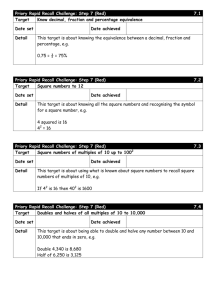
Q UA L I T Y A C... 2 0 1 2 -1 3 QUALITY
advertisement

PRIORY HEALTHCARE QUA L IT Y ACC O U NT 2012 -1 3 PROVIDING QUALITY INSPIRING INNOVATION DELIVERING VALUE Introduction and background The Priory Group of Companies is the UK's leading provider of mental healthcare and specialist education services. We work in partnership with our service users and their families, as well as commissioners, regulators and other stakeholders, to provide the best possible outcomes at every stage of an individual's care pathway. By providing a seamless transition for service users as they progress between higher and lower dependency services, we ensure continuity of care that underpins the delivery of successful outcomes*. Priory Pathways are our range of services that provide accessible expertise appropriate to each service user as part of their personalised care pathway. This integrated approach to treatment supports the service user's progression by providing sustainable placements and, where appropriate, reintegration back into a community setting. P A T H W A Y S Behavioural, emotional and social difficulties Acute mental health Addictions Eating disorders Child and adolescent mental health Secure Complex care Autism including Asperger’s syndrome Positive Behaviour Support Community and domiciliary options (‘Supporting You’) re Our integrated approach to treatment Ca Hea lt m Edu c oo or e Autism are c h eg Learning disabilities Fostering C ra Mental health Specialist further education ion at Neuro-disabilities Learning disabilities Autism including Asperger’s syndrome r Am Residential care Nursing care Dementia care Day care Respite care Re-ablement and convalescence care End of life care * Priory Healthcare satisfaction results based on opinion surveys completed during 2012-13. All service users' quotes within this Quality Account have been retrieved from anonymous comments within these surveys. Clinical outcomes based on standard metrics used across all Priory hospitals, 2012-13. All commissioner quotes are their own. Detailed information on the scope of data inclusion in relation to the outcomes highlighted in this Quality Account are outlined in the appendix, from page 43. 2 External review by PricewaterhouseCoopers In 2012, the Priory Group commissioned an external review of the Group’s quality assurance and governance processes, performed by PricewaterhouseCoopers (PwC). The findings from the review were largely positive, and our aim is to continue to develop market leading practices to ensure that all Priory sites maintain their high quality standard of service. Seven key senior positions have since been created, including a Director of Corporate Assurance and Chief Nursing Officer, who has led the improvements in safety, quality and compliance, with a Director for each of the three functions to ensure effective delivery. Heads of Quality for each division within the Group have also been appointed, to take divisional responsibility for proactively driving improvements in quality; ensuring quality indicators, care standards and regulatory requirements are fully satisfied. • the implementation of a quality dashboard, which contains information on key quality performance indicators, that can be interrogated down to site level. This allows the Quality team to adopt an overarching view of quality across the organisation, and can also drill down to divisional, regional and site level information if required. Divisional management teams are also able to access the information on the dashboard to enable them to work closely with sites where potential issues are highlighted PricewaterhouseCoopers will return in 2013-14 to review the changes that have been made and present their findings to the Quality Assurance Committee. A Quality Review Project Board was formed during the year to ensure delivery of the planned improvements in 2012-13. In addition, a Quality Assurance Committee was established, which reports to the Board on all matters relating to safety, quality and compliance. The Quality Assurance Committee is chaired by a Non-Executive Director. Key achievements and improvements to date include: • strengthening the risk register process to ensure risks are identified at site level, with mitigating action taken when required. Divisional risk registers feed into the Group Risk Register and ultimately the Board Assurance Framework • the introduction of an e-compliance system, along with a strengthened internal team of compliance inspectors. Separate tools have been developed to cover all Priory Group services as well as the different regulatory bodies (a total of 23 tools). There is a proactive internal programme of inspections, which enable any issues to be picked up immediately, with actions put in place to resolve them. Action plans are monitored by the divisional Heads of Quality 3 Providing Inspiring Delivering 4 4 Contents Part 1 – Statement from the Chief Executive Statement from the Chief Executive 7 Quality statement from the Director of Corporate Assurance and Chief Nursing Officer Overview of the Priory Healthcare division 9 10 Part 2 – Performance against objectives Performance against 2012-13 objectives 12 Detailed review of performance against 2012-13 objectives 14 Part 3 – Priorities for improvement Priorities for improvement 2013-14 16 Part 4 – Additional information Service user satisfaction – delivering value through clinical excellence 18 Outcomes – the success of our service users 20 Investing in staff, education and training 22 Regulatory compliance 25 Focus sites during 2012-13 27 Working in partnership with our commissioners and regulators 28 Improving safety for our service users 29 Continuous improvement in the delivery of our services 30 Part 5 – Appendix Statement of assurance from our lead commissioner 32 Statement of directors' responsibilities in respect of the Quality Account 33 Independent auditor’s limited assurance report 34 Format of this Quality Account 37 Glossary of terms 39 Commissioning for Quality and Innovation framework 40 Scope of data inclusion 43 5 Our promise PROVIDING QUALITY Quality is not only applied to the care and services we deliver, it also stretches across our staff and facilities, ensuring optimum standards of delivery in the appropriate surroundings. What quality means to us: • • • • • Consistent delivery of care and education at the highest level Safe, effective and regulated services Listening to our service users The highest calibre of staff Investing in our facilities INSPIRING INNOVATION As a service provider, we are always looking for new ways to do things better. Innovation can be in the form of a new idea or by simply being innovative with an existing one. What innovation means to us: • • • • Constantly reviewing the way we work to ensure we continually develop best practice Not accepting the status quo if things could be improved Being at the forefront of treatment and care-led trends and solutions Creating unique and market leading practices DELIVERING VALUE We offer the best quality individualised programmes at competitive prices, tailored to specific treatment goals. These programmes offer flexibility as well as the ability to reduce costs throughout treatment. What value means to us: • • • • 6 Tailored and cost effective treatment Remaining highly competitive in the market Transparent and flexible pricing models Regular pricing reviews Part 1 – Statement from the Chief Executive Welcome to our third Healthcare Quality Account, my first as Chief Executive Officer of the Group, which provides a summary of the achievements of our Healthcare division during 2012-13 and outlines our priorities for quality improvement during 2013-14. mental health service where 97% of service users rated the overall quality of their therapy treatment as good or excellent and in our complex care service where 99% of service users wholly or partially achieved all of their treatment goals. All of us at the Priory Group are passionate about the quality of service that we provide to all of those entrusted into our care. Over the course of the last 12 months we have made significant further improvements in performance against key quality measures and, at the date of writing this report, I am pleased to announce that we have no embargoes in place across the Healthcare division from any of our regulators. In our addictions and eating disorders services, 99% and 98% of service users respectively, said they were treated with respect and dignity and 95% of service users from our child and adolescent mental health services (CAMHS) were satisfied with the care and treatment they received. 96% of outcomes inspected by our regulators were met Thanks to the hard work of our staff, we have successfully delivered against the quality priorities we set ourselves in our 2011-12 Quality Account as well as achieving our Commissioning for Quality and Innovation (CQUIN) targets for the year. Providing innovative treatments across our service lines is key to the success of the business; as such, we are working on developing integrated care pathways that cross our divisions to ensure we can offer a complete package of care to service users throughout the key stages of their lives, from inpatient care to supported living and then out into the community. Our ultimate goal is to provide excellence in mental healthcare across the communities we serve. We have a hugely dedicated, professional workforce, who continue to deliver care to an excellent standard. The commissioning landscape has changed significantly over recent months and it is my aim to successfully navigate the Group through the evolving environment, ensuring that the wellbeing of service users and the health of our organisation is protected and the highest quality standards are upheld. I work closely with the Healthcare division’s senior management team and, to the best of my knowledge, the information contained in this report is a true and accurate reflection of the services and outcomes that we have delivered. Tom Riall Chief Executive Officer June 2013 Our focus is always on service user safety, clinical effectiveness and the service user experience. Achievement of these goals is clearly demonstrated within the acute Our ultimate goal is to provide excellence in mental healthcare across the communities we serve 7 Highlights from this year’s Quality Account What our service users think 94% of our younger service users felt that their healthcare professionals listened to and understood their problems 90% of service users within complex care services said they were treated with dignity and respect 98% of service users within addiction services were satisfied with their overall quality of care What our staff think 8 90% of our staff feel that service users are given choice and flexibility regarding their care 89% of our staff feel that they are able to contribute to the success of their team 90% of our staff feel motivated to go the extra mile for the people they care for Quality statement from the Director of Corporate Assurance and Chief Nursing Officer The Priory Group ensures that our clinical teams are supported by an arms-length Corporate Assurance function, which has been made possible by the significant investment in this area that was made during 2012. This ensures that our services are safe and effectively regulated and enhances the effectiveness of services and care provided. Achieving positive outcomes, coupled with the experience of our service users and staff, defines the quality of our service and is at the heart of everything we do. This approach is also reflective of the national agenda for quality. Our priorities for driving quality within the Priory Group are to: • exceed national standards of care • improve outcomes for both our adult and adolescent service users • deliver safe and secure services • ensure a positive experience of care from all who use our services In addition, we will continue to invest in our staff through education and training, which ensures that the high levels of care that we expect are delivered. variations from England, Scotland, Wales and Northern Ireland. This not only helps us to satisfy our