Ability to perform a single heel-rise is significantly related to
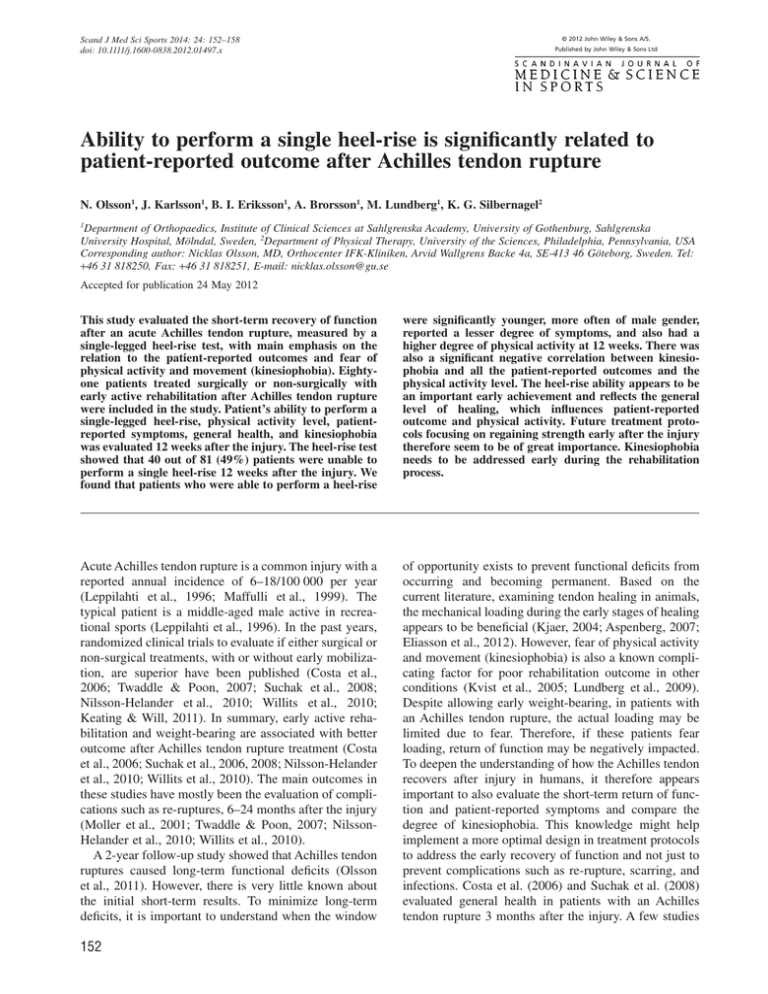
advertisement
© 2012 John Wiley & Sons A/S. Scand J Med Sci Sports 2014: 24: 152–158 doi: 10.1111/j.1600-0838.2012.01497.x Published by John Wiley & Sons Ltd Ability to perform a single heel-rise is significantly related to patient-reported outcome after Achilles tendon rupture N. Olsson1, J. Karlsson1, B. I. Eriksson1, A. Brorsson1, M. Lundberg1, K. G. Silbernagel2 1 Department of Orthopaedics, Institute of Clinical Sciences at Sahlgrenska Academy, University of Gothenburg, Sahlgrenska University Hospital, Mölndal, Sweden, 2Department of Physical Therapy, University of the Sciences, Philadelphia, Pennsylvania, USA Corresponding author: Nicklas Olsson, MD, Orthocenter IFK-Kliniken, Arvid Wallgrens Backe 4a, SE-413 46 Göteborg, Sweden. Tel: +46 31 818250, Fax: +46 31 818251, E-mail: nicklas.olsson@gu.se Accepted for publication 24 May 2012 This study evaluated the short-term recovery of function after an acute Achilles tendon rupture, measured by a single-legged heel-rise test, with main emphasis on the relation to the patient-reported outcomes and fear of physical activity and movement (kinesiophobia). Eightyone patients treated surgically or non-surgically with early active rehabilitation after Achilles tendon rupture were included in the study. Patient’s ability to perform a single-legged heel-rise, physical activity level, patientreported symptoms, general health, and kinesiophobia was evaluated 12 weeks after the injury. The heel-rise test showed that 40 out of 81 (49%) patients were unable to perform a single heel-rise 12 weeks after the injury. We found that patients who were able to perform a heel-rise were significantly younger, more often of male gender, reported a lesser degree of symptoms, and also had a higher degree of physical activity at 12 weeks. There was also a significant negative correlation between kinesiophobia and all the patient-reported outcomes and the physical activity level. The heel-rise ability appears to be an important early achievement and reflects the general level of healing, which influences patient-reported outcome and physical activity. Future treatment protocols focusing on regaining strength early after the injury therefore seem to be of great importance. Kinesiophobia needs to be addressed early during the rehabilitation process. Acute Achilles tendon rupture is a common injury with a reported annual incidence of 6–18/100 000 per year (Leppilahti et al., 1996; Maffulli et al., 1999). The typical patient is a middle-aged male active in recreational sports (Leppilahti et al., 1996). In the past years, randomized clinical trials to evaluate if either surgical or non-surgical treatments, with or without early mobilization, are superior have been published (Costa et al., 2006; Twaddle & Poon, 2007; Suchak et al., 2008; Nilsson-Helander et al., 2010; Willits et al., 2010; Keating & Will, 2011). In summary, early active rehabilitation and weight-bearing are associated with better outcome after Achilles tendon rupture treatment (Costa et al., 2006; Suchak et al., 2006, 2008; Nilsson-Helander et al., 2010; Willits et al., 2010). The main outcomes in these studies have mostly been the evaluation of complications such as re-ruptures, 6–24 months after the injury (Moller et al., 2001; Twaddle & Poon, 2007; NilssonHelander et al., 2010; Willits et al., 2010). A 2-year follow-up study showed that Achilles tendon ruptures caused long-term functional deficits (Olsson et al., 2011). However, there is very little known about the initial short-term results. To minimize long-term deficits, it is important to understand when the window of opportunity exists to prevent functional deficits from occurring and becoming permanent. Based on the current literature, examining tendon healing in animals, the mechanical loading during the early stages of healing appears to be beneficial (Kjaer, 2004; Aspenberg, 2007; Eliasson et al., 2012). However, fear of physical activity and movement (kinesiophobia) is also a known complicating factor for poor rehabilitation outcome in other conditions (Kvist et al., 2005; Lundberg et al., 2009). Despite allowing early weight-bearing, in patients with an Achilles tendon rupture, the actual loading may be limited due to fear. Therefore, if these patients fear loading, return of function may be negatively impacted. To