The Snapping Scapula: Diagnosis and Treatment Current Concepts
advertisement

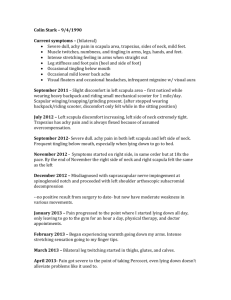
Current Concepts The Snapping Scapula: Diagnosis and Treatment LT Michael Kuhne, M.D., M.C., U.S.N., Nicole Boniquit, B.A., Neil Ghodadra, M.D., Anthony A. Romeo, M.D., and CDR Matthew T. Provencher, M.D., M.C., U.S.N. Abstract: As a largely under-recognized problem, snapping scapula stems from the disruption of normal mechanics in scapulothoracic articulation. It is especially common in the young, active patient population, and symptoms are frequently seen with overhead and throwing motions. Understanding the anatomy of the scapula and surrounding neurovascular structures is crucial in making a differential diagnosis and providing both nonoperative and surgical treatments. Common causes of snapping scapula include bursitis, muscle abnormality, and bony or soft-tissue abnormalities. Anatomic variations, such as excessive forward curvature of the superomedial border of the scapula, may also be a cause for snapping. Benign tumor conditions of the scapula can also predispose one to snapping scapula syndrome and should be thoroughly investigated during the course of treatment. Patients with snapping scapula syndrome typically present with a history of pain with overhead activities. Snapping scapula is associated with audible and palpable crepitus near the superomedial border of the scapula. Various imaging studies may be used to rule out soft-tissue and bony masses, which may cause impingement at the scapulothoracic articulation. In most cases nonoperative treatment is curative and includes physical therapy for scapular muscle strengthening and nonsteroidal anti-inflammatory medications. Corticosteroid injections may also be used for therapeutic and diagnostic purposes. In most cases overuse injuries and repetitive strains respond well to nonoperative treatments. When nonoperative measures fail, surgery is a proven modality, especially if a soft-tissue or bony mass is implicated. Both open and arthroscopic techniques have been described with predictable results. Key Words: Snapping scapula—Bony abnormality—Scapula— Superomedial bursitis—Bursitis. S napping scapula is a largely under-recognized problem. Patients present with palpable, audible, and painful crepitus of the scapula causing diminished From the Department of Orthopaedic Surgery, Naval Medical Center San Diego (M.K., M.T.P.), San Diego, California, and Department of Orthopaedic Surgery, Rush University Medical Center (N.B., N.G., A.A.R.), Chicago, Illinois, U.S.A. Dr. Romeo is supported by funding from Arthrex, Naples, FL. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or US Government. Address correspondence and reprint requests to CDR Matthew T. Provencher, M.D., M.C., U.S.N., Department of Orthopaedic Surgery, Naval Medical Center San Diego, 34800, Bob Wilson Dr, Suite 112 San Diego, CA 92134-1112, U.S.A. E-mail: mattprovencher@earthlink. net © 2009 by the Arthroscopy Association of North America 0749-8063/09/2511-8639$36.00/0 doi:10.1016/j.arthro.2008.12.022 1298 quality of life. Snapping scapula is most often caused by repetitive shoulder girdle stress and overhead arm use, although the differential diagnosis is quite extensive.1 The patient population is, therefore, normally a younger, active population. Although less common than other disorders of the shoulder, this disorder is a source of chronic pain and limited function for affected patients that oftentimes can be overlooked in the evaluation of those with upper extremity complaints.2 Although most of the patients are treated successfully with nonoperative measures, surgical intervention is a proven modality. ANATOMY An understanding of the anatomy and physiology of the scapulothoracic articulation is required to understand the pathogenesis of scapulothoracic disorders. Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 25, No 11 (November), 2009: pp 1298-1311 SNAPPING SCAPULA The scapula is a triangular-shaped bone articulating with the posterior thorax. It is attached to the axial skeleton by only the acromioclavicular joint, and therefore its stability is dependent on surrounding musculature.3 The periscapular musculature creates stability of the scapulothoracic articulation. The levator scapulae and rhomboids attach to the medial border of the scapula, whereas the subscapularis is on its anterior surface.1,4 The serratus anterior originates on the ribs and inserts on the medial scapular anterior surface. A cushion between the scapula and the thoracic wall is created by the serratus anterior and the subscapularis.5-8 Two spaces, the subscapularis space and the serratus anterior space, are created by the musculature of the joint. The serratus anterior space is located between the chest wall, serratus anterior, and rhomboids. The subscapularis space is bounded by the serratus anterior, subscapularis, and axilla.6,7,9,10 Three muscles of the rotator cuff originate at the scapula: the supraspinatus and the infraspinatus on the posterior surface of the scapula and the subscapularis on the anterior surface (Fig 1). There are several important neurovascular structures surrounding the scapula. The accessory nerve goes through the levator scapulae muscle near the superomedial angle of the scapula and runs along the medial scapular border deep to the trapezius muscle. The transverse cervical artery branches into the dorsal scapular artery (deep branch) and a superficial branch that travels with the accessory nerve. The dorsal scap- FIGURE 1. Superior view of cross-sectional anatomy showing the subscapularis and serratus anterior spaces, created by surrounding subscapularis and serratus anterior musculature. Their relation to the thoracic rib cage and overlying scapula should be noted. These spaces are important to distinguish because they may be sources of subscapular pain and “snapping.” 