regulatory bodies, but also enables us to produce policies and procedures that are relevant and aimed at providing the highest standard of care. The Priory Group is responsive to any external investigation that may highlight areas for improvement within the healthcare industry. As such, we have reviewed the recommendations from the Francis Inquiry that were published in March 2013, and have already committed to take forward a number of actions arising from the report. Therefore, I am delighted to accept the role of Chief Nursing Officer for the Group; strengthening the voice of nursing and leading on professional standards. We will continue to support our staff, hear the voice of our service users, and safeguard our vulnerable adults and children in the changing health and social care landscape to ensure we are well equipped to meet the challenges ahead. Siân Wicks Director of Corporate Assurance and Chief Nursing Officer June 2013 The way in which we aim to improve on best practice standards is by listening to our service users; our experts by experience. This, along with benchmarking ourselves against National Institute for Health and Care Excellence (NICE) quality standards and other national and international standards, is fundamental as we strive to make a difference to the people who use our services. We ensure that our policies and procedures are up to date, evidence-based and take into consideration regional Quality is at the heart of everything we do 9 Overview of the Priory Healthcare division Acute mental health services Eating disorder services With the largest network of mental healthcare hospitals and clinics in the UK, we offer a flexible range of treatment programmes that feature: As the market leader in specialist acute care and high dependency treatment, including naso-gastric and PEG feeding, Priory hospitals offer a broad range of innovative therapy programmes and creative workshops alongside: comprehensive, multidisciplinary therapy services with a single point of access integrated and personalised treatment programmes, tailored to the needs of the service user bespoke therapeutic interventions, including dialectical behaviour and mindfulness therapies treatment programmes for service users with a dual diagnosis close working relationships with commissioners, which have delivered a 30% reduction in length of stay structured pricing plans, including episode pricing and relapse guarantees 95% rated the quality of their care as good or excellent 80% demonstrated improvement in their attitude to their diet, shape and weight 91% gained weight one-stop, direct access into our therapy services 99% 86% rated the overall quality of their therapy treatment as good or excellent showed improvement in their overall mental wellbeing Child and adolescent mental health services (CAMHS) 75% demonstrated recovery or significant improvement at discharge from therapy Addiction services Offering 12 months of aftercare and family support included as part of personalised addiction treatment programmes, Priory hospitals provide: specialist programmes to address underlying psychological issues, such as trauma reduction 10 We accept referrals into our CAMHS facilities 24 hours a day, seven days per week and provide a two hour response time to emergency requests. Our service is designed to enable children and young people to improve their long term wellbeing, which promotes effective reintegration into the community by providing: a wide range of specialist therapeutic interventions innovative treatment programmes that are tailored to the unique needs of each young person second stage residential rehabilitation a focus on promoting safe and sustainable recovery within the least restrictive environment possible 30 years of experience in treating addictions structured pricing plans a free initial assessment facilities across the UK 98% rated the quality of their treatment as good or excellent 95% of young people were satisfied with the overall quality of their care 93% showed improvement in their overall mental wellbeing after seven days 24% reduction in absconsions 99% felt that they were treated with dignity and respect 77% showed improvement in their overall mental wellbeing Complex care services Autism and Asperger’s syndrome services With personalised packages of care for people with complex and intensive or rehabilitative needs, the Priory offers the highest quality of rehabilitation and recovery as well as: Our residential homes provide high quality, supportive community living within safe, structured and engaging environments. Our aim is to enable each person to develop essential social, educational and vocational skills that will help them to progress towards a more positive future and successful independent living wherever possible by: active engagement with the service user and their family in their care plan wherever possible high success rates in reducing levels of aggression and behaviours which challenge generic services tailoring therapy treatment to each service user's unique needs an adapted recovery model for individuals with cognitive impairment emphasising the development of appropriate social behaviours, communication and interpersonal skills bespoke pricing and care packages providing the opportunity to access a wide range of activities, facilities, clubs and social groups within the community 85% rated the overall quality of their care as good or excellent 99% wholly or partially achieved their goals Secure services Offering a comprehensive care pathway and intensive rehabilitation programmes for service users from medium and low secure services through to step-down provision and independent living, we provide: providing seamless access to services that facilitate continuity of care and support 100% of support plans include personalised, outcome driven goals 100% of residents engage in activities within the community 89% of residents have accessed education or work in the last six months high levels of support for service users that have failed in multiple placements Neuro-disability services a recovery focused philosophy that encourages service users to take more control over their lives Offering the highest quality of long term care and rehabilitation to people with a neuro-developmental disorder or brain injury, we: episode pricing for medium and low secure units based on predicted lengths of stay adaptable and flexible pathways structured pricing plans and volume discounts 63% 64% 0 showed improvement in their overall mental wellbeing combine a personalised approach to treatment with the practice of some of the most experienced and well respected clinicians within the UK provide evidence-based treatment programmes that demonstrate real life changing results for those in our care 100% believed that staff communicate in a way that is easy to understand 93% felt that they received enough emotional support 100% believed they are cared for and supported showed improvement in their risk profile never events 11 Part 2 – Performance against 2012-13 objectives To ensure that we achieve the highest standards of quality, we continually strive to improve in the areas that define both the experience and outcomes of our service users. This includes scrutinising the processes and practices that we adopt to achieve these goals, alongside investment in our staff, services and facilities. We have identified eight priorities for improvement in 2013-14 at a divisional and service level, which are detailed in Part 3 on pages 16 and 17. In this section, we will analyse our progress against the objectives prioritised within the 2011-12 Quality Account, using data held in our service user management system CareNotes and other IT systems, to demonstrate our achievements in these areas. To ensure the most accurate and effective evaluation of the objectives identified, we have used baseline indicators from the 2011-12 Quality Account where possible. Our Quality Account will make reference to a number of acronyms and these have been detailed in the glossary at the end of this report (page 39) for ease of reference. Results of our service user satisfaction surveys 2012-13 To improve the quality of services that we offer, it is important to understand what people think about their care and treatment. The service user satisfaction survey is one way that the Priory Healthcare division obtains the opinion and experiences of people who have recently used our services. Using the results of these surveys, we are able to constantly improve our services to ensure they meet the needs of our service users. Theme Acute mental health Addiction Satisfaction of Priory service users remains high within our acute mental health, addiction and eating disorder services, with some improvement required within complex care and secure services in relation to care planning and communication. More detailed outcomes, including satisfaction results from our child and adolescent mental health services, are included on pages 18 and 19. Eating disorder Secure Complex care Average NHS benchmark* Involved in care planning and communication 96% 97% 97% 73% 82% 89% 90% Treated with dignity and respect 99% 99% 98% 82% 90% 94% 87% Given information regarding side effects of medication 82% 88% 80% 66% 73% 78% 72% Friend or family recommendation 97% 98% 92% n/a n/a n/a data not available * NHS benchmarking information taken from CQC Community Mental Health Survey 2012, which incorporates 61 NHS Mental Health Trusts in England, including combined community mental health and social care trusts. Since the most recent acute mental health service user satisfaction survey conducted by the CQC was undertaken in 2007, it is not possible to compare like for like outcomes directly. 12 Summary of progress against 2012-13 Quality Indicators In 2011-12, our Quality Account incorporated the feedback from service users, Priory staff, commissioners and other external stakeholders, to identify four priority areas and 12 priority goals for 2012-13. In this section, we will summarise our achievements against these priorities and provide a detailed breakdown on pages 14 and 15, covering the domains of: improving outcomes for service users (under the 2013-14 domain of: clinical effectiveness) delivering safe and secure services (under the 2013-14 domain of: service user safety) ensuring a positive experience (under the 2013-14 domain of: service user experience) investing in staff, education and training (under the 2013-14 domain of: clinical effectiveness) Page ref Priority Service Outcome Improving outcomes for service users in 2012-13 14 Improve risk assessment and management of all service users, including informal service users Acute mental health and addiction services Achieved 14 Spread innovation in severe anorexia across all eating disorder facilities Eating disorder services Achieved 14 Improve care planning and other clinical documentation so that it is more tailored for adolescent service users Child and adolescent mental health services Achieved 14 Improve multidisciplinary team working across all sites Complex care services Achieved Delivering safe and secure services in 2012-13 14 Spread innovation in risk assessment practice Secure services Mostly achieved 14 Reduce absconsions from units by 25% Child and adolescent mental health services Mostly achieved (24%) Ensuring a positive experience of care in 2012-13 15 Improve service user perception of family involvement in care planning by 25% Child and adolescent mental health services Mostly achieved (24%) 15 Increase service user involvement in the appointment of senior clinical staff at site level Child and adolescent mental health services Mostly achieved 15 Improve service user representation at ward and site level meetings Secure services Achieved 15 Improve standards of nutritional care Neuro-disability and complex care services Achieved Investing in staff, education and training in 2012-13 15 Introduction of General Medical Council (GMC) revalidation for all doctors, with individualised clinical governance data All services Achieved 15 90% of staff to undertake training relating to the Mental Capacity Act All services Achieved 13 Detailed review