deepen the understanding of how the Achilles tendon recovers after injury in humans, it therefore appears important to also evaluate the short-term return of function and patient-reported symptoms and compare the degree of kinesiophobia. This knowledge might help implement a more optimal design in treatment protocols to address the early recovery of function and not just to prevent complications such as re-rupture, scarring, and infections. Costa et al. (2006) and Suchak et al. (2008) evaluated general health in patients with an Achilles tendon rupture 3 months after the injury. A few studies 152 Achilles tendon rupture, short-term result have reported the return of function at 3 months (Kangas et al., 2003; Twaddle & Poon, 2007; Keating & Will, 2011), but as far as we know, no study has evaluated function in connection to how it may affect the patients’ general health and quality of life. The purpose of this study was therefore to evaluate the recovery of function at 12 weeks after the injury and to study how function relates to the patient-reported outcomes, with regard to the lower limb function, as well as general health and quality of life. The secondary purpose was to evaluate the degree of patients’ fear of movement and how this fear relates to function and patient-reported symptoms. We hypothesized that patients who are able to perform a single-legged heel-rise at 12 weeks would report less symptoms, report higher level of physical activity, and less impact on function of daily activity and sports and improved quality of life compared with patients that were unable. Furthermore, we hypothesized that the degree of kinesiophobia would correlate with patientreported symptoms, quality of life, and function. Materials and methods The study is part of a randomized controlled trial (RCT) conducted at the Department of Orthopedics Sahlgrenska University Hospital, Gothenburg, Sweden. Patients, 18–65 years of age, were included if they had an acute mid-substance rupture presented within 4 days. The subjects were randomized to either surgical or non-surgical treatment. The results of the RCT will be presented separately. In this short-term follow-up, we have included the first 81 patients, from the larger randomized study. One patient was lost to follow-up at the 12-week evaluation. Between April 2009 and September 2010, a total of 81 (69 males and 12 females) patients had been followed up for 12 weeks. The mean [standard deviation (SD)] age was 40 (10), the mean (SD) weight was 84 (12) kg, and the mean (SD) height was 179 (8) cm. All subjects gave written informed consent to participate in the study. Ethical approval was obtained from the Regional Ethical Review Board in Gothenburg, Sweden. Treatment procedure Surgical group Forty patients were treated surgically with open repair using identical suture technique. The tendon was repaired end-to-end with core suturing using two semi-absorbable sutures (No. 2 Orthocord™; Depuy Mitek, Norwood, Massachusetts, USA) in a modified Kessler technique (Kessler, 1973). A running circumferential suture was used with absorbable sutures (No. 0 Polysorb™; Tyco, Norwalk, Connecticut, USA) using a modified Silvferskiold technique (Silfverskiold & May, 1994) to reinforce the core sutures. The patients were post-operatively immobilized in a pneumatic walker brace (Aircast XP Diabetic Walker; DJO, Vista, California, USA) including heel pads. No cast was used. Patients were allowed full weight-bearing immediately post-operatively. During the first 2 weeks, no other specific rehabilitation recommendation was prescribed besides the weight-bearing. The following 4 weeks, active rehabilitation following a standardized protocol including training without brace under the supervision of a physical therapist was performed. In this group, the brace was used for a total time of 6 weeks. Non-surgical group Forty-one patients were included in the non-surgical group. Treatment started immediately after the randomization using the same brace as in the surgical group. Full weight-bearing was allowed from the start. This treatment group started the active rehabilitation, supervised by a physical therapist, when the brace was removed at 8 weeks. Evaluation All the patients were evaluated at mean (SD) 12 (0.9) weeks by the same physical therapist at our testing laboratory. The evaluating physical therapist was not involved in the treatment of the patients. Patient-reported