1299 FIGURE 2. Posterior view of scapular anatomy showing the relative location of key muscle attachments and nerve structures. The deep scapular musculature is reflected to delineate the attachment points of the muscles to the scapula. (n, nerve; a, artery.) ular artery travels with the dorsal scapular nerve 1 cm medial to the medial border of the scapula. They pierce the scalenus medius and travel deep to the rhomboid major and minor. The nerve innervates both of these structures. The long thoracic nerve is located on the surface of the serratus anterior. The suprascapular nerve and artery pass toward the suprascapular notch on the superior scapular border medial to the base of the coracoid (Fig 2).6,7,9,11 Several scapular bursae have been implicated in the development of scapular bursitis, which can lead to pain and snapping. Bursae are located in areas of friction and are potential spaces lined by a synovial membrane.1 Two major bursae are found consistently in patients: the infraserratus bursa located between the serratus anterior and the chest wall and the supraserratus bursa located between the subscapularis and serratus anterior.3,4,6,12-15 These can be noted on both dissection and arthroscopy (Fig 3).4 There are 4 minor bursa that are found inconsistently and are usually present as a response to abnormal scapulothoracic articulation mechanics. These minor bursae are located at the superomedial angle of the scapula and can be either inferior or superior to the serratus muscle. Another infraserratus bursa can be located at the inferior angle of the scapula, and the trapezoid bursa is located at the medial base of the spine under the trapezius.3,4,7,12-15 The bursa at the superomedial angle is the most common source of symptoms, with the 1300 M. KUHNE ET AL. FIGURE 3. Location of scapular bursal spaces in posterior (A) and superior (B) cross-sectional views. inferior angle as the second most common site for scapular bursitis.4,12,15 Pearls ● The dorsal scapular artery and nerve run along the medial border of the scapula. ● The suprascapular nerve passes through the scapular notch, and the suprascapular artery passes over the superior transverse scapular ligament. ● The 2 main bursa that become inflamed are the infraserratus and supraserratus. ● The main neurovascular structures near the scapula are the transverse cervical artery, dorsal scapular artery, suprascapular artery, dorsal scapular nerve, long thoracic nerve, suprascapular nerve, and accessory nerve. PATHOPHYSIOLOGY Snapping scapula occurs when the normal smooth gliding of the concave portion of the anterior scapula over the convex thorax is disrupted.6,9,16,17 The motion of the shoulder is a combined motion of both the scapula and the humerus to maximize joint stability and function by minimizing the load on the glenohumeral joint and the acromioclavicular joint.18-20 The scapula moves with motion of the arm to ensure proper positioning of the glenohumeral joint. The purpose of this positioning is to stabilize, absorb, and transfer forces that are generated by the articulating humerus. The glenohumeral joint must remain stable throughout its full range of motion for the rotator cuff muscles to adequately maintain joint integrity. Snap- ping scapula occurs predominantly with overhead and throwing motions. During the cocking phase of throwing, the scapula externally rotates (retraction). Then, in the acceleration phase, the scapula will internally rotate (protraction) and move anteriorly around the thoracic cage as the arm moves forward in followthrough. Superior elevation of the scapula also occurs during the cocking and acceleration phases. Scapular protraction, retraction, and superior elevation occur through action of the serratus anterior, trapezius, and rhomboid muscles to avoid impingement of the rotator cuff.21,22 The etiology of snapping scapula is divided into 3 major categories: bursitis, muscle abnormality, and bony or soft-tissue abnormality.5,6,12,17,23,24 Regardless of the etiology, the snapping occurs because of abnormal mechanics of the scapula grating on the underlying ribcage during arm movement with sound amplified by the thoracic cavity.1,4,5 Bursitis originates from a soft-tissue disorder, whereas crepitus is commonly from an osseous abnormality with grating or thumping of the scapula against the ribcage.4 The etiology of scapular bursitis is an overuse injury causing reactive bursa formation in a cycle of inflammation, reactive bursitis, and scarring. Repetitive motion of the scapula over the thorax irritates soft tissues and forms muscular microtears, causing chronic bursitis and inflammation. Resolution of the inflammation occurs in the form of scar tissue. Scarred periscapular musculature or bursa leads to impingement, pain, and further inflammation. The result is fibrosis of the bursa with secondary scarring, pain, and snapping.1,4,12 SNAPPING SCAPULA Another common cause of scapular snapping is muscular abnormality.25 The scapular stabilizer muscles function in an endurance capacity to position the glenohumeral fossa in the appropriate position for overhead activities. Atrophied muscle, fibrotic muscle, or anomalous muscle insertions, most commonly of the serratus anterior muscle, cause abnormal scapular movement, leading to snapping. Rhomboid and levator scapulae weakness, muscle trauma, or complications from shoulder surgery may be other causal factors.5,14,15,26 Arm elevation induces a posterior tilting of the scapula, thus compressing the space between the inferior pole and the ribcage.3 Tightness in the pectoralis minor, which attaches to the coracoid process, can pull forward on the scapula, causing an anterior tilt, decreasing the space between the superior scapula and the thoracic wall.21 Anatomically, there is less muscle mass on the medial border of the scapula where the subscapularis is thinnest, predisposing this location to rub against the ribcage.5-7,9,17,26 Bony and soft-tissue lesions, including scapular anatomic variation, osteochondroma, chondrosarcoma, or elastofibroma dorsi, comprise a less common group of causal factors. Anatomic variations are the most common subgroup and are caused by a hooked superomedial angle, Luschka’s tubercle, reactive spurs, or malunited rib fractures.1,3-5,7,9,14-17,24,25,27 Luschka’s tubercle is a prominence of bone or fibrocartilage at the superomedial angle of the scapula. Bone spurs occur from repetitive periscapular muscle