of performance against 2012-13 objectives >>Improving outcomes for service users Complex care services Acute mental health and addiction services Improve multidisciplinary team working across all sites Improve risk assessment and management of all service users, including informal service users • • Measure: Audit of inpatient and day patient risk assessment quality by September 2012; resulting action plan to be completed by March 2013 • Measure: Audit and act on the results of: – ward round frequency documentation and attendance – consultant performance of medical reviews and CPAs – internal compliance inspections • Achieved: Internal inspections were undertaken, which generated action plans as required. Clinical governance minutes are sent to the internal compliance team monthly and outstanding actions relating to internal compliance inspections are monitored via the monthly Healthcare dashboard pack Achieved: Care plan and risk assessment audit was completed across both services. A training module was formulated and cascaded to all sites Eating disorder services Spread innovation in severe anorexia across all eating disorder facilities • • Measure: All adult eating disorder facilities to organise, or contribute to, the development of a local multiagency group to develop protocols for the management of physically ill service users with anorexia nervosa >>Delivering safe and secure services Secure services Spread innovation in risk assessment practice • Measure: For each unit to produce a training and implementation plan for moving towards implementation of the Structured Assessment of Protective Factors (SAPROF) clinical risk assessment tool by December 2012 • Mostly achieved: Fully implemented in some sites and partially in others. All sites have a training plan towards implementation Achieved: CQUIN achieved in this area. Procedures, training and action plans in place Child and adolescent mental health services Improve care planning and other clinical documentation so that it is more tailored for adolescent service users Child and adolescent mental health services • Measure: New set of adolescent specific documents on CareNotes by December 2012 Reduce absconsions from units • Achieved: CAMHS specific multidisciplinary team meeting formats and Care Programme Approach (CPA) reports have now been developed. In addition, capacity and family feedback procedures have been implemented • Measure: A reduction in absconsions by 25% between April 2012 and April 2013 • Mostly achieved: A 24% improvement noted – from 42 absconsions in quarter 4 of 2011-2012 to 32 absconsions in quarter 4 of 2012-2013 50 Q4 2011-12 Improve quality and frequency of consultant and therapist reports to GPs Measure: Audit by September 2012, action plan to be completed by March 2013 Due to a strategic review, this objective was changed to improve the quality of clinical documentation, which has been reported in the priority above 14 Linear (2012-13) Absconsions • 2012-13 25 0 Q4 2011-12 Q1 2012-13 Q2 2012-13 Q3 2012-13 Q4 2012-13 >>Ensuring a positive experience in care Neuro-disability and complex care services Child and adolescent mental health services Improve standards of nutritional care Improve service user perception of family involvement in care planning • Measures: • Every service user will have a nutritional screening using a recognised tool • Therapeutic diets to be provided when required • All menus to provide balance and choice • Staff to be trained in nutrition and dysphagia management • Staff to be trained in supporting service users at mealtimes • Achieved: A dietetics assessment on admission is followed by therapeutic diets, which are prescribed by the dietitian as required. Menus are developed on site by the head chef and reviewed by the dietitian to ensure they are balanced and meet the service users’ needs. Care and catering staff are trained by both the dietitian and speech and language therapist • Measure: 25% improvement in service user satisfaction within this aspect of care • Mostly achieved: The average satisfaction score for 2011-12 was just over 85%, and the score achieved in quarter 4 of 2012-13 was 89%. The 24% overall improvement just misses the 25% target 90% 2011-12 average 2012-13 85% 80% >>Investing in staff, education and training 2011-12 Q1 2012-13 Q2 2012-13 Q3 2012-13 Q4 2012-13 All services Increase service user involvement in the appointment of senior clinical posts at site level Introduce GMC revalidation for all doctors, with individualised clinical governance data • Measure: To have a service user representative on all new appointment panels for senior clinical posts at site level • • Mostly achieved: Following a two year pilot, learning and guidance will now be shared across our CAMHS wards, and training tools and guidelines for young people to participate in recruitment will be developed. Staff retention and performance will also be analysed Measures: • Full approval of the policies and procedures from the SHA and GMC by June 2012 • 50% of appraisers to be trained by the end of 2012 • All doctors to move towards revalidation by the end of 2012 • Active management of doctors in difficulties • Good consultant level quality information to support revalidation by June 2012 • Achieved: 65% of doctors had completed appraiser training by December 2012. All doctors are in the appraisal cycle and are being tracked. There is a policy in place for managing doctors in difficulty with active monitoring and review. Quality data is monitored and included in the revalidation process Secure services Improve service user representation • • Measure: All secure facilities to establish a service user forum with representation from each ward, and facilitated by a senior manager. Service user representatives to attend business or clinical governance meetings and clinical governance committees for the ward Achieved: In all facilities, a service user representative attends for part of the clinical governance meeting to raise issues from the ward meetings and hospital-wide service user councils or forums Improve staff knowledge of Mental Capacity Act • Measure: Staff completion of Mental Capacity Act training to increase to 90% via online e-learning, from 2011-12 baseline of 67% • Achieved: 90% compliant 15 Part 3 – Priorities for improvement 2013-14 In addition to the requirements laid out by the Commissioning for Quality and Innovation (CQUIN) framework and other nationally prescribed standards of clinical excellence, the Priory Healthcare division has included feedback from our service users, Priory staff, commissioners and other external stakeholders to identify eight priorities for improvement during 2013-14. These priorities have been determined in accordance with the guidelines issued by the healthcare regulator Monitor, which will ensure a transparent and consistent approach to our quality reporting going forward. Our priorities will be measured via monthly Business Review Meetings and fall under the three domains of: clinical effectiveness service user safety service user experience >>Quality performance indicators for the Priory Healthcare division >>Quality performance indicators by service Clinical effectiveness and service user safety Secure services Service user experience All service users to have their physical healthcare needs assessed and a plan put in place to address areas of physical health need Service users to participate in the recruitment of senior clinical posts (Ward Manager equivalent and above) across all our secure sites • • Rationale: NHS nationally prescribed CQUIN within the secure service specification • Target: Service users to be involved in 80% of interviews for senior clinical posts at their sites • How will it be measured: Audit of appointments within secure services at site level via the HR electronic records • • Rationale: In 2012 the Schizophrenia Commission report, The Abandoned Illness noted that “people with severe mental illness such as schizophrenia still die 15 to 20 years earlier than other citizens”. The NHS has also focused on this aspect of care, including it in the nationally prescribed CQUIN for mental health services Target: 90% of CPAs to have a physical healthcare plan in place and address needs in the following areas: alcohol consumption, smoking intake, previous illegal drug use, body mass index, cholesterol, blood glucose Complex care services Clinical effectiveness How will it be measured: The first quarterly audit of clinical health records (via CareNotes) will commence in September 2013 Increase service user involvement and engagement in meaningful activity to support their recovery and rehabilitation • Rationale: NICE Quality Standard (QS14): Meaningful activities on the ward and Service user experience in adult mental health (NICE clinical guidance 136); which states that service users in hospital should have access to a wide range of meaningful and culturally appropriate occupations and activities seven days per week, and not restricted to 9am to 5pm. These should include creative and leisure activities, exercise, self care and community access activities (where appropriate). Activities should be facilitated by appropriately trained health or social care professionals • Target: 25 hours of diverse and meaningful activity to be offered to every service user each week • How will it be measured: Audit of clinical health records (via CareNotes) to evidence the offer of activity and the number of hours taken up by the service user Clinical effectiveness and service user safety Ensure that unmet need is recorded for all service users to assist in the CPA and discharge planning process • Rationale: National specialist NHS prescribed services CQUINs and service specifications requirement • Target: 95% of CPA minutes and multidisciplinary team (MDT) review minutes to record any unmet need and if there is no unmet need, that there is a clear statement outlining this • 16 How will it be measured: The first quarterly audit of CPA minutes and MDT review minutes will commence in September 2013 Eating disorder services Service user experience Acute mental health services Service user safety Increase family and carer engagement and wellbeing Ensure that the service user is signposted to appropriate support services in the event of a crisis upon discharge from acute services • Rationale: NHS nationally prescribed mental health specification and standard for the Quality network for Eating Disorders (QED) • Target: 90% of families or carers to be offered a Priory Carer Wellbeing Workbook and to attend a wellbeing planning meeting • How will it be measured: Sites to keep a record of the number of workbooks given out and wellbeing planning appointments taken up Child and adolescent mental health services Service user experience Service users to be more involved and to participate in the planning and review of safe, sound and supportive services • Rationale: NHS nationally prescribed CAMHS service specification and Quality Network for Inpatient CAMHS (QNIC) standard • Target: Service user presence at 90% of clinical governance meetings • How will it be measured: Clinical governance minutes to record service user attendance and sites to submit a quarterly report to be included in the quarterly service user action plan • Rationale: Standard 17.6 Accreditation for Inpatient Mental Health Services (AIMS): standards for inpatient wards – working age adults; which states that service users should be given information on discharge in a written aftercare plan, which includes the action to be taken should signs of relapse occur or if there is a crisis, or if the service user fails to attend treatment • Target: 90% of service users to be offered a crisis card upon discharge • How will it be measured: Each hospital to keep a record of the number of cards offered, and the number of times a discussion took place to explain the purpose of the card Secure services Service user experience Increase service user satisfaction in relation to care planning and communication • Rationale: National specialist service specification for the NHS for medium and low secure mental health services • Target: Service user satisfaction to increase by 