outcome and physical activity Questionnaires were used to evaluate patient-reported outcome and were answered prior to the functional testing. All the scores used have in previous studies been shown to be reliable and valid (Grimby, 1986; EuroQol, 1990; Roos et al., 2001; Lundberg et al., 2004; Nilsson-Helander et al., 2007). The Physical Activity Scale (PAS) questionnaire (Grimby, 1986) was used to evaluate the activity level and a score of 1 equals to no physical activity, whereas a score of 6 equals to heavy physical exercise several times per week. The Achilles Tendon Total Rupture Score (ATRS) (Nilsson-Helander et al., 2007) was used to evaluate injury specific patient-reported outcome. The ATRS ranges from 0 to 100; a lower score indicates more symptoms and greater limitations of physical activity. Three subscales of the Foot and Ankle Outcome Score (FAOS) (Roos et al., 2001) were used to get a foot and ankle perspective: function in daily living (ADL), function in sport and recreation (Sport&Rec), and foot- and ankle-related quality of life (QoL). All the subscales of FAOS ranged from 0 to 100 and a score of 0 indicates extreme foot- and ankle-related symptoms, whereas 100 indicates no symptoms. For measuring the general healthrelated quality of life, EQ-5D (EuroQol Group) was used (EuroQol, 1990; Brooks, 1996). An EQ-5D score of 0 is considered to be the worst imaginable health state and a score of 1.00 is considered the best imaginable health state. One should notice that the quality-of-life scores FAOS QoL and EQ-5D differ from each other in terms of different perspective, such as quality of life from a foot and ankle perspective (FAOS) or a total health state (EQ5D). Fear of physical activity and movement was measured with the Tampa Scale for Kinesiophobia Swedish Version (TSK-SV) (Lundberg et al., 2004). TSK varies between 17 and 68. A high TSK value indicates a high degree of kinesiophobia. Kinesiophobia is defined when the value is more than 37. At the time of inclusion (baseline), PAS and EQ-5D were measured. During the follow-up at 12 weeks, all the scores above were measured (PAS, ATRS, FAOS, EQ-5D, and TSK-SV). Functional evaluation The single heel-rise test is a part of a more extensive functional evaluation, but the ability to perform a single-legged heel-rise is the only functional outcome measurement reported in this study. This test is simple to perform in the clinic and we believe it to be suitable in this early stage of rehabilitation. In several other Achilles tendon studies (Moller et al., 2002, 2005; Weber et al., 2003; Bostick et al., 2010; Silbernagel et al., 2010), single-legged heel-rise is a commonly used test. Prior to testing, the patients 153 Olsson et al. warmed up for 5 min on a stationary bicycle and then performed 3 sets of 10 two-legged heel-rises. Standardized instructions were used prior to testing. The participants were standing on a flat box with the ankle in neutral position and asked to perform a single heel-rise. The patients were classified as being able to perform a one-legged heel-rise if they were able to lift the heel at least 2 cm once while keeping the knee straight. MuscleLab® (Ergotest Technology, Oslo, Norway) measurement system was used for the evaluations as previously described in the literature (Silbernagel et al., 2010). A linear encoder was used. A spring-loaded string is connected to a sensor inside the liner encoder unit. When the string is pulled, the sensor outputs a series of digital pulses that is proportional to the distance traveled. The resolution is approximately one pulse every 0.07 mm. The spring-loaded string of the linear encoder was attached to the heel of the subject’s shoe. Table 1. Demographics and results from the 12-week evaluation Variable 12 weeks Number of patients Age (years) 81 40.0 (9.6) 40 (20; 63) 69 (85%) 12 (15%) 2.9 (1.0) 3 (1; 6) 38.8 (17.3) 37 (6; 86) 77.8 (15.5) 81 (13; 100) 31.1 (19.1) 30 (0; 80) 42.6 (17.2) 44 (0; 75) 0.75 (0.16) 0.73 (0.19; 1.00) 35.9 (7.5) 35 (18; 60) 41/40 51%/49% Male (n) Female (n) PAS ATRS FAOS – ADL FAOS – Sport&Rec FAOS – QoL EQ-5D Statistical analysis Descriptive data are reported as mean, median, SD, and range (minimum-maximum) in the tables and in the text as mean and SD. The Mann-Whitney U-test was used for continuous variables to compare different groups. The level of significance was set at P < 0.05. For comparison between