avulsions.4,7,8,15 The most frequent deformity of the superomedial border is a bulbous top or anterior hook/angle rubbing across the ribs.28 The superomedial border and the inferior pole of the scapula have wide anatomic variability.27 When no obvious deformity is found, it is hypothesized that an excessive forward curvature of the superomedial corner of the scapula is the cause of the disorder.7-9 A bony projection at the inferior pole is present in 22% of the population, making it the second most common site for symptoms.27 Although the previously mentioned scapular anatomic variants increase the risk of snapping scapula, many persons with anatomic variations are asymptomatic. Conversely, other cases of snapping scapula have no visible anatomic cause.29 Any abnormal bone formation can cause a hot spot, leading to snapping, pain, and reactive soft-tissue changes.3,4,15,23,26 Osteochondroma of a rib or the anterior surface of the scapula is usually diagnosed in adolescence and early adulthood. Although it is the most common bony anomaly causing this disorder, it is a rare benign tumor. When present on the anterior scapular surface, 1301 it will invade into the scapulothoracic space, disrupting smooth motion.5,7,8,15,17,24,29-31 Scapular chondrosarcomas are infrequently the cause of snapping scapula. They are slightly more predominant in male patients and occur most frequently between 40 and 70 years of age. Surgical excision with wide margins is needed for curative treatment but is difficult because of the extensive neurovasculature around the scapula.32 Another infrequent cause of snapping scapula, elastofibroma dorsi, is a slow-growing, benign softtissue tumor. Seen more commonly in elderly women, it is located in the subscapular or infrascapular region on the chest wall at the level of the rhomboid major and latissimus dorsi muscles.33,34 It can also occur in athletes and is believed to form in response to repetitive microtrauma.3 Although it is firmly adherent to the costal wall, this connective tissue lesion elevates the inferior scapula.13,35 Pearls ● Bursitis is a reaction due to overuse or repetitive trauma of the articulation. ● Muscle weakness or changes can disrupt the articulation, causing crepitus or bursitis. ● Bony abnormalities include an angulated superomedial scapular angle, rib fractures, osteochondroma, Luschka’s tubercle, or reactive spurs. PATIENT PRESENTATION The patient will most commonly present to the physician with a history of pain during overhead activities, repetitive overuse of the shoulder, or even a single traumatic injury.3,4,9,11,12,14,15,36,37 Patients describe an audible and palpable crepitus with active shoulder movements, including shrugging of shoulders.9,38,39 There may be continuous grating of muscles, coarse thumping, a single snap, or intermittent clunks.25 Other descriptive terminology includes clicking, crunching, grating, or snapping sensations.1,11,40 These symptoms may result from participation in sports activities, including swimming and throwing, or from other rapid overhead arm movements.1,3,12,15,41 Pain may be severe enough to limit activities. Most often the location of the pain is at the superomedial angle or inferior pole of the scapula with variable amounts of cervical radiation.9,14,27 Symptoms will range from annoying to painful to disabling.4 On examination, the physician can feel crepitus, elicit tenderness to palpation, and hear the snapping in 1302 M. KUHNE ET AL. most patients. The patient most commonly will have tenderness to palpation at the superomedial border or inferior pole of the scapula.3,12 The patient can also present with tenderness to palpation located over the levator scapulae, trapezius, and/or rhomboid muscles. The patient will almost always have palpable crepitus with or without audible snapping.1,3,5,9 The crepitus is easily reproduced during arm movement because pain occurs most commonly with shoulder abduction. The crepitus may be accentuated when the superior angle of the scapula is being compressed against the chest wall during arm abduction.42 Pain is normally not reproducible with isometric movements.1,27,38,39 The pain and snapping may be decreased when the patient puts the hand of the affected shoulder on the opposite shoulder, thus lifting the scapula from the ribcage.5 It is important to assess scapular symmetry. The presence of winging or fullness may be the result of an underlying mass or space-occupying lesion. A mass does not always present with pseudo-winging of the scapula.4,43 The patient’s posture should also be assessed to rule out kyphosis.3 Palpable crepitus may have a familial tendency and can be bilateral in some patients.4,39 Scapular bursitis presents with fullness over the bursa.4 Pseudo-winging may be present as the patient compensates for pain.12,14 Palpation of the scapula during arm range of motion can pinpoint the location of bursitis.4 If the scapulothoracic bursa is inflamed, the pain will be deep to the levator scapulae and the superomedial angle of the scapula. Pain at the trapezoid bursa is rarer and more superficial, with pain over the junction of the spine and the medial border.14 Radiographic evaluation of the snapping scapula is important to rule out osseous deformity, tumors, or other bony causes of the patient’s pain. Plain radiographs should be the first study in the evaluation of the patient with scapular snapping. A lateral scapular view (also called the tangential or oblique view) in TABLE 1. Bony Pathology/Soft-Tissue Mass Osteochondroma Luschka’s tubercle Reactive bone spur Abnormal scapular superior angle curvature Rib fracture Elastofibroma Chondrosarcoma addition to anteroposterior and axillary views is obtained in the plane of the scapula.3-5,8,9,12,14,26,38 In patients with normal radiographs but suspected osseous lesions or fractures, a computed tomography (CT) or magnetic resonance imaging (MRI) scan should be obtained.12 A low threshold is necessary for obtaining MRI or CT scans because the anterior scapula is difficult to visualize with conventional radiographs. The usefulness of 3-dimensional CT scans versus conventional CT scans has been evaluated. Threedimensional CT