10% from the 2012-13 baseline of 73% • How will it be measured: Through the service user satisfaction survey Group therapy helped me to share my thoughts and feelings with others and made me feel less alone with my problems 17 Part 4 – Additional information Service user satisfaction – delivering value through clinical excellence Service user satisfaction provides a key stimulus to service development both across the Priory Healthcare division itself and between services within the Priory Group of Companies. We know that service users who are engaged with the care that they are receiving from healthcare professionals they can trust, is a fundamental driving force to ensure the best possible outcomes. Service users with a forensic history who have been admitted into our low and medium secure facilities have demonstrated a lower level of satisfaction with the service in 2012-13 than within other areas of the Healthcare division. This may be partially attributed to the length of their formal detainment, but will be an area of focus for us in 2013-14. Overall satisfaction with the quality of care by service 97% acute mental health services 95% child and adolescent mental health services 99% day therapy services 100% neuro-disabilty services 98% addiction services 85% complex care services 95% eating disorder services 71% secure services Highlights from the service user satisfaction survey by service 18 Acute mental health services survey Day therapy services survey Key findings from our service users: Key findings from our service users: 97% would recommend us to a friend 99% felt treated with courtesy and respect 99% said that they were treated with dignity and respect 97% said that we understood their needs and difficulties 98% reported that they felt safe during their stay 97% felt that their therapy was as good as expected Addiction services survey Complex care survey Key findings from our service users: Key findings from our service users: 99% said that when they arrived, staff made them feel welcome 88% were happy with the support they got from their support worker 98% would recommend our services to a friend 87% felt cared for and supported 99% said that they were treated with dignity and respect 90% said that they were treated with dignity and respect Eating disorder services survey Secure services survey Key findings from our service users: Key findings from our service users: 98% said that when they arrived, staff made them feel welcome 79% felt that they were consulted on decisions about their medication 98% said that they were treated with dignity and respect 82% said that they were treated with dignity and respect 97% reported that they felt safe during their stay 74% felt that they were well supported with the moving on process Child and adolescent mental health services survey Neuro-disability services survey Key findings from our service users: Key findings from our service users: 91% felt that the service helped to deal with their problems 100% felt safe and secure 94% felt that their healthcare professionals listened to and understood their problems 100% believed time spent on their interests was encouraged 93% were satisfied with the services offered to them 94% felt they are able to attend service user meetings 19 Outcomes – the success of our service users One of the central objectives of the Priory Healthcare division is to enable every service user to be an active participant in their own recovery process, where possible. Outcomes demonstrate the progression that each service user has made, and as such, are an intrinsic element of every personalised care pathway. When appropriate, we regularly feed outcomes back to the individual, alongside families and carers, as well as those who commission our services and form an integral part of the individual's wider care pathway. Clinical outcomes within acute mental health, addiction services and eating disorder services use the nationally recognised Health of the Nation Outcomes Scales (HoNOS). The HoNOS assessment is undertaken upon admission and again at discharge (or bi-annually within our secure services) to ascertain the level of improvement in a service user’s clinical condition during their inpatient stay. Acute mental health services 86% showed improvement in their overall mental wellbeing 75% demonstrated significant improvement or recovery at discharge from therapy Within child and adolescent mental health services, we use the Health of the Nation Outcomes Scales for Children and Adolescents (HoNOSCA), and the HoNOS Secure tool is used within our low and medium secure facilities. All of the HoNOS outcomes quoted below that relate to improvement in overall mental wellbeing refer to service user outcomes at the point of discharge. Across the Healthcare division, additional outcome tools may also be used, according to the nature of each service. We believe that progress is made in many forms, and achieving outcomes is relevant to the unique needs of each service user. This means that we also consider the social, emotional and physical development of the individual alongside their clinical progression. For this reason, we place great emphasis on qualitative outcomes alongside clinical metrics to reflect the success of our service users. Complex care services 99% Addiction services 86% were still abstinent 12 months post discharge* 93% showed improvement in their overall mental wellbeing** Child and adolescent mental health services 77% showed improvement in their overall mental wellbeing Eating disorder services 80% wholly or partially achieved their goals 100 demonstrated improvement in their overall attitude to their diet, shape and weight 50 91% gained weight 0 77% showed improvement in their overall mental wellbeing Discharge 3 months 6 months 9 months 12 months Abstinent since last PARQ Abstinent but relapsed since last PARQ Abstinent but improved Not abstinent Service user abstinence over 12 months * 86% of service users admitted into a Priory hospital, who were not readmitted and could be contacted, were still abstinent 12 months post discharge using the Priory Addiction Recovery Questionnaire (PARQ) outcome measure ** 93% of service users showed improved overall mental wellbeing where their length of stay was greater than seven days 20 Secure services 63% showed improvement in their overall mental wellbeing 64% showed improvement in their risk profile 26% overall reduction in the rate of incidents during the second six months of admission* I'm very thankful for the professional and engaged treatment I received at the Priory. It exceeded all expectations and has been a turning point in my life Realising dreams ... at the Priory Grange Heathfield Staff at a Priory hospital in East Sussex have helped to make a dream come true for one of their residents who expressed a wish to take part in a half marathon. Darren, who has Huntington’s disease, a progressive neurological condition that requires him to use a wheelchair, has been called ‘an inspiration’ after completing the 2013 Hastings half marathon. With the support of his team at the Priory Grange Heathfield, Darren completed the course in four hours and raised £800 for the charity MIND. The race organisers have been so impressed by his achievements that they presented Darren with a special achievement award at a ceremony in April 2013. The Registered Manager at the Priory Grange Darren’s desire to take part in a race emerged after an Heathfield said: occupational therapy assistant at the hospital ran the Brighton Marathon. “We are all very proud of what Darren has achieved. Despite his illness, he maintains a real zest for life. Darren went along to support him, and a few days later Our aim is to provide staff and services which inspire revealed he would have loved to have done a marathon an individual to achieve their best possible outcomes. before he became ill. As soon as staff heard this they made Helping Darren to realise one of his dreams reflects every effort to help make his dream come true. A team this ethos.” of ten Priory staff volunteered to assist Darren on the day, with some pushing his wheelchair and others running Darren, who has lived at the Priory Grange Heathfield alongside him. since 2010, added: “The day was great and I loved it.” * Reduction in rate of incidents during the second six months of admission compared to the first six months of admission 21 Investing in staff, education and training Learning and development We recognise the important contribution that staff make both in terms of the quality of care delivered and service user experience. Foundations for Growth, our internal e-learning programme for staff, was launched seven years ago and in 2012-13 alone, the programme has enabled Healthcare staff to complete 81,409 e-learning modules and 17,674 face to face training sessions. However, we also recognise the importance of learning and development within the wider context of delivering quality and inspiring innovation within our services. For this reason, over £90,000 was invested in the continuing professional development of 288 people in order to supplement their ongoing training during 2012-13. Percentage of allocated e-learning modules completed by Priory Healthcare staff during 2012-13 Safeguarding vulnerable adults 94% Safeguarding children 99% Confidentiality and data protection 99% Infection control 92% Managing challenging behaviour 92% Safe handling of medicines 97% Suicide and self harm 98% Mental Capacity Act 90% Deprivation of liberty 90% Staff opinion The annual Colleague Opinion Survey is well received by staff from the Healthcare division, with a response rate of 63% for the 2012 survey (the highest response rate in the Group). Where possible, the results of this survey have been benchmarked against the NHS. We recognise that, although staff recognition is higher within the Priory Healthcare division than the NHS benchmark identified below, it is still an area of focus for the Group. Therefore, we will be launching an internal awards scheme in 2013, which aims to recognise the many significant contributions made by staff members across the Group. Achievements are also highlighted in the weekly staff e-newsletter, which was launched in 2012. The Group also undertook a Culture Survey in 2012, and results for the Healthcare division were positive, with highlights included on page 8 of this Quality Account. Staff opinion key findings: 22 Theme Result NHS benchmark Feel they are able to contribute to the success of their team 89% 66% Feel they are able to do their job to a standard they feel pleased with 79% 63% Would recommend Priory as a good place to work 74% 48% Would recommend Priory for treatment or care to a friend or relative 67% 60% Feel they will still be working for Priory in 12 months time 91% 78% Feel they achieve recognition for good work 54% 49% Completed the Colleague Opinion Survey and gave positive answers to all of the questions asked 71% data not available The Commissioning for Quality and Innovation (CQUIN) framework All services contracted using the national standard bilateral or multi-lateral contract may be subject to a CQUIN scheme. For our contracts in 2012-13, this was principally for specialised commissioned services such as secure services, child and adolescent mental health services and eating disorder services. The full CQUIN framework is detailed from page 40 in the appendix. The quarter four reports have been submitted to the commissioners to review and so far indicate that we have achieved 100% of our targets. Service Target Outcome Eating disorder Implementation of the recommendations from the Royal College of Psychiatrists report – Management of Really Sick Patients with Anorexia Nervosa (MARSIPAN) Achieved Child and adolescent mental health Education, training and meaningful activity: ensuring that the service user experience features activities which lead to effective rehabilitation and hence timely discharge Achieved Service user involvement in recruitment Achieved Patient flow annual report Achieved Patient Safety Thermometer: improve responsiveness to personal needs of service users Achieved Improvement in outcomes Achieved Improving physical