groups, the chisquare test was used for dichotomous variables and Fischer’s exact test when the sample size was small. The correlations were analyzed with Spearman’s rank correlation. All data were analyzed using SPSS statistics (version 18.0, SPSS inc., Chicago, Illinois, USA). Results Comparison between the initial treatment groups At the 12-week evaluation, there was no statistical difference (P = 0.269) between surgical and non-surgical group according to heel-rise ability. The number of patients with the ability to perform a single heel-rise was 23 out of 40 (58%) in the surgical treated group and 18 out of 41 (44%) in the non-surgical group. There were no statistical differences (P-values: 0.18–0.88) between the two treatment groups in terms of demographics and other parameters at baseline (PAS and EQ-5D) or at the 12-week evaluation [PAS, ATRS, FAOS (ADL, Sport&Rec, and QoL), EQ-5D, and TSK-SV]. Therefore, we present the results for the whole group regardless of treatment. Patient-reported outcome at 12 weeks At the 12-week evaluation, the patient-reported questionnaires show that the patients have symptoms affecting function and quality of life (Table 1). According to the reported physical activity level, there was a significant (P < 0.001) reduction of physical activity 12 weeks after the injury, 2.9(1.0) compared with baseline 4.1(1.1). There was also a significant reduction (P < 0.001) of EQ-5D from the baseline value of 0.97(0.08) to 0.75(0.16) 12 weeks after the injury. 154 TSK Heel-raise ability (yes/no) For categorical variables, data are reported as n and (%). For continuous variables mean (standard deviation)/median (minimum–maximum). Patient-reported outcomes scores (normal range): PAS [Physical Activity Scale (1–6)], ATRS [Achilles Tendon Total Rupture Score (0–100)], FAOS [Foot and Ankle Outcome Score (0–100)], and the subscales: ADL (function in daily living), Sport&Rec (function in sport and recreation) and QoL (foot- and ankle-related quality of life), EQ-5D [EuroQol Group, general health-related quality of life (0–1.00)], and TSK-SV [Tampa Scale for Kinesiophobia Swedish Version (17–68)]. Function at 12 weeks The heel-rise test showed that 40 out of 81 (49%) patients were unable to perform a single heel-rise 12 weeks after the injury (Table 1). Recovery of function in relation to age, gender, and symptoms Ability to perform a heel-rise at 12 weeks related to age, gender, and symptoms are shown in Table 2. We found that patients who were able to perform a heel-rise were significantly younger, more often of male gender and had a higher score in ATRS and all subscales of FAOS, and had a higher degree of physical activity at 12 weeks. There was no significant difference (P = 0.270) between the degree of kinesiophobia between patients who were able to perform a heel-rise and those who could not. Correlation between degree of kinesiophobia and patient-reported outcome At the 12-week evaluation, we found a highly significant negative correlation between the TSK-SV score and ATRS, FAOS – ADL, FAOS – Sport&Rec, and FAOS – Achilles tendon rupture, short-term result Table 2. Comparison between patients who were able to perform a heelrise and those who were not Variable Heel-rise YES Heel-rise NO Number of patients Age (years) 41 (51%) 36.8 (8.3) 37.0 (20; 58) 39 2 3.2 (1.0) 3 (2; 6) 44.7 (17.4) 43 (9; 86) 82.3 (12.5) 85 (53; 97) 36.3 (19.0) 40 (5; 80) 49.2 (16.3) 50 (19; 75) 0.78 (0.15) 0.73 (0.29; 1.00) 35.0 (6.9) 36 (18; 52) 40 (49%) 43.2 (9.9) 43 (27; 63) 30 10 2.7 (1.1) 3 (1; 6) 32.8 (15.3) 31 (6; 73) 73.2 (17.0) 74 (13; 100) 25.8 (17.7) 25 (0; 65) 35.7 (15.7) 31 (0; 69) 0.72 (0.17) 0.73 (0.19; 1.00) 36.9 (8.0) 34 (20; 60) Male Female PAS ATRS FAOS – ADL FAOS – Sport&Rec FAOS – QoL EQ-5D TSK P-value 0.005 0.013 0.022 0.002 0.008 0.017 0.001 0.094 0.270 For categorical variables, data are reported as n and (%). For continuous variables mean (standard deviation)/median (minimum–maximum). For comparison between groups, the Fischer’s exact test was used for dichotomous variables. The Mann-Whitney U-test was used for continuous variables. ADL, function in daily living; ATRS, Achilles Tendon Total Rupture Score; EQ-5D, EuroQol Group, general health-related quality of life; FAOS, Foot and Ankle Outcome Score; PAS, Physical Activity Scale; QOL, foot and ankle-related quality of life; Sport&Rec, function in sport and recreation; TSK-SV, Tampa Scale for Kinesiophobia