can show the exact location of the snapping site and show superomedial scapular angulation, and it can be used to distinguish soft-tissue from bony incongruity and note the size of a deformity. This information is useful for noting the exact location for injection or surgical intervention. This modality is best used when conservative treatment fails and surgical intervention is a possibility.23,44 It is more sensitive than plain radiographs and regular CT scans.24,26 MRI is useful in the diagnosis of bursitis and soft-tissue masses, such as elastofibroma dorsi. Bursae on MRI show a well-demarcated cystic mass with high T1 and T2 signal intensity and are normally located between the serratus anterior and the lateral chest wall.4,13,33,45 The differential diagnosis includes several diagnoses that implicate the shoulder girdle (Table 1). Pearls ● Scapular motion causes noise or palpable crepitus. ● Pain is most common at the superomedial or inferior pole of scapula, especially with overhead activities. ● Radiographs or CT scans are usually normal. Three-dimensional CT reconstruction may show the snapping site. Differential Diagnosis Soft-Tissue Pathology Postural Causes Shoulder Girdle Bursitis Muscular weakness, atrophy, anatomic variation Scoliosis Kyphosis Glenohumeral pathology Periscapular muscle strain Winged scapula Neurogenic disorder SNAPPING SCAPULA INDICATIONS FOR NONOPERATIVE VERSUS OPERATIVE TREATMENT Despite the underlying cause of the diagnosis, a trial of nonoperative treatment is warranted. Given the high success rate of nonoperative interventions, they should be trialed for at least 6 months to 1 year before surgical intervention is considered.3 Snapping scapula responds to nonoperative treatment when caused by overuse and repetitive strain.12 However, if it is caused by an anatomic lesion that it is unlikely to benefit from nonoperative measures, a trial of nonoperative care is still warranted.4,12 When there is evidence of an anatomic or bony abnormality, excision has a high success of achieving permanent cure.4,5,15,17,23-25,33,40 Scapular crepitus can occur in approximately 30% of normal asymptomatic persons.3,4,15,17 Painless crepitus is more common than painful crepitus and does not usually need to be treated.36 However, a painful, clinically significant snapping may occur without sound or crepitus, and treatment is indicated, starting with nonoperative measures.14 Indications for surgery include failure of nonoperative measures. Surgery has an increased success rate if the patient responds to corticosteroid injections.4 Removal of the superomedial corner of the scapula even in patients in whom no bony abnormality is noted has been shown to be effective.9,16 The surgical candidate should be motivated, compliant, and have pain that significantly interferes with his or her quality of life.14 Contraindications to surgery include neck problems, other shoulder problems, neurologic deficits in the arms, or wasting of periscapular musculature.10 Both open and arthroscopic techniques have been described in the literature. The open surgical technique has an excellent track record, but concerns regarding the morbidity of the approach and cosmesis are important to discuss with the patient. The arthroscopic technique is more technically demanding, and the lack of bony landmarks can increase the risk of damage to neurovascular structures.36 Pearls ● A trial of nonoperative treatment is the mainstay of treatment. ● Bony anomalies or radiographic abnormalities respond well to surgical intervention with removal of the lesion. 1303 NONOPERATIVE TREATMENT Nonoperative management must focus on the scapular muscles and possible postural causes of abnormal scapulothoracic articulation.3,46 Because the major etiologic factors are overuse or improper joint mechanics, the patient must first modify activities and rest the joint to calm the cycle of bursitis and scarring. A course of nonsteroidal anti-inflammatory medications helps decrease inflammation.4,12 A trial of physiotherapy can be initiated to realign joint mechanics. If the patient is unable to undergo physical therapy and is continuing to have pain, then an injection of anesthetics and steroids is warranted.4,12,36,40 Ice, heat, and ultrasound treatments have been described with variable success.1,4 Muscular training and postural training are the most beneficial treatments. Postural training to minimize kyphosis, promote upright posture, and strengthen upper thoracic musculature is indicated for cases in which posture is the proposed causal factor. A figure-of-8 harness may assist in postural training.4,12,14,15,26,47 Because the scapula is responsible for static stability of the shoulder girdle, endurance training is the key for scapular stability. This type of training necessitates low-intensity, high-repetition exercises. Strengthening of the subscapularis and serratus anterior helps achieve successful results because a weak serratus anterior muscle may allow the scapula to tilt forward, causing crepitus.3,12,14,48,49 Scapular adduction and postural shoulder shrug exercises are of the utmost importance because they strengthen the scapular stabilizers, including the serratus anterior, rhomboids, and levator scapulae (Fig 4).7,16,17 Abduction and elevation of the scapula cause increased pressure and strain on the underlying musculature and should be avoided.3 If nonsteroidal anti-inflammatory drugs and physical therapy are unable to control the pain, scapular injection is a useful tool.15,17 The injection is given with a 1.5-inch 22- to 25-gauge needle. The patient lies prone with the arm in a chicken-wing position with the hand behind the back. This places the shoulder in a position of extension, internal rotation, and adduction. After a sterile environment is obtained, the needle is inserted parallel to the anterior border of the scapula, with care taken not to penetrate too deeply causing a pneumothorax. For pain at the inferior angle of the scapula, the needle is inserted on the inferiormedial border of the scapula aimed laterally. For the superomedial bursa, the needle should be angled 45° 1304 M. KUHNE ET AL. FIGURE 4. (A-C) Various