healthcare and wellbeing of service users Achieved Payment by Results (PbR) feasibility project: to implement, review and feed back the requirements set out in the Feasibility Implementation Booklet within a clear reporting structure. This includes: clustering, five care pathway indicators, benchmarking and reporting feasibility Achieved Shared pathway: recovery and outcomes Achieved Shared pathway – implementing standard secure pathway: to introduce and monitor key milestones on the service user pathway in order to make the pathway more efficient and reduce length of stay Mostly achieved Access to specialised mental health services Achieved 25 hours of meaningful activity per week Achieved Quality dashboard: to implement the routine use of specialised services’ clinical dashboards Achieved User defined CPA standards: to introduce and monitor the 20 service user defined CPA standards Achieved Optimising length of stay: to understand the total care pathway, and plan how it might work differently in order to optimise length of stay Achieved Secure Applicable to all three of the above services 23 Participation in clinical audits and National Confidential Inquiries All sites across the division have completed safeguarding and ligature audits during the year and action plans have been produced to address any areas not meeting the required standard. Hospitals also complete bespoke audit schedules based on local need. Ashtons, our pharmacy suppliers, have increased the frequency of their audit programme and now undertake monthly audits of prescribing and administration of medication within Healthcare. The auditors’ results are fed back to sites on a weekly basis allowing them to rectify any errors as soon as they occur. The increased frequency of audits has led to an improvement in the quality of medicines management across the Healthcare division (see table below). There is one National Confidential Inquiry which is relevant to the Healthcare division: the National Confidential Inquiry into Suicides and Homicides by people with a mental illness (NCISH) and information is provided to the Inquiry as requested. No. of prescription cards MHA compliance errors % Patient details errors% No. of prescription items Prescription writing errors % Administration errors % Q1 11573 2.3 1.4 109127 1.5 2.2 Q2 11273 1.5 1.3 109006 1.3 2.3 Q3 10804 1.7 1.0 105515 1.2 1.9 Q4 11560 1.1 1.1 112858 0.9 1.6 Total 45210 1.7 1.2 436506 1.2 2.0 I was anxious – it was clearly identified that I was anxious and I was treated with kindness, respect and dignity 24 Regulatory compliance The Healthcare division covers England, Scotland and Wales, and is therefore required to work under the standards set out by regulators within each respective area. 43 of our 54 healthcare sites were inspected by regulators between 1st April 2012 and 31st March 2013. These are broken down by regulator as follows: Care Quality Commission 37 Health Inspectorate Scotland 1 Health Inspectorate Wales 2 Care and Social Services Inspectorate Wales 3 96% of outcomes inspected by our regulators were met Care Quality Commission Health Inspectorate Scotland The Care Quality Commission inspected 217 outcomes identified in the Essential Standards of Quality and Safety across Priory Healthcare English sites between April 2012 and March 2013. The Health Inspectorate Scotland inspected five outcomes identified in the Scottish regulations at the Priory Healthcare Scottish site between April 2012 and March 2013. The Inspectorate deemed this site to be fully compliant within all areas assessed. of outcomes were judged to have been met 95% Of the 217 outcomes assessed, nine were found to be unmet within eight areas of inspection. The graph below highlights the number of unmet outcomes compared to the total number of met outcomes within these eight areas. 40 100% of outcomes were judged to have been met Outcomes inspected Met Quality of information 1 Quality of care and support 1 Quality of environment 1 Quality of staffing 1 Quality of management 1 Unmet Met 20 Records Unmet Quality of service Medicines Infection control Safeguarding Care and welfare Consent to care Respecting/involving people 0 Met 25 Healthcare Inspectorate Wales Care and Social Services Inspectorate Wales The Healthcare Inspectorate Wales inspected 11 standards identified in the Welsh regulations at Priory Healthcare Welsh sites between April 2012 and March 2013. There were no unmet standards identified by the regulator in the time period. The Care and Social Services Inspectorate Wales inspected 12 standards across Priory Healthcare Welsh sites between April 2012 and March 2013. 11 of the standards were judged to have been met. One standard was deemed to have been unmet – quality of environment – at one site, Newhouse, which has since been relocated to a new site. 100% of standards were judged to have been met 92% of standards were judged to have been met Standards inspected Met Medicines 1 Standards inspected Met Unmet Statement of purpose 2 Quality of information 3 0 Quality of service provision 2 Quality of care and support 3 0 Notification of other incidents 2 Quality of environment 2 1 Financial position 2 Quality of staffing 3 0 Notification of death 1 Notification of death and the MHA 1 Embargoes and warning notices Currently there are no embargoes in place at any Priory Healthcare site. Across the division during 2012-13, the following action was carried out as a result of issues detailed on page 27 at the Priory Hospital Middleton St George, the Priory Ticehurst House, the Priory Highbank Centre, Newhouse, the Priory Hospital Widnes and Cefn Carnau: Sites with Warning Notices 2 Site with Regulatory Embargoes to Admissions 1 26 Focus sites during 2012 -13 From time to time, particular areas of care or service delivery fail to achieve the high standards of quality that our regulators and service users rightly expect. This section details areas in which compliance with our regulatory bodies may have fallen short and required remedial action to be taken. On the rare occasion that an issue should arise, we communicate openly and always work as closely as possible with our regulators and commissioners, service users, their families and carers and other external stakeholders for as long as necessary to ensure full confidence in our service is restored. The Priory Hospital Middleton St George Newhouse As a result of an inspection in January 2013, the CQC raised concerns about our recruitment procedures at the hospital, which were followed up with a warning notice. An action plan was promptly implemented to address these issues. Newhouse in Cardiff was acquired by the Priory Group as part of the wider acquisition of Craegmoor services in 2010. Since acquisition, the site had some issues around the physical environment of the buildings. Following re-inspections from the CQC and rigorous responsive intervention, the hospital was found to be compliant with the regulations. The internal compliance team and the operational management at the hospital continue to implement and monitor improvements to ensure future and ongoing compliance. The Priory Ticehurst House Following a serious incident in November 2012, a decision was taken by the Group to commence a voluntary restriction on admissions whilst an investigation took place. The hospital worked closely with regulators and commissioners throughout this time to ensure compliance with regulations were maintained. The CQC inspected the hospital in November 2012 and found the site to be compliant with all outcomes inspected. On completion of the investigation and implementation of actions arising, the voluntary restriction was lifted on the 1st March 2013 with the support of commissioners. The Priory Highbank Centre In response to a serious allegation of abuse towards a service user at the Priory Highbank Centre, a temporary suspension was placed on the site. The CQC carried out an investigation immediately following the allegation, and found the site to be compliant in all areas assessed. An external investigation was later carried out by the safeguarding lead for NHS Bury and NHS Liverpool in conjunction with the safeguarding lead for the local authority, which concluded that this was not a systemic issue. As a result, the commissioners lifted the suspension on the site. A thorough internal investigation was also carried out. In March 2012, a restriction on new admissions was agreed with the regulator to allow an effective solution to be adopted. The Group made a decision to relocate the service to a new purpose-appropriate facility in Aberdare, which opened on 16th April 2013. The Priory Hospital Widnes Following the acquisition of the Priory Hospital Widnes in 2011, the Group was unable to sustain improvements, and ongoing quality issues led to enforcement action from the CQC. After a number of discussions with regulators and commissioners, it was decided to de-register the service in September 2012. At this time, the Priory Group worked closely with commissioners, service users and their families to ensure the safe transfer of service users to new locations suitable for their needs. Cefn Carnau After a detailed analysis of challenges facing the clinical team on one of the wards at the hospital, a decision was taken to review the admission processes to the ward. In order to achieve this, the hospital voluntarily suspended admissions to ensure that these processes could be reviewed effectively. This commenced on 25th May 2012 and remained in place until 28th September 2012. This process was carried out with the full knowledge and support of the regulator and commissioners of the service. 27 Working in partnership with our commissioners and regulators Within the Priory Healthcare division alone, 78% of our services are commissioned on behalf of the NHS and other public bodies throughout the UK. It is therefore essential to us that our services are delivered in close collaboration with referring commissioners and other external care providers to ensure the optimum outcome for each service user as part of their overall care pathway. This means ensuring early visibility of the service user’s progression throughout each treatment phase relevant to their individual goals and objectives and, where possible, developing a stepped care approach to treatment, with transparent and flexible pricing frameworks. As a commissioner, I use the Priory because they have a very comprehensive range of services, and I have generally found they are of a high clinical standard. When I am tasked, as is frequently the case, with finding an inpatient service for a client with complex needs, the Priory Group is one of the providers I think of first for the above reasons. They usually have a specialist service that potentially offers what I need... (and) I find my point of contact to be helpful, responsive and a great ambassador for the Priory Group... Lastly, in my experience as a Group, they are responsive to requests for assessment; responding quickly both with the assessment as well as a proposal of care for a particular client Steve Southall Out of Area Placements Manager at Berkshire Healthcare NHS Foundation Trust The Priory's range of services enable us to place people quickly and appropriately. They are our largest contracted provider of eating disorder services, providing a specialist service for people with complex needs, who often present with high levels of risk and physical difficulties. We often source CAMHS beds from them, because they provide a full care pathway of services for young people and are always very responsive, admitting 24 hours a day, seven days per week. Priory have a full and diverse multidisciplinary team across all their services, providing a high standard of clinical care and good outcomes. We find them easy to work with, good at communicating with us and local teams, and they are well embedded in the local healthcare economy Steve Hamer Supplier Manager at NHS England (Cheshire, Wirral and Warrington Area Team) 28 Improving safety for our service users As a Group, Priory strives to foster an open and transparent culture, in which staff feel able to report incidents as they occur. We believe that this approach is fundamental to driving improved processes and practices within our services. Priory Healthcare reports all incidents using a bespoke electronic reporting system, to which all clinical staff are provided access. Its use is explained during the staff member’s induction, and an overview of the importance of incident reporting is also included within the e-learning modules on Safety, Quality and Compliance. In line with the ethos of the National Patient Safety Agency, we encourage our staff to report all incidents, serious incidents and near misses using this reporting system*. 