Swedish Version. Table 3. Evaluation of relationship between level of kinesiophobia (TSKSV) and patient-reported outcome at 12 weeks Variable Correlations coefficient* P-value (two-tailed) PAS ATRS FAOS – ADL FAOS – Sport&Rec FAOS – QoL EQ-5D -0.275 -0.371 -0.376 -0.346 -0.321 -0.239 0.013 0.001 0.001 0.002 0.003 0.032 *Spearman’s rank correlation was used. ADL, function in daily living; ATRS, Achilles Tendon Total Rupture Score; EQ-5D, EuroQol Group, general health-related quality of life; FAOS, Foot and Ankle Outcome Score; PAS, Physical Activity Scale; QoL, foot- and ankle-related quality of life; Sport&Rec, function in sport and recreation; TSK-SV, Tampa Scale for Kinesiophobia Swedish Version. QoL. A negative correlation was also found between TSK-SV and PAS and EQ-5D, respectively, at 12 weeks (Table 3). Discussion The most important finding in our study was that at 12 weeks, approximately only half of the patients had achieved the ability to perform a single-legged heel-rise. The patients who were able to perform a heel-rise were significantly younger, more often of male gender, had less patient-reported symptoms, and had a higher degree of physical activity. The degree of kinesiophobia measured with TSK-SV was also negatively correlated with symptoms and measures of general health. Thus, our hypotheses were confirmed. The ability to perform a heel-rise appears to be an important milestone in patients’ recovery following an Achilles tendon rupture. To be able to test the hypothesis of the present study, we collected data from a cohort, which was a part of a larger study, where we collected data at the time of rupture and at 12 weeks. At the time of this study, the patients had undergone 4 or 10 weeks (depending of the treatment group) of supervised rehabilitation focused on regaining calf muscle strength and function. In comparison with other studies, this can be considered as an early start of the rehabilitation exercises. Despite the early start of the exercises, supervised by physical therapists, only half of the patients were able to perform the singlelegged heel-rise and there was no difference between the two treatment groups. It could be questioned if the treatments and outcomes in the present study are comparable to other studies. In order to put our results into perspective of the literature, we have only found one publication presenting short-term data on one-legged heel-rise after acute Achilles tendon rupture. Uchiyama et al. (2007) showed at 12 weeks that after modified surgical technique, approximately half of the patients were able to perform a single-legged heel-rise. They also reported the timing for achieving this critical test to a mean of 12 weeks (range: 7–25 weeks). The injury- and joint-specific questionnaires all indicate that the patients have major symptoms relating to their foot and ankle, along with limitations in activities of daily living, physical activity, and quality of life. Because the degree of patient-reported symptoms were significantly different between the group who could perform a heel-rise and those who could not, deficit in calf muscle strength appears to have a profound impact on the patient’s recovery. The results regarding patientreported outcome could also be very useful both to clinicians and patients in providing information about realistic short-term expectations with regard to recovery and symptoms. Not only did this patient group have deficits in lower leg function and patient-reported symptoms, but their general health also appeared to be negatively affected. As a comparison to our results, a general population study by Burstrom et al. (2001) had a mean EQ-5D of 0.86 (SD 0.009) in a corresponding age group. Our baseline value for these patients was higher. This might reflect that patients with an Achilles tendon rupture are more active and healthier compared with the general population. In the present study, there was a significant decrease in EQ-5D from baseline to 12 weeks. Costa 155 Olsson et al. et al. (2006) reported an EQ-5D value of 0.69–0.73 at 10 and 14 weeks after acute Achilles tendon rupture depending on the type of treatment. This corresponds well to the value reported in the present study 12 weeks after the injury and indicates that also general health is negatively affected at this time point. In the general population study, Burstrom et al. reported a similar EQ-5D value (0.74) in the age