scapular on and scapular protraction exercises. laterally in a cephalad to caudad direction, entering just off the superior-medial tip of the scapula (Fig 5).3,7 The maximum frequency of corticosteroid injec- tions is usually 3 to 4 times per year.4 By combining a local anesthetic agent with the steroid, injection is both diagnostic and therapeutic. If there is pain relief, SNAPPING SCAPULA 1305 OPERATIVE TREATMENT Relevant Anatomy Anatomic structures are at risk of injury during operative intervention of snapping scapula and include the long thoracic nerve, dorsal scapular artery, suprascapular nerve, axillary contents, and thoracic cavity.4 Knowledge of their location and avoidance of these structures decreases surgical complications. Before the incision is made, a skin marker may be used to identify the inferior and superomedial corners of the scapula, the medial border, the scapular spine, and the acromion.16,36 Surgical incision, bony resection, and placement of arthroscopic portals must be precise to avoid neurovascular structures. In the arthroscopic technique, 2 portals are placed on the medial border of the scapula approximately 3 to 4 cm medial to the vertebral border of the scapula and below the level of the scapular spine to avoid injury to the dorsal scapular nerve and artery and the accessory nerve.6,10-12,16,40,43,50 Placement of a third, superior portal must be methodical because of the presence of multiple neurovascular structures, including the accessory nerve, the suprascapular nerve, the dorsal scapular nerve, and the transverse cervical artery, coursing nearby.11,12 Both open and arthroscopic procedures must avoid the accessory and long thoracic nerves medially.36 Instrument orientation or bony resection either superiorly or laterally toward the coracoid process must avoid the suprascapular nerve and artery located in the suprascapular notch.4,27 FIGURE 5. The 2 common locations of scapular bursal injections are at the superomedial border and at the inferior tip. there is a high likelihood that scapular bursitis or crepitus is the cause of the patient’s pain.1 Pearls ● Initial activity modification, nonsteroidal anti-inflammatory drugs, and physical therapy are the main components of a successful treatment approach. ● Physical therapy should focus on strengthening the subscapularis and serratus anterior. ● Corticosteroid and anesthetic injection is a good predictor of successful outcomes with either nonoperative or surgical intervention. Open Surgical Approach and Technique Partial scapulectomy is an option for treating symptomatic snapping scapula resistant to nonoperative treatment.4,15 Not all cases require excision of the superomedial section of the scapula. In studies in which bursectomy alone was performed, excellent results were obtained.2,51 However, resection of the superomedial border more consistently produces successful results and is the more commonly used method.36,52 Open bursectomy can be performed either at the superomedial angle or at the inferior pole, the 2 most common locations for scapulothoracic bursitis.12 Localization of the snapping or pain determines the site for resection.25 Surgery on the inferior bursa is approached through an oblique incision distal to the inferior angle of the scapula. The surgeon will split the trapezius and latissimus dorsi in line with the muscle 1306 M. KUHNE ET AL. fibers to expose the bursa. Excision of the bursa with removal of any osteophytes on the scapula is performed. The wound is then closed over a drain.4 For superomedial bursitis, a vertical incision medial to the medial border of the scapula is made. The trapezius is dissected free and retracted cranially from the scapular spine, followed by dissection of the levator scapulae, subscapularis, and supraspinatus, which are retracted proximally through subperiosteal dissection.4,9 The bursa can then be resected and any osteophytes removed.4 The procedure ends with reapproximation of the periscapular muscles. Bony resection can improve surgical results.36 When no obvious bony lesion is noted, removal of the medial 2 cm of the scapula allows a more natural articulation of the scapulothoracic joint when the muscles are reattached.29 The medial scapular border contains the origin of the subscapularis, supraspinatus, infraspinatus, serratus anterior, rhomboid, and levator scapulae muscles. Their disruption with resection of the entire medial border of the scapula can lead to significant postoperative disability.26,28 More recently, snapping scapula has been treated successfully with excision of just the superomedial border of the scapula, avoiding the negative outcomes.9,12,15 To perform the superomedial scapular resection, the patient is placed in the prone position, and an incision over the medial scapular spine is made with dissection through the soft tissue to expose the scapular spine.4,15 The periosteum is incised with subperiosteal elevation of the medial periscapular muscles, including the supraspinatus, subscapularis, rhomboid, and levator scapulae, which are retracted proximally.4,9,12,48 The trapezius is retracted cranially.9,15 The superomedial angle of the scapula is resected with an oscillating saw in the shape of an equilateral triangle extending to the medial base of the scapular spine.4,15,48 Elevated muscles are reapproximated to the spine of the scapula by suturing them to the bone by use of drill holes.4,12,53 The affected arm is mobilized during surgery to confirm relief of the snapping. The wound is closed over a drain (Fig 6).9 Pearls ● Surgical treatment is reserved for patients with painful, audible, and palpable crepitus not responding to nonoperative treatment.36 ● Severe winging is a contraindication to surgical resection of the superomedial scapula.36 Arthroscopic Approach and Technique Arthroscopic treatment of snapping scapula is an alternative that decreases the morbidity of the open technique caused by muscle takedown. Cosmesis and earlier rehabilitation with earlier return to full function are other benefits.10,12,43,54 It is an effective and safe procedure for bursectomy and resection of the superomedial corner of bone.50 Arthroscopic procedures