 2002/03 10,852.19 1,874 55.8 0.4
2.1
6.5 18.4 25.2 30.6 15.1
1.7
2003/04 12,085.73 1,802 54.3 0.6
2.3
6.7 17.4 25.8 29.1 16.2
1.9
16
APPENDIX 2
Estimation LE from the CCR-Both sex, weighted average for all age groups
Cancer
Lung
Breast
Prostate
Colorectal
4cancers
LE1995
LE 2001
2.11
16.66
11.88
6.69
7.17
LE 2002
1.95
20.02
15.66
8.25
8.71
2.41
26.85
20.1
10.75
10.74
17
APPENDIX 3
Cost-of-living index (COLI) for cancer in 2002/03 (1995/96 = 100)
Value of longevity (Benefits) for a
OCCI Real AC
baseline value of life-year of
$ 2002
Life
Year
Expectancy $10,000 $25,000 $50,000 $75,000
AC
Change
6,538
1995/96 7yrs 2m
9,640
24,100
48,199
72,299
8,419
1,881
2002/03 10yrs 9m
7,759
22,219
46,318
70,418
Willingness To Pay
Y0= $145,016
COLI=(1-K/Y0) *100
94.6
84.7
68.1
51.4
Annual Change in
-0.78%
-2.35%
-5.35%
-9.06%
COLI
18