group of 80–88 years (Burstrom et al., 2001). Twelve weeks after an Achilles tendon rupture, there is a significant decrease in terms of physical activity, which is expected of course. Earlier studies have shown that even 2 years after the injury, approximately only half of the patients have reached their previous physical activity level (Moller et al., 2001). This patient group, in general, is very active and often describes a desire to return to the same activity level, but several studies have shown that this might not be the case, mainly due to deficits in lower leg function or fear of re-injury (Moller et al., 2001). At the present time, we do not know if the early recovery of heel-rise can predict the return to physical activity, but this would be of interest to investigate in future studies. Most studies and clinical guidelines recommend return to running and non-contact sports between weeks 16 and 20 (van Sterkenburg et al. 2008; Maffulli et al., 2011). In general, most of the guidelines are time-based and do not include any specific criteria with regard to return of strength or lower leg function. Costa et al. (2006) reported a median time of 12.5–18 weeks (depending of treatment) to return to normal walking. The Achilles Tendon Study Group has given guidelines for sport resumption in their book Achilles Tendon Rupture – Current Concepts (van Sterkenburg et al. 2008). They divided the recovery into four levels of increasing activity: walking, running, return to noncontact sport, and return to contact sport. Each phase must be fully accomplished prior to entering the next one. The first level ends when the patient is able to walk normally again. To achieve that, the difference in strength is said to be less than 25% compared with the uninjured side in repeated single heel-rises and also toe walking should be possible. The proposed time for this level is 12 weeks, but 8 weeks for operative treatment with a functional brace. We conclude similar to the Achilles Tendon Study Group that a functional perspective rather than a time perspective is of major importance when rehabilitation is advanced. On the other hand, our data do not support that the majority of patients could go into the Achilles Tendon Study Group’s next level of rehabilitation, including resumed running, after 12 weeks. This simple test of heel-rise ability appears to be an important milestone in the early rehabilitation process; however, its importance in relation to achieving a normal gait pattern needs to be further investigated. As indicated by the results of the present study, we suggest that the heel-rise test could have an important 156 clinical application and give realistic expectations for both the patient and the physical therapist/doctor with regard to expected return of various activities such as running and sports. However, if early return of a singlelegged heel-rise capacity is predictive of achieving a full recovery needs to be further investigated. Future treatment protocols focusing on treatment modalities allowing early weight-bearing and early strength training appears warranted based on this and other studies (Costa et al., 2006; Suchak et al., 2006, 2008; Willits et al., 2010). Identifying signs of kinesiophobia during the early stage of rehabilitation might also be of great importance in order to achieve compliance with early weightbearing and early exercise protocols. In the present study, it was shown that males had significant better functional outcome, based on the single heel-rise test, than females. Difference in gender has also been reported by Saxena et al. (2011) when they looked at parameters for predicting return to activity after Achilles tendon surgery. It has previously been suggested that there are gender differences in tendon healing (Magnusson et al., 2007; Miller et al., 2007; Westh et al., 2008). However, as Achilles tendon ruptures occur mostly in males, and in this study, only 15% of the included patients were females, it is difficult to draw any conclusions regarding possible differences in tendon healing. The results in the present study indicate that kinesiophobia is a factor that correlates negatively with the physical activity level, the degree of symptoms, and general health in patients 12 weeks following an Achilles tendon rupture (Table 3). This suggests that during the rehabilitation process this might need to be addressed separately by the treating