2012-13 2011-12 NHS average (2012-13) Total number of incidents reported (per 1000 ordinary bed days) 21.8 21.29 23.8 Serious incidents relating to the death of a service user 0.2% 0.2% 0.8% Incidents resulting in the permanent harm of a service user 0.3% 0.04% 0.8% During 2012-13 there were no incidents that would be classified as never events as defined by the National Patient Safety Agency. Life-long learning ... at the Priory Hospital Keighley Service users at the Priory Hospital Keighley, a complex mental health and rehabilitation hospital in West Yorkshire, have recently taken part in a session at Jamie Oliver’s Ministry of Food in Bradford. The ten week scheme offers the opportunity for service users with complex mental health problems who require longer or ongoing hospital care to learn to cook traditional recipes, whilst promoting core independence skills as part of their rehabilitation. The scheme enabled the mixed functional ability group to master cooking skills, whilst building their confidence and developing time management and team working skills. Funders, including the NHS and local councils, have helped to establish Ministry of Food sites across the country, teaching how to cook from scratch using fresh, seasonal ingredients and in doing so, lead healthier lives with improved eating habits. “The response we have had from service users has been great; they are very relaxed, laughing and presenting as high functioning when usually they struggle with everyday daily living. It has also had a really positive and unexpected impact on my working relationship with individuals who now feel empowered to take more control over their recovery journey.” Occupational therapist * A new incident reporting system was implemented during 2012 to provide closer alignment with NHS categorisations of incident reporting. Therefore, it is not possible to compare safety performance between 2011-12 and 2012-13 directly. More information on the reporting of incidents can be found in the appendix on page 45. 29 Continuous improvement in the delivery of our services Providing a high quality service for both our service users and those who commission our services is a central objective for the Priory Healthcare division. As such, we take all complaints very seriously and utilise this feedback as part of an overall ethos to drive service development through continuous improvement. Over the course of 2012-13, we have implemented a more thorough and effective reporting mechanism in order to ensure that the management and resolution of complaints is handled with greater efficiency and transparency. We operate a robust and thorough framework for managing all complaints, which comprises of three stages: Stage one Complaints are resolved at a local level by the individual service or site within an agreed response timeframe. Whilst the majority of complaints are satisfactorily resolved in this manner, a complainant may request in writing that the issue be referred to stage two if they remain dissatisfied, following a final attempt to resolve by further dialogue or meetings Stage two The complaint is reviewed and/or reinvestigated by the Group Complaints Co-ordinator (part of the Safety, Quality and Compliance team) within an agreed response timeframe Stage three Further and final recourse for unresolved complaints is available through the Parliamentary Health Service Ombudsman (PHSO) for NHS-commissioned service users, or to the Independent Sector Complaints Adjudication Service (ISCAS) for those who are privately funded Complaints during 2012-13 Complaints per 1000 occupied bed days 2012-13 1.32 2011-12 1.45 2010-11 1.40 Due to the more robust reporting systems implemented during 2012, as well as the inclusion of new sites to the Priory Healthcare division following the acquisition of Craegmoor and Affinity Healthcare, the number of complaints referred to stage two review has increased during 2012 to 22 cases, compared with four in 2011. Two cases were referred to stage three (ISCAS) during 2011-12 and 2012-13 respectively. Following consultation with the Priory Healthcare division, the PHSO concluded that further investigation of one complaint made to the Ombudsman during 2012-13 was unnecessary. 30 Part 5 – Appendix 31 Statement of assurance from our lead commissioner This statement is given to the best of my knowledge for the period 2012-13 in respect of secure services, adult eating disorder services and child and adolescent mental health services commissioned by South Central Specialised Commissioning Group. Priory Healthcare has been compliant with the performance reporting cycle and have provided good quality, timely reporting in relation to the key quality indicators as defined in the contract. Priory Healthcare has complied with submissions of serious incident and safeguarding notifications, related reports and action plans. This has supported the robust monitoring of the safety and quality of placements, with areas of concern identified being addressed promptly. Priory Healthcare has enthusiastically and successfully implemented the national CQUINS across secure services, and has provided commissioners with good evidence to support the monitoring of achievements each quarter. Commissioner meetings with service users and the advocacy service at Thornford Park* have been supported and encouraged by Priory, and this has provided commissioners with invaluable feedback on the quality of service provision. Louise Doughty Head of Mental Health and Programme of Care Lead Wessex, NHS England * Thornford Park is a low and medium secure facility in Berkshire 32 Statement of directors’ responsibilities in respect of the Quality Account In preparing the Quality Account, directors are required to take steps to satisfy themselves that: 1. The content of the Quality Account meets the relevant requirements set out in Monitor’s Annual Reporting Manual 2012-13 2. The content of the Quality Account is not inconsistent with internal and external sources of information including: • Board minutes and papers for the period April 2012 to June 2013 • papers relating to quality reported to the Board over the period April 2012 to June 2013 • feedback from commissioners • feedback from external auditing reviews (conducted by PricewaterhouseCoopers) 3. The Quality Account presents a balanced picture of the Priory Healthcare division’s performance over the period covered 4. The performance information reported in the Quality Account is reliable and accurate 5. There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice 6. The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions and is subject to appropriate scrutiny and review 7. The Quality Account has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Account regulations) as well as the standards to support data quality for the preparation of the Quality Account The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board June 2013 Signed: Mike Jeffries Chairman The Priory Group Tom Riall Chief Executive Officer The Priory Group 33 Independent Limited Assurance Report to the Board of Directors of the Priory Group No. 1 Limited on the Annual Quality Report We have been engaged by the Board of Directors of the Priory Group No. 1 Limited (“the Company”) to perform an independent limited assurance engagement in respect of the Company’s Quality Report for the year ended 31 March 2013 (the ‘Quality Report’). Scope and subject matter The Company has voluntarily applied certain principles of the guidance provided by Monitor to NHS Foundation Trusts ‘Detailed Guidance for External Assurance on Quality Reports 2012/13’ (published 22 March 2013) (“the guidance”), and Annex 2 of the NHS Foundation Trust Annual Reporting Manual (“the ARM”). These principles have been selected based on those deemed applicable to the Company and have been set out in the ‘Format of the Quality Report’ section of the Appendix to the Quality Report. Monitor’s guidance for the Quality Report incorporates the requirements set out in the Department of Health’s Quality Accounts Regulations and additional reporting requirements set by Monitor. • the Quality Report is not consistent in all material respects with the sources specified below. We read the Quality Report and consider whether it addresses the content requirements of the ARM applicable to the Company, as set out in the ‘Format of the Quality Report’ section of the appendix to the Quality Report, and consider the implications for our report if we become aware of any material omissions. We read the other information contained in the Quality Report and consider whether it is materially inconsistent with the following documents: • Board minutes for the period April 2012 to March 2013; • the Company’s monthly complaints scorecard; • the quarterly patient surveys; • the annual staff survey dated May 2013; • papers relating to quality reported to the Board over the period; • feedback from the Commissioners (NHS England); and • feedback from Directors. We provide assurance in respect of: i) the content of the Quality Report, in line with the principles of the guidance and Annex 2 of the ARM that are applicable to the Company, as set out in the ‘Format of the Quality Report’ section of the Appendix to the Quality Report; and ii) the consistency of the Quality Report with the documents specified below Respective responsibilities of the Directors and auditors We are in compliance with the applicable independence and competency requirements of the Institute of Chartered Accountants in England and Wales (ICAEW) Code of Ethics. Our team comprised assurance practitioners and relevant subject matter experts. The Directors are responsible for the content and the preparation of the Quality Report in accordance with those principles of the guidance and Annex 2 of the ARM that are applicable to the Company, as set out in the ‘Format of the Quality Report’ section of the appendix to the Quality Report. This limited assurance report, including the conclusion, has been prepared solely for the Board of Directors of the Company as a body, to assist the Company in reporting the quality agenda, performance and activities. We permit the disclosure of this limited assurance report within the Quality Report for the year ended 31 March 2013. Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Board of Directors as a body and the Company for our work or this report save where terms are expressly agreed and with our prior consent in writing. • the Quality Report does not incorporate the matters specified in the guidance and Annex 2 to Chapter 7 of the ARM that are applicable to the Company; and 34 We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with those documents. Our responsibilities do not extend to any other information. Assurance work performed We conducted this limited assurance engagement in accordance with International Standard on Assurance Engagements 3000 ‘Assurance Engagements other than Audits or Reviews of Historical Financial Information’ issued by the International Auditing and Assurance Standards Board (‘ISAE 3000’). Our limited assurance procedures included: • making enquiries of management; • comparing the guidance and content requirements of the ARM that are relevant to the Company, as set out in the ‘Format of the Quality Report’ section of the Appendix to the Quality Report; and • reading the relevant documents and comparing their consistency with the information within the Quality Report. A limited assurance engagement is less in scope than a reasonable assurance engagement. The nature, timing and extent of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Limitations Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw, allows for the selection of different but acceptable measurement techniques which can result in materially different measurements and can impact comparability. The precision of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precision thereof, may change over time. It is important to read the Quality Report in the context of the content requirements of the ARM and the Directors’ determination of its applicability to the Company, as set out in the ‘Format of the Quality Report’ section of the Appendix to the Quality Report. The nature, form and content required of Quality Reports are determined by the Company based on Monitor’s guidance for the purposes of this assurance engagement. This may result in the omission of information relevant to other users. In addition, the scope of our assurance work has not included governance over quality or performance indicators in the Quality Report, which have been determined locally by the Company. Basis for qualified conclusion The ARM requires Part 2 of the Quality Report to include priorities for improvement then statements of assurance from the Board. Part 2 of the Quality Report does not include priorities for improvement, and instead these are included in Part 3 of the Quality Report. The applicable contents of the Statements of Assurance have been included in a number of sections throughout the report rather than in Part 2. The ARM requires information relating to registration with the Care Quality Commission and periodic/special reviews in a prescribed form of statement to be included in Part 2 of the Quality Report. This is not included within the Quality Report. The ARM requires Part 3 of the Quality Report to include performance against the relevant indicators and performance thresholds set out in Appendix B of the Compliance Framework. This has been included in the Quality Report, except for: • percentage of patients on Care Programme Approach who were followed up within 7 days after discharge; • percentage of admissions to acute wards for which the Crisis Resolution Home Treatment Team acted as a gatekeeper during the reporting period; • percentage of patients re-admitted to hospital within 28 days of discharge; • minimising mental health delayed transfers of care; • admissions to inpatients services had access to crisis resolution home treatment teams; • meeting commitment to serve new psychosis cases by early intervention teams; • data completeness: identifiers; and • data completeness: outcomes for patients on CPA 35 The ARM requires Part 3 of the Quality Report to include an overview of the quality of care offered by the NHS Foundation Trust based on performance in 2012/13 against indicators selected by the board in consultation with stakeholders, with an explanation of the underlying reason(s) for selection. The Quality Report does not directly provide an overview in the format prescribed by the guidance, and it is included within Part 2 instead of Part 3. Qualified conclusion Based on the results of our procedures, except for the matters described in the basis for qualified conclusion paragraph, nothing has come to our attention that causes us to believe that for the year ended 31 March 2013; • the Quality Report does not incorporate the matters set out in the guidance and Annex 2 of the ARM that are applicable to the Company as set out in the ‘Format of the Quality Report’ section of the appendix to the Quality Report • the Quality Report is not consistent in all material respects with the documents specified above. Date: PricewaterhouseCoopers LLP Chartered Accountants Benson House 33 Wellington Street Leeds The maintenance and integrity of the Priory Group Limited website is the responsibility of the directors; the work carried out by the assurance providers does not involve consideration of these matters and, accordingly, the assurance providers accept no responsibility for any changes that may have occurred to the reported performance indicators or criteria since they were initially presented on the website. 36 Format of this Quality Account This Quality Account has been produced using the NHS Foundation Trust Annual Reporting Manual for 2012-13, published by Monitor in March 2013. There is currently no requirement for the Priory Group to produce a Quality Account and, whilst we have broadly adhered to the guidelines produced by Monitor, the format of the Account does not directly follow that stipulated in the guidance. This decision has been taken to improve the readability of the Account and to exclude sections that are not relevant to the Priory Group. Deviations from the Monitor guidance are listed below: • Priorities for improvement 2013-14 are documented in Part 3 of our report. Performance against 2012-13 objectives have been fully documented in Part 2 (rather than split between Part 2 and 3 as suggested by the guidance) • Where applicable, areas of the Statements of Assurance that the guidance indicates to include in Part 2, have instead been included within appropriate sections throughout the Quality Account • The verbatim text suggested in the Monitor guidance regarding the CQC registration has not been included in this Account. The Priory Group is a national organisation and as such, is not only regulated by the CQC. The Regulatory compliance section of this Account details information for all of our regulators • Additional information has been included in Part 4 rather than within Part 3 – Other information to improve the clarity and readability of the Account • Views and opinions of third party organisations (including local Healthwatch organisations and Overview and Scrutiny Committees) are required to be presented under Monitor's guidance but are not applicable to the Priory Group Criteria which are not relevant to the Priory Group As an independent healthcare provider, the following criteria within the NHS Foundation Trust Annual Reporting Manual are not relevant to the Priory Group: • Schedule 2 row 1 • Schedule 2 row 2 • Schedule 2 row 3 • Schedule 2 row 4 • Information in relation to income conditional upon achieving quality improvement and innovation goals • Schedule 2 row 5 • Schedule 2 row 8 • Schedule 2 row 9 • Information relating to clinical coding 37 Data items from the NHS Quality Accounts content checklist not included in the Priory Healthcare division’s 2012-13 Quality Account The table below documents items which were not reported according to the NHS Quality Accounts content checklist annex within the NHS Foundation Trust Annual Reporting Manual for 2012-13 because they were not applicable to the services delivered by the division. Data guidance item Rationale for exclusion Care Programme Approach (CPA) service users, either receiving follow-up contact within seven days of discharge or having formal review within 12 months Minimising mental health delayed transfers of care Priory service users are generally discharged back to the NHS Percentage of service users readmitted to a hospital within 28 days of being discharged Admissions to inpatient services have access to crisis resolution home treatment teams No crisis resolution home treatment service provided by Priory hospitals Meeting commitment to serve new psychosis cases by early intervention teams No early intervention in psychosis service provided by Priory hospitals Data completeness: identifiers Data completeness: outcomes for service users on CPA Service user experience of community mental health services 38 No mental health minimum data set submission required for Priory hospitals Priory hospitals do not provide community mental health services Glossary of terms CAMHS Child and Adolescent Mental Health Services CPA Care Programme Approach CQC Care Quality Commission CQUIN Commissioning for Quality and Innovation framework: a national incentive scheme to improve quality and innovation in healthcare CSSIW Care and Social Service Inspectorate Wales GMC General Medical Council HIW Health Inspectorate Wales HoNOS Health of the Nation Outcome Scales HoNOSCA Health of the Nation Outcome Scales for Children and Adolescents MDT Multidisciplinary team MHA Mental Health Act (2007) NCISH National Confidential Inquiry into Suicides and Homicides by people with a mental illness: this inquiry features research into suicide, unexplained death and homicide by service users with a mental health condition across the UK. It produces regular national reports for England, Wales, Scotland and Northern Ireland NICE National Institute for Health and Care Excellence Never events Refers to serious, largely preventable service user safety incidents that should not occur if the available preventative measures have been implemented PARQ Priory Addiction Recovery Questionnaire: the outcome metric used by Priory addiction services to monitor abstinence following discharge from treatment PEG feeding Percutaneous Endoscopic Gastrostomy feeding: process of feeding via a tube that is placed through the skin and into the stomach Priory Carer Wellbeing Workbook Inspirational stories, poems and other thought-provoking content is included in this workbook, which aims to provide guidance and advice for the carer. A follow up wellbeing appointment is made with the carer by the nursing staff, and a care plan is drawn up to ensure that the carer is signposted to relevant services within the community QED Quality network for Eating Disorders QNIC Quality Network for Inpatient Child and adolescent mental health services SHA Strategic Health Authority: a now defunct commissioning body responsible for running or commissioning regional NHS services 39 Commissioning for Quality and Innovation framework The CQUIN framework accounts for 2.5% of the overall NHS contract in place across the Priory Healthcare division. The table below shows the overall schemes required for these targets to be achieved: Secure services South of England Specialist Commissioning Group West Midlands East Midlands North West North East Yorkshire and the Humber East Midlands Quality dashboard: implement the routine use of specialised services clinical dashboards Payment by Results (PbR) feasibility project: implement, review and feedback the requirements set out in the Feasibility Implementation Booklet. This includes: clustering, five care pathway indicators, benchmarking and reporting feasibility within a clear reporting structure Shared pathway: recovery and outcomes Shared pathway – implementing standard secure pathway: introduce and monitor key milestones on the care pathway in order to make the pathway more efficient and reduce length of stay User defined CPA standards: introduce and monitor the 20 service user defined CPA standards Optimise length of stay: understand the total care pathway and plan how it might work differently to optimise length of stay Access to specialised mental health services 25 hours of meaningful activity per week Eating disorder services Quality dashboard: implement the routine use of specialised services clinical dashboards User defined CPA standards: introduce and monitor the 20 service user defined CPA standards Optimise length of stay: understand the total care pathway and plan how it might work differently to optimise length of stay Implement the recommendations from the report Management of Really Sick Patients with Anorexia Nervosa (MARSIPAN) 40 South of England Specialist Commissioning Group Child and adolescent mental health services South of England Specialist Commissioning Group West Midlands East Midlands North West North East London Quality dashboard: implement the routine use of specialised services clinical dashboards User defined CPA standards: introduce and monitor the 20 service user defined CPA standards Optimise length of stay: understand the total care pathway and plan how it might work differently to optimise length of stay Education, training and meaningful activity: ensure that service user experience features activity which leads to effective rehabilitation and hence timely discharge Service user involvement in recruitment Patient flow annual report Patient safety thermometer: improve responsiveness to personal needs of