were first described using 2 portals placed 3 cm medial to the scapula, but because of visibility limitations, the procedure evolved to the more common recent practice of using a third, superior portal. Some surgeons prefer to first perform a shoulder arthroscopy to exclude other causes of shoulder pain. Once this has been done, the surgeon focuses on the scapulothoracic articulation. A sterile stockinet is placed around the arm. The patient is placed in the prone position with the arm in a chicken-wing position by use of internal rotation. This allows for easier access to the articulation because this causes scapular winging.10,11,14,16,36,55 A spinal needle may be placed at the superomedial corner of the scapula to assist in orientation.14,36 One of the medial portals is a viewing portal at the level of the spine, and the other is a working portal inferior to the spine of the scapula.10-12,16,40,50 The introducer is passed through the skin, subcutaneous tissue, and trapezius; then between the rhomboid minor and rhomboid major at the level of the spine of the scapula; and finally, into the serratus anterior space. Entry to the subscapularis space can be made by penetration of the serratus anterior muscle. The potential pitfalls include overpenetration through the chest wall, causing pneumothorax, or penetration through the serratus anterior into the axillary space.6,10,12,56 A third, superiorly located portal allows easier access for resection of the superomedial angle of the scapula.36 To create this portal, instrumentation is passed between the scapula and the thoracic cage and directed caudal and medially. The portal is located one third of the distance from the medial scapular border between the superior medial angle of the scapula and the lateral border of the acromion to avoid neurovascular structures.11,16,36 When instrumentation is passed to locate the third portal, care must be taken to remain close to the ventral surface of the scapula to avoid penetration of the thoracic cavity (Fig 7).11,16,36 Once portal placement is complete, the portal 3 cm medial to the scapular spine is used as the viewing portal with a 4.5-mm 30° arthroscope.10,12,36 Fluid SNAPPING SCAPULA 1307 FIGURE 6. Open surgical approach for treatment of snapping scapula. (A) The patient is positioned prone, and the incision is made on the medial border of the scapula, ensuring that the dorsal scapular nerve is protected. The trapezius and deltoid are identified along the scapular spine (B) and retracted to see the periscapular muscles (C). (D) The levator scapulae and rhomboid are tagged and subperiosteally elevated off the superomedial scapula border. 1308 M. KUHNE ET AL. FIGURE 6. (Continued). (E) Approximately 1.5 cm of superomedial scapula bone is resected with a small oscillating saw and the bursa just deep to the bone debrided. (F) Bone tunnels are drilled (1.5 mm) into the scapula to securely repair the levator scapulae and rhomboid with No. 2 nonabsorbable suture. (G) Final repair. pressure is introduced into the scapulothoracic space to 50 mm Hg.40 The intercostal muscles and ribs should be visualized inferiorly, the subscapularis laterally, and the rhomboids medially.14 A bipolar radiofrequency device is used to minimize bleeding.12 Resection of thin areolar tissue and fibrous bands with the shaver creates a view of the subscapular bursa. The thoracic surface of the superomedial scapula can be identified by use of direct palpation and scapular movement.10,40 Any fibrous adhesions that are encountered in the bursa between the subscapularis and serratus anterior and in the bursa between the serratus anterior and the chest wall should be debrided.4,55 Soft-tissue and bursal tissue from the deep surface of the superomedial corner of the scapula is removed with the shaver.16,36,57 Radiofrequency ablation is useful to skeletonize the bone.14 Once bursectomy is complete, the superomedial corner of the scapula is resected. Meniscal and notchplasty burs are used to excise a triangular section of the superomedial part of the scapula.10,16,36 To avoid the suprascapular nerve, the surgeon should mark a point on the medial border of the scapula halfway between the scapular spine and the inferior pole. The shaver is passed through the superior portal and directed no more lateral than toward that point and no more distal than the scapular spine, creating a 2.5-cm buffer to protect this nerve.36 Before removing the arthroscope, the surgeon should ensure that there is full clearance of the scapula without impingement.10,40 Pearls ● A 3-portal approach with care and preplanning avoids neurovascular structures. ● Arthroscopic technique affords better cosmesis, decreased morbidity, and a more rapid return to full function than the open procedure. ● Two of the portals should be placed 3 cm medial to the medial scapular border and caudal to the spine of the scapula to avoid injury to the dorsal scapular nerve and artery. POSTOPERATIVE REHABILITATION The course for postoperative physical therapy depends on whether the surgical technique was open or arthroscopic. Arthroscopic surgery, with less muscle disruption, allows a more rapid course of physical rehabilitation with earlier return to full activities. After open bursectomy on the inferior scapular bursa, physical therapy is begun at 1 week. Because of the increased dissection for superomedial bursectomy, a longer postoperative course is needed. Passive motion and pendulum exercises can begin immediately with a sling for comfort. Physical therapy continues with active motion between 3 and 8 weeks and strength training at 12 weeks.4,15 The open superomedial scapular resection postoperative course is of longer duration. A splint is placed for 3 weeks.9 Rehabilitation is started with early passive motion and then active motion at 4 weeks, fol- SNAPPING SCAPULA 1309 FIGURE 7. (A) For arthroscopic resection, the patient is placed prone and the medial border of the scapula is elevated off the thorax by internally rotating the arm up the back. (B) The arthroscopic portals are approximately 3 cm medial to the most medial edge of the scapula to avoid injuring the dorsal scapular and spinal