physician and/or the physical therapist or rehabilitation specialist in order to achieve optimal outcome. The instructions to the patients in this study were that full weight-bearing was allowed and promoted from the start. It could be that patients with a higher degree of fear of movement actually do not weight-bear (less compliance) and load the tendon to the same degree as patients with less fear (high compliance). Histological studies have shown better collagen formation after mechanical loading (Jarvinen et al., 1997; Kannus et al., 1997; Rantanen et al., 1999; Kjaer et al., 2005). Clinical studies have also shown improved results of early functional treatment after an Achilles tendon rupture (Kangas et al., 2003; Maffulli et al., 2003; Costa et al., 2006; Nilsson-Helander et al., 2010; Willits et al., 2010). However, further studies are needed to evaluate if the degree of weight-bearing and loading of the tendon is affected by kinesiophobia. Perspectives Half of the patients were able to perform a singlelegged heel-rise at 12 weeks after an Achilles tendon rupture. The ability to perform a single heel-rise at this time is significantly related to physical activity and Achilles tendon rupture, short-term result patient-reported outcome. Male gender and younger age seem to be of importance to obtain a satisfactory functional outcome at 12 weeks after an Achilles tendon rupture. Future treatment protocols should focus on regaining strength in the calf muscle early in the rehabilitation process and we believe that the single-legged heel-rise test is critical in the recovery after an Achilles tendon rupture. In a functional perspective, this test might be an important tool to monitor the progress of the rehabilitation. The present study also demonstrated that kinesiophobia correlates with physical activity, patientreported symptoms, and general health. Fear of physical activity and movement needs to be addressed especially during the early stages of the rehabilitation process. Key words: Achilles Tendon Total Rupture Score (ATRS), Foot and Ankle Outcome Score (FAOS), EQ-5D, kinesiophobia, calf muscle strength. Conflict of interest The authors declare that they have no conflict of interest. Acknowledgements This study was supported by the Swedish National Centre for Research in Sports (CIF). References Aspenberg P. Stimulation of tendon repair: mechanical loading, GDFs and platelets. A mini-review. Int Orthop 2007: 31: 783–789. Bostick GP, Jomha NM, Suchak AA, Beaupre LA. Factors associated with calf muscle endurance recovery 1 year after achilles tendon rupture repair. J Orthop Sports Phys Ther 2010: 40: 345–351. Brooks R. EuroQol: the current state of play. Health Policy 1996: 37: 53–72. Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001: 10: 621–635. Costa ML, MacMillan K, Halliday D, Chester R, Shepstone L, Robinson AH, Donell ST. Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg Br 2006: 88: 69–77. Eliasson P, Andersson T, Aspenberg P. Achilles tendon healing in rats is improved by intermittent mechanical loading during the inflammatory phase. J Orthop Res 2012: 30: 274–279. EuroQol. EuroQol – a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy 1990: 16: 199–208. Grimby G. Physical activity and muscle training in the elderly. Acta Med Scand Suppl 1986: 711: 233–237. Jarvinen M, Jozsa L, Kannus P, Jarvinen TL, Kvist M, Leadbetter W. Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports 1997: 7: 86–95. Kangas J, Pajala A, Siira P, Hamalainen M, Leppilahti J. Early functional treatment versus early immobilization in tension of the musculotendinous unit after Achilles rupture repair: a prospective, randomized, clinical study. J Trauma 2003: 54: 1171–1180. Discussion 1180–1171. Kannus P, Jozsa L, Natri A, Jarvinen M. Effects of training, immobilization and remobilization on tendons. Scand J Med Sci Sports 1997: 7: 67–71. Keating JF, Will EM. Operative versus non-operative treatment of acute rupture of tendo Achillis: a prospective randomised evaluation of functional outcome. J Bone Joint Surg Br 2011: 93: 1071–1078. Kessler I. The “grasping” technique for tendon repair. Hand 1973: 5: 253–255. Kjaer M. Role of extracellular matrix in adaptation of tendon and skeletal muscle to mechanical loading. Physiol Rev 2004: 84: 649–698. Kjaer M, Langberg H, Miller BF, Boushel R, Crameri R, Koskinen S, Heinemeier K, Olesen JL, Dossing S, Hansen M, Pedersen SG, Rennie MJ, Magnusson P. Metabolic activity and collagen turnover in human tendon in response to physical activity. J Musculoskelet Neuronal Interact 2005: 5: 41–52. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005: 13: 393–397. Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand 1996: 67: 277–279. Lundberg M, Styf J, Carlsson S. A psychometric evaluation of the Swedish version of the Tampa Scale for Kinesiophobia (TSK) from a physiotherapeutic perspective. Physiother Theory Pract 2004: 20: 121–130. Lundberg M, Styf J, Jansson B. On what patients does the Tampa Scale for Kinesiophobia fit? Physiother Theory Pract 2009: 25: 495–506. Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in elite athletes. Foot Ankle Int 2011: 32: 9–15. Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med 2003: 31: 692–700. Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med 1999: 9: 157–160. Magnusson SP, Hansen M, Langberg H, Miller B, Haraldsson B, Westh EK, Koskinen S, Aagaard P, Kjaer M. The adaptability of tendon to loading differs in men and women. Int J Exp Pathol 2007: 88: 237–240. Miller BF, Hansen M, Olesen JL, Schwarz P, Babraj JA, Smith K, Rennie MJ, Kjaer M. Tendon collagen synthesis at rest and after exercise in women. J Appl Physiol 2007: 102: 541–546. Moller M, Lind K, Movin T, Karlsson J. Calf muscle function after Achilles tendon rupture. A prospective, randomised study comparing surgical and non-surgical treatment. Scand J Med Sci Sports 2002: 12: 9–16. Moller M, Lind K, Styf J, Karlsson J. The reliability of isokinetic testing of the ankle joint and a heel-raise test for endurance. Knee Surg Sports Traumatol Arthrosc 2005: 13: 60–71. Moller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br 2001: 83: 843–848. Nilsson-Helander K, Silbernagel KG, Thomee R, Faxen E, Olsson N, Eriksson BI, Karlsson J. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using 157 Olsson et al. validated outcome measures. Am J Sports Med 2010: 38: 2186–2193. Nilsson-Helander K, Thomee R, Gravare-Silbernagel K, Thomee P, Faxen E, Eriksson BI, Karlsson J. The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med 2007: 35: 421–426. Olsson N, Nilsson-Helander K, Karlsson J, Eriksson BI, Thomee R, Faxen E, Silbernagel KG. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 2011: 19: 1385–1393. Rantanen J, Hurme T, Kalimo H. Calf muscle atrophy and Achilles tendon healing following experimental tendon division and surgery in rats. Comparison of postoperative immobilization of the muscle-tendon complex in relaxed and tensioned positions. Scand J Med Sci Sports 1999: 9: 57–61. Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int 2001: 22: 788–794. Saxena A, Ewen B, Maffulli N. Rehabilitation of the operated achilles tendon: parameters for predicting return 158 to activity. J Foot Ankle Surg 2011: 50: 37–40. Silbernagel KG, Nilsson-Helander K, Thomee R, Eriksson BI, Karlsson J. A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 2010: 18: 258–264. Silfverskiold KL, May EJ. Flexor tendon repair in zone II with a new suture technique and an early mobilization program combining passive and active flexion. J Hand Surg Am 1994: 19: 53–60. Suchak AA, Bostick GP, Beaupre LA, Durand DC, Jomha NM. The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg Am 2008: 90: 1876–1883. Suchak AA, Spooner C, Reid DC, Jomha NM. Postoperative rehabilitation protocols for Achilles tendon ruptures: a meta-analysis. Clin Orthop Relat Res 2006: 445: 216–221. Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med 2007: 35: 2033–2038. Uchiyama E, Nomura A, Takeda Y, Hiranuma K, Iwaso H. A modified operation for Achilles tendon ruptures. Am J Sports Med 2007: 35: 1739–1743. van Sterkenburg MN, Donley BG, van Dijk CN. Guidelines for sport resumtion. In: van Dijk CN, Karlsson J, Maffuli N, Thermann H, eds. Achilles tendon rupture, current concepts. Guildford: DJO Publications, 2008: 108–117. Weber M, Niemann M, Lanz R, Muller T. Nonoperative treatment of acute rupture of the achilles tendon: results of a new protocol and comparison with operative treatment. Am J Sports Med 2003: 31: 685–691. Westh E, Kongsgaard M, Bojsen-Moller J, Aagaard P, Hansen M, Kjaer M, Magnusson SP. Effect of habitual exercise on the structural and mechanical properties of human tendon, in vivo, in men and women. Scand J Med Sci Sports 2008: 18: 23–30. Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am 2010: 92: 2767–2775.