service users Improve outcomes Optimise length of stay and improve outcomes Improve physical healthcare and wellbeing of service users Kent and Medway CQUIN scheme Complex care services Kent and Medway Patient safety thermometer: improve responsiveness to personal needs of service users Shared pathway – recovery and outcomes User defined CPA standards: introduce and monitor the 20 service user defined CPA standards Optimise length of stay: understand the total care pathway and plan how it might work differently to optimise length of stay Access to specialised mental health services 41 Future plans for CQUIN schemes in 2013-14 Going forward, the specialised commissioners have standardised the CQUIN schemes for 2013-14 and the following will apply to specialist commissioned mental health services. The Secure Recovery and Outcomes Group have already devised an action plan to look at all areas of the CQUIN requirements as below. Optimising pathways: all services Clarify admission and discharge pathway Design system to collect data on days spent at each stage for service user and specify variance, cluster, key issues, action taken and outcomes, as well as whether treatment targets were met Physical healthcare: all services Analyse national guidelines on performing health checks and ensure we are following them Ensure that each service user has a physical health care programme in place and it is recorded in the staying healthy section of CPA reports Look into checklist for coronary heart disease Ensure a diabetes and hypertension assessment is in place Document a health promotion programme for the hospital Care Programme Approach: all services Baseline audit of CPAs in Q1 Ensure CPA minutes reflect unmet need Provision of literacy and numeracy: secure services Baseline audit of current literacy, IT and numeracy opportunities Develop action plan for improvement in literacy and numeracy Improve service users' experience through innovative access to and for secure services: secure services Baseline audit of current use of technology Identify units in service users' pathways and share contact numbers Develop plan to work with other units Look at financial costs of new technology Develop local guidance on promoting the use of technology, which includes positive service user experience, testing before use, maintaining confidentially and governance, staff training Set date for roll out of new technology Provide information for service users, families and carers on new technology 42 Scope of data inclusion The 2012 -13 Quality Account provides an overview of the performance of the Priory Healthcare division against a wide range of internal measures and metrics, relevant to the division itself, or particular services and sites therein. This data may not represent the entire breadth of services or sites within the Priory Healthcare division; therefore, this appendix sets out the scope of data inclusion, as well as any relevant considerations (such as the methods by which samples were selected for analysis). Some sites were not fully integrated into the Priory Healthcare division’s systems for the entirety of the period and are therefore not included in all figures, although all sites are reflected in some way across the indicators used in this report. In this appendix, we will refer to two groups of sites, according to their implementation of the service user management system CareNotes. These are: CareNotes sites • • • • • • • • • • • • • • • • • • • The Priory Hospital Altrincham The Priory Hospital Brighton and Hove The Priory Hospital Bristol The Priory Hospital Cheadle Royal The Priory Hospital Chelmsford The Priory Hospital Dewsbury The Priory Hospital Glasgow The Priory Hospital Hayes Grove The Priory Hospital Keighley (previously the Willows) The Priory Hospital Market Weighton (previously Holme House) The Priory Hospital Middleton St George The Priory Hospital North London The Priory Clinic Nottingham The Priory Hospital Preston The Priory Hospital Roehampton The Priory Hospital Southampton The Priory Hospital Widnes (now closed) The Priory Hospital Woking Woodbourne Priory Hospital • • • • • • • • • • • • • • The Priory Grange Coombe House (now closed) The Priory Grange Heathfield The Priory Grange Hemel Hempstead The Priory Grange Potters Bar The Priory Grange St Neots The Priory Grange Sturt House The Priory Cloisters The Priory Highbank Centre The Priory Ticehurst House Chadwick Lodge Cefn Carnau Farmfield Thornford Park Ty Gwyn Hall • • • • • • • Highfields Longhouse (now closed) Princes Street Rookery Hove Rookery Radstock The Vines Ty Ffynu Non-CareNotes sites • • • • • • • The Priory Hospital Church Village (previously Caerlan) The Priory Hospital Aberdare (previously Newhouse) Avalon Beechley Drive Brynawel Caewal Road Egerton Road 43 Autism and Asperger’s syndrome services outcomes (p10) Analysis includes three of the four Priory Healthcare sites providing autism and Asperger’s syndrome services, specifically Rookery Radstock, Rookery Hove and Highfields. Data is based on a census of service users on 30-06-2012. The Priory Hospital Hayes Grove did not participate in the outcomes data collection involving the division’s wider specialist services sites and as such, no data was available for inclusion. Results of our service user satisfaction surveys 2012-13 (p12) Data was sourced from CareNotes sites only. Surveys are offered to all service users upon discharge, apart from within neuro-rehabilitation services, secure services and complex care services, where surveys are offered during an annual census period. Neuro-rehabilitation service user satisfaction data includes only The Vines and the Priory Highbank Centre, as other sites have not yet undertaken their service user satisfaction survey. Acute patients (acute mental health services, addiction services, eating disorders services and child and adolescent mental health services) are included where the following criteria is met: 1. The service user was discharged from the relevant service in the period from 1st April 2012 to 31st March 2013 inclusive 2. The service user submitted a paper satisfaction form having answered at least one question 3. The form was recorded on CareNotes ‘Agreement’ or ‘Satisfaction’ is defined as those people scoring 3, 4 or 5 on a 5 point scale. Detailed review of performance against 2012-13 objectives (p14) All relevant sites included, including non-CareNotes sites. Service user satisfaction – delivering value through clinical excellence (p18) Data was sourced from CareNotes sites only. Data covers all forms submitted in the reference period. Surveys are offered on discharge, other than for neuro-rehabilitation services, secure services and complex care services, where surveys are offered during an annual census period. Neuro-rehabilitation service user satisfaction data includes only The Vines and the Priory Highbank Centre as other sites have not yet undertaken their service user satisfaction survey. Outcomes – the success of our service users (p20) Data sourced from CareNotes sites only. Service users within an acute service (acute mental health services, addiction services, eating disorder services and child and adolescent mental health services) are included in the HoNOS/ HoNOSCA outcomes where the following criteria is met: 1. The service user has both an admission and discharge HoNOS completed and recorded on CareNotes 2. The service user is discharged in the period from 1st April 2012 to 31 March 2013 inclusive 3. At least nine of the 12 HoNOS measures are completed 4. Within addiction services, the service user stayed within the service for at least seven days The proportion of discharges included for each service are detailed below: Completion rates for the period are documented below: Acute mental health services: 88% Acute mental health services: 52% Addiction services: 62% Eating disorder services: 52% Addiction services: 74% Eating disorder services: 70% Child and adolescent mental health services: 71% Child and adolescent mental health services: 55% Summary of progress against 2012-13 Quality Indicators (p13) All relevant sites included, including non-CareNotes sites. 44 Data relating to other outcome measures has been included if the service user has at least an admission and discharge or review outcome score, with the latter score being in the period from 1st April 2012 to 31st March 2013 inclusive. Investing in staff, education and training (p22) All relevant sites included, including non-CareNotes sites. Regulatory compliance (p25) All relevant sites included, including non-CareNotes sites. Improving safety for our service users (p28) All relevant sites included, including non-CareNotes sites. Incidents which meet all of the following criteria are included: 1. The incident involves at least one service user as a participant (incidents involving more than one service user are counted as one incident) 2. The incident is reported on the Priory Group clinical governance system The number of ordinary bed days includes beds that have been contracted by an NHS commissioning body. Whilst under contract, these beds are considered to be fully occupied (regardless of service user occupancy). As a consequence, this may result in a slight understatement of the indicator result. Incidents leading to permanent harm are rated as having a "high" level of harm (second highest on a five point scale) and are defined as "any incident that appears to have resulted in permanent harm to one or more persons. Serious injury resulting in brain damage, loss of limb or impaired use". Incidents leading to the death of a service user are defined as those incidents which have resulted in the death of a service user, and are the highest grade on the five point scale. This is defined as: "any incident that directly resulted in the death of one or more persons". Both of the above have been manually checked to eliminate obvious errors. Improving safety for our service users (p28) and Continuous improvement in the delivery of our services (p30) The Priory Group implemented a new incident and complaint reporting system on 1st January 2012, including a revised incident management and reporting policy. Because of the inherent differences between the previous and new systems, it was not feasible to combine the data with our 2011-12 data. Therefore, where we present 2011-12 incident and complaint data, we have used the period 1st April 2011 to 31st December 2011. 45 The Priory Group of Companies is dedicated to helping people toeducation improve their health and wellbeing. From to hospitals, care homes and secure thethat Priory Groupfor ofpeople Companies offers We facilities, understand in order to achieve individually tailored, multidisciplinary treatment high quality clinical and educational outcomes, they programmes thoseprogrammes, with complexsuiting educational need individuallyfor tailored their needs or requiring acute, long-term and respite specific needs. mental healthcare. The Priory Group has established an unrivalled reputation for providing quality, inspiring The integrated strength of each serviceinnovation provides seamless value transition forservice the individual as they andadelivering for its users. With more progress between higher and lower dependency than 30 years of experience, the Priory Group treats over and 70 different conditions nationwide care across services. Thisthrough unique aapproach ensures every individual opportunity networkthat of over 275 facilities has thatthe support service to achieve the best possible outcomes and quality users’ health, care, education and specialised needs. of life with the Priory Group. As 85% of our services are publicly funded and delivered partnership with commissioners, our teams As 85% ofinour services are publicly funded and work within commissioning bodies across the country to delivered partnership with commissioners, our providework transparent pricing models and across evidence-based teams with commissioning bodies the country to provide transparent pricing models and care programmes. evidence-based care programmes. Priory Healthcare, 80 Hammersmith Road, London, W14 8UD PG04443/Jun13 About our group About our Group