accessory nerves. (C) An additional portal may be made superiorly in the medial one third of the scapula coming from superior to inferior to assist with access to the superomedial scapular border. (n, nerve.) lowed by strengthening at 8 to 12 weeks.12 Resistance exercises can then be started at 12 weeks.4 After arthroscopy, the patient uses a sling for 24 to 48 hours and then begins both passive and active physiotherapy focused on thoracic posture, scapular control, and rhomboid strengthening.10,36,40 Full active motion with the arthroscopic technique is expected by 1 week.16,36 In one study all patients reported a reduction in pain and snapping at 6 weeks postoperatively.40 Full recovery can be expected by 2 to 4 weeks postoperatively.36 Even if a full recovery has occurred, the return to sports and overhead activities should not occur until 2 or 3 months postoperatively.10,16,36 Pearls ● After arthroscopy, a full recovery is expected by 2 to 4 weeks with return to sports by 2 to 3 months. ● After an open procedure, longer physical therapy and rehabilitation regimens are necessary because of the extent of surgical dissection. ● Physical therapy begins with passive motion, fol- 1310 M. KUHNE ET AL. lowed by active motion and then strengthening exercises. OUTCOMES The literature supports nonoperative treatment as the initial treatment for patients with snapping scapula. Approximately 50% of patients, with the rate being as high as 80% in some studies, had relief of symptoms with nonoperative treatment.5,9,55 When this fails, surgical interventions have a high success rate. In one study 50% of the patients who underwent open surgical resection had relief of symptoms at 1 year.5 Other studies showed a higher success rate. One study showed that 12 of 14 patients had relief of pain and snapping at a mean of 42 months after surgery,48 and another had an 88% success rate.4 In these studies no gross anatomic abnormalities of the resected portion of the scapula were noted. Another study described 5 patients who underwent surgery, all of whom returned to normal activities, although 1 reported incomplete resolution of symptoms.9 Three patients with osteochondroma underwent surgical excision, all with good results. In a study using the arthroscopic approach with 2 portals, the authors reported that 95% of patients would undergo the procedure again and 22 of 23 patients had good or excellent results.51 Among the 23 patients, there were no surgical complications. All patients were able to return to their previous activities. In studies involving the arthroscopic approach with the third portal, the procedure was found to be safe and successful. No intraoperative or postoperative complications were found with this surgical approach. Although the studied patient population remains small, the results are promising. Among 26 patients, all with normal radiographs before surgery, only 1 had symptoms that were not improved after surgery. However, all patients reported that the procedure was worthwhile. Although their pain was resolved, 25% of the patients continued to have mild crepitus with occasional clicking.16,36,58 In one study of 10 patients, only 1 patient remained unable to return to work duties and 7 returned to their sporting activities.16 CONCLUSIONS Snapping scapula is caused by a disruption in the normal mechanics of the scapulothoracic articulation. Once neurogenic disorders and disorders of the acromioclavicular and glenohumeral joints are excluded, the etiology of the crepitus must be determined through history, physical examination, and radiologic studies. If there is an obvious anatomic cause for the snapping, nonoperative treatment should be trialed with likely progression to surgical excision of the abnormality. If no anatomic lesions are noted, conservative treatments should be trialed first, but if unsuccessful, both open and arthroscopic procedures for excision of the superomedial scapular border have been proven to provide relief of these patients’ symptoms. REFERENCES 1. Percy EC, Birbrager D, Pitt MJ. Snapping scapula: A review of the literature and presentation of 14 patients. Can J Surg 1988;31:248-250. 2. McCluskey GM, Bigliani I, Bigliani LU. Surgical management of refractory scapulothoracic bursitis. Orthop Trans 1991;15: 801. 3. Manske RC, Reiman MP. Nonoperative and operative management of snapping scapula. Am J Sports Med 2004;32:15541565. 4. Kuhn JE, Plancher KD, Hawkins RJ. Symptomatic scapulothoracic crepitus and bursitis. J Am Acad Orthop Surg 1998; 6:267-273. 5. Carlson HL, Haig AJ, Stewart DC. Snapping scapula syndrome: Three case reports and an analysis of the literature. Arch Phys Med Rehabil 1997;78:506-511. 6. Ruland LJ III, Ruland CM, Matthews LS. Scapulothoracic anatomy for the arthroscopist. Arthroscopy 1995;11:52-56. 7. Butters KP. The scapula. In: Rockwood C, Matsen F, eds. The shoulder. Ed 2. Philadelphia: WB Saunders, 1998:335-352. 8. Parsons TA. The snapping scapula and subscapular exostoses. J Bone Joint Surg Br 1973;55:345-349. 9. Lesprit E, Le Huec JC, Moinard M, Schaeverbeke T, Chauveaux D. Snapping scapula syndrome: Conservative and surgical treatment. Eur J Orthop Surg Traumatol 2001;11:51-54. 10. Harper GD, McIlroy S, Bayley JI, Calvert PT. Arthroscopic partial resection of the scapula for snapping scapula: A new technique. J Shoulder Elbow Surg 1999;8:53-57. 11. Chan BK, Chakrabarti AJ, Bell SN. An alternative portal for scapulothoracic arthroscopy. J Shoulder Elbow Surg 2002;11: 235-238. 12. O’Holleran JD, Millett PJ, Warner JJP. Arthroscopic management of scapulothoracic disorders. In: Miller MD, Cole BD, eds. Textbook of arthroscopy. Ed 3. Philadelphia: Saunders, 2004:277-287. 13. Huang CC, Ko SF, Ng SH, Lin CC, Huang HY, Yu PC, Lee TY. Scapulothoracic bursitis of the chest wall: Sonographic features with pathologic correlation. J Ultrasound Med 2005; 24:1437-1440. 14. Millett PJ, Pacheco IH, Gobezie R, Warner JJP. Management of recalcitrant scapulothoracic bursitis: Endoscopic scapulothoracic bursectomy and scapuloplasty. Tech Shoulder Elbow Surg 2006;7:200-205. 15. Kuhn, JE. In: Iannotti JP, Williams GR, eds. The scapulothoracic articulation: Anatomy, biomechanics, pathophysiology and management. Philadelphia: Lippincott Williams & Wilkins, 1999:817-845. 16. Pavlik A, Ang K, Coghlan J, Bell S. Arthroscopic treatment of painful snapping of the scapula by using a new superior portal. Arthroscopy 2003;19:608-612. 17. Safran MR. Management of scapulothoracic problems. Curr Opin Orthop 1997;8:67-74. 18. Dome DC, Kibler WB. Evaluation and management of scapulothoracic disorders. Curr Opin Orthop 2006;17:321-324. SNAPPING SCAPULA 19. Bourne DA, Choo AM, Regan WD, MacIntyre DL, Oxland TR. Three-dimensional rotation of the scapula during functional movements: An in vivo study in healthy volunteers. J Shoulder Elbow Surg 2007;16:150-162. 20. Sheikhzadeh A, Yoon J, Pinto VJ, Kwon YW. Three-dimensional motion of the scapula and shoulder during activities of daily living. J Shoulder Elbow Surg 2008;17:936-942. 21. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg 2003;11:142-151. 22. Cutti AG, Giovanardi A, Garofalo P, Rocchi L, Davalli A. Shoulder and elbow motion analysis through wearable sensors: Part 2: Preliminary validation of the anatomical systems of reference. Gait Posture 2008;28:S28 (abstr). 23. Takahara K, Uchiyama S, Nakagawa H, Kamimura M, Ohashi M, Miyasaka T. Snapping scapula syndrome due to malunion of rib fractures: A case report. J Shoulder Elbow Surg 2004; 13:95-98. 24. Oizumi N, Suenaga N, Minami A. Snapping scapula caused by abnormal angulation of the superior angle of the scapula. J Shoulder Elbow Surg 2004;13:115-118. 25. Milch H. Partial scapulectomy for snapping of the scapula. J Bone Joint Surg Am 1950;32:561-566. 26. Mozes G, Bickels J, Ovadia D, Dekel S. The use of threedimensional computed tomography in evaluating snapping scapula syndrome. Orthopedics 1999;22:1029-1033. 27. Edelson JG. Variations in the anatomy of the scapula with reference to the snapping scapula. Clin Orthop Relat Res 1996:111-115. 28. Alvik I. Snapping scapula and Sprengel’s deformity. Acta Orthop Scand 1959;29:10-15. 29. Cameron HU. Snapping scapulae: A report of three cases. Eur J Rheumatol Inflamm 1984;7:66-67. 30. Van Riet RP, Van Glabbeek F. Arthroscopic resection of a symptomatic snapping subscapular osteochondroma. Acta Orthop Belg 2007;73:252-254. 31. Marcos J, Rodríguez Russo P, Lima S, Rodríguez EL. Elastofibroma dorsi: An unusual case of a subscapular nodular mass. J Clin Rheumatol 2004;10:21-24. 32. Schneiderbauer MM, Blanchard C, Gullerud R, et al. Scapular chondrosarcomas have high rates of local recurrence and metastasis. Clin Orthop Relat Res 2004:232-238. 33. Majó J, Gracia I, Doncel A, Valera M, Núñez A, Guix M. Elastofibroma dorsi as a cause of shoulder pain or snapping scapula. Clin Orthop Relat Res 2001:200-204. 34. Moss ALH. Elastofibroma dorsi: A rare diagnosis in chest wall tumours. J Plast Reconstr Aesthet Surg 2008;61:585-586. 35. Daigeler A, Vogt PM, Busch K, et al. Elastofibroma dorsi— Differential diagnosis in chest wall tumours. World J Surg Oncol 2007;5:15. 36. VanRiet RP, Bell SN. Scapulothoracic arthroscopy. Tech Shoulder Elbow Surg 2006;7:143-146. 37. Lintner D, Noonan TJ, Kibler WB. Injury patterns and biomechanics of the athlete’s shoulder. Clin Sports Med 2008;27: 527-551. 38. Kouvalchouk JF. Subscapular crepitus. Orthop Trans 1985;9: 587-588. 1311 39. Cobey MC. The rolling scapula. Clin Orthop Relat Res 1968; 60:193-194. 40. Pearse EO, Bruguera J, Massoud SN, Sforza G, Copeland SA, Levy O. Arthroscopic management of the painful snapping scapula. Arthroscopy 2006;22:755-761. 41. McFarland EG, Tanaka MJ, Papp DF. Examination of the shoulder in the overhead and throwing athlete. Clin Sports Med 2008;27:553-578. 42. Milch H. Partial scapulectomy for snapping of the scapula. J Bone Joint Surg Am 1962;44:1696-1697. 43. Fukunaga S, Futani H, Yoshiya S. Endoscopically assisted resection of a scapular osteochondroma causing snapping scapula syndrome. World J Surg Oncol 2007;5:37. 44. de Haart M, van der Linden ES, de Vet HC, Arens H, Snoep G. The value of computed tomography in the diagnosis of grating scapula. Skeletal Radiol 1994;23:357-359. 45. Ken O, Hatori M, Kokubun S. The MRI features and treatment of scapulothoracic bursitis: Report of four cases. Ups J Med Sci 2004;109:57-64. 46. Tripp BL. Principles of restoring function and sensorimotor control in patients with shoulder dysfunction. Clin Sports Med 2008;27:507-519. 47. Neviaser RJ. Painful conditions affecting the shoulder. Clin Orthop Relat Res 1983:63-69. 48. Arntz CT, Matsen FA. Partial scapulectomy for disabling scapulothoracic snapping. Orthop Trans 1990;14:252-253. 49. Lehman GJ, Gilas D, Patel U. An unstable support surface does not increase scapulothoracic stabilizing muscle activity during push up and push up plus exercises. Man Ther 2008; 13:500-506. 50. Cole D, Ginn TA, Smith A, Poehling GG. Scapulothoracic arthroscopy: Indications, review of literature, and report of 24 patients. Arthroscopy 2006;22:e8-e9. Available online at www. arthroscopyjournal.org. 51. Lehtinen JT, Tetreault P, Warner JJP. Arthroscopic management of painful and stiff scapulothoracic articulation. Arthroscopy 2003;19:28e. 52. Nijs J, Roussel N, Struyf F, Mottram S, Meeusen R. Clinical assessment of scapular positioning in patients with shoulder pain: State of the art. J Manipulative Physiol Ther 2007;30: 69-75. 53. Lehtinen JT, Macy JC, Cassinelli E, Warner JJ. The painful scapulothoracic articulation: Surgical management. Clin Orthop Relat Res 2004:99-105. 54. Bell S, Pavlik A. Paper #216 arthroscopic treatment of painful snapping of the scapula. Arthroscopy 2003;19:109-110 (abstr). 55. Ciullo JV. Subscapular bursitis: Treatment of “snapping scapula” or “washboard syndrome.” Arthroscopy 1992;8:412-413. 56. Bell SN, Van Riet RP. Safe zone for arthroscopic resection of the superomedial scapular border in the treatment of snapping scapula syndrome. J Shoulder Elbow Surg 2008;17:647-649. 57. Lien S, Shen P, Lee C, Lin L. The effect of endoscopic bursectomy with mini-open partial scapulectomy on snapping scapula syndrome. J Surg Res 2008;150:236-242. 58. Horman D, Pavlic A, Bell S. Arthroscopic treatment of painful snapping of the scapula. J Bone Joint Surg Br 2002;84:271 (Suppl III, abstr).