QUALITY ACCOUNT 2012-13 1
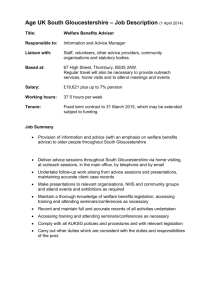
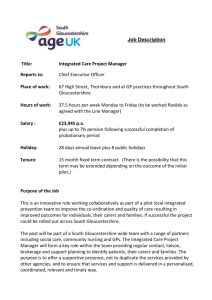
advertisement

QUALITY ACCOUNT 2012-13 1 Contents Section 1 What is a Quality Account? Statement from the Chair Statement of Directors’ responsibilities in respect of the Quality Account About our services Gloucestershire Care Services NHS Trust: Our Visions and Values Where our services are provided Section 2 Our priorities for clinical improvement in 2013-14 Clinical effectiveness – improving the quality of our care pathways Learning from experience Putting patients first 2 Section 3 Review of quality priorities for 2012-13 Using the expertise of staff through the Top 100 Ideas scheme Quality Improvements Infection Prevention and Control Medicines Management Safeguarding Gloucestershire Care Services Volunteer Programme Working with Communities – “Your Care, Your Opinion” Listening, learning and improving Patient’s stories Care Quality Commission 2012-13 Our compliance with Care Quality Commission standards Complaints and our learning Incident reporting 2012-13 Valuing our staff Quality and performance Same sex accommodation: declaration of compliance 2013-14 Our information governance (IG) toolkit attainment level Data quality NHS number and general medical practice code validity Financial statement How to contact us Amendments and additions to the document following feedback from our partners Appendix A - Statement from Gloucestershire County Council - Health and Care Overview and Scrutiny Committee Appendix B – Statement from Gloucestershire LINk Appendix C – Statement from Gloucestershire Clinical Commissioning Group Glossary 3 Section 1 Page 5……. What is a Quality Account? Page 6……. Statement from the Chair Page 7….… Statement of Directors’ responsibilities in respect of the Quality Account Page 8…… About our services Page 12…… Gloucestershire Care Services NHS Trust: Our Visions and Values Page 13…… Where our services are provided 4 ‘Gloucestershire Care Services NHS Trust is committed to working with you to provide high quality, local, health and social care’ What is a Quality Account? A Quality Account is provided to support openness and transparency across the NHS regarding the quality of services provided. This document may be used by patients and carers, stakeholders, the public and our staff, to assess the level of quality care we provide. Comparisons to other organisations may be made utilising some of the quality performance data within the document. 5 Statement from the Chair On behalf of Gloucestershire Care Services NHS Trust (the Trust), the Trust Board and our staff I am delighted to present our annual Quality Account. This provides us with an opportunity to restate our commitment as an organisation to continue to improve the quality of the services that we provide and to demonstrate the achievements of our staff. Throughout this reporting period (1st April 2012 to 31st March 2013), we have continued to focus on quality improvement across all our services. During 2012-13 the Trust operated as an arm’s length provider within NHS Gloucestershire as progress to establish a Community Interest Company met with legal challenge. In considering the future of the organisation, Commissioners called for a response that did not dilute the market for care in Gloucestershire and that would deliver its strategic vision. The plan to establish Gloucestershire Care Services (GCS) as an NHS Trust was agreed and the transition to Gloucestershire Care Services NHS Trust took place on the 1st April 2013, following significant preparation and staff involvement. The reflective “look back” aspects of this document relate to our predecessor organisation (NHS Gloucestershire Care Services), whilst the “look forward” sets out our objectives and commitment for Gloucestershire Care Services NHS Trust. Despite the significant organisational change and period of uncertainty for the future, staff have continued to be focussed and work hard, especially in the area of quality and performance. They are to be congratulated and should be proud of the high standards they have achieved. Continuously improving the quality of our services remains our primary focus for the Trust, through a growing portfolio of quality improvement initiatives aimed at enhancing the safety, experience and outcomes for all our patients. Our Board ensures that matters relating to care quality remain high on its agenda and will throughout the coming year ensure that lessons learnt from the concerns raised regarding Mid Staffordshire NHS Trust, are used to review our practices. We recognise the importance of providing assurance to our partners and users of our services, that the care we deliver is of a high standard, as safe as possible and achieve good clinical outcomes. We welcome the comments and interest we have received from our partners and stakeholders and wherever possible have incorporated these into this final draft. To the best of our knowledge, the information presented to you in this Quality Account is accurate and provides a fair representation of the quality within our organisation. Ingrid Barker – Chair 6 STATEMENT OF DIRECTORS' RESPONSIBILITIES IN RESPECT OF THE QUALITY ACCOUNT The Directors of the Trust are required under the Health Act 2009, National Health Service (Quality Accounts) Regulations 2010 and National Health Service (Quality Account) Amendment Regulation 2011 to prepare Quality Accounts for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporate the above legal requirements). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: • • • • the Quality Accounts presents a balanced picture of the Trust’s performance over the period covered; the performance information reported in the Quality Account is reliable and accurate; there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; the data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Account has been prepared in accordance with Department of Health guidance. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board 28.6.2013……….Date.............................................................Chair 28.6.2013……….Date............................................................Deputy Chief Executive 7 About our services Gloucestershire Care Services NHS Trust (the Trust) provides high quality accessible and responsible community and specialist NHS services across Gloucestershire and employs in excess of 2,800 staff. Staff include Nursing, Medical, Dental, Allied Health Professionals, Support Staff, Administrative And Clerical Workers. Having worked closely with colleagues in social care for many years, we have now integrated adult health and social care services and manage approximately 800 staff – Social Workers and Reablement Workers on behalf of Gloucestershire County Council. We deliver community-based health and social care to people of all ages across Gloucestershire covering a population of approximately 600,000 people. These services are delivered in a variety of settings including people’s homes, community clinics and community hospitals. Throughout 2012-13 a total of 54 different healthcare services were provided by the organisation. Each year the organisation’s staff engages in more than two million contacts with patients and other service users. Providing Services across Gloucestershire 1. Children and Young Peoples’ Services Brings together all the specialist community services for children and young people across Gloucestershire and offers a co-ordinated approach for child health as well as delivering the universal childrens’ services of Health Visiting, School Nursing and the Neonatal hearing screening service. 2. Locality Based Services for Adults Provides a range of services for the local communities within the county including community based care and hospital admission avoidance, District Nursing, Adult Social Care, Community Podiatry and therapy services for older people. Our services also provide care within seven community hospitals which includes minor injury units, outpatient and inpatient care. 3. Specialist Services • • • • • Community Dental Services Provide a range of specialist dental services across Gloucestershire Sexual Health Services Provide a range of sexual health and genito-urinary medical services across the county. Specialist Nursing including Tuberculosis, Parkinson’s Disease and Heart Failure. The clinical services are supported by a range of corporate functions such as Human Resources, Finance, Performance, Governance And Risk Management. Patient Advocacy and Liaison Service (PALS) and the Patient Experience Service provide liaison with users, their families and carers. 8 4. Integrated Community Teams GCS and GCC have worked hard to integrate services being delivered across Gloucestershire, based on our joint commitment, as set out in the July 2012 Concordat and Business Case to the integration of health and social care services in Gloucestershire. The intentions have been: • • To improve health and social care outcomes for adults in Gloucestershire To deliver operating efficiencies across the County against challenging economic and demographic trends Evidence from national studies provide a consensus that integration between health and social care provides significant benefits to service users, staff and organisations including: • • • • • Improved overall access to services Shortened time from identification of need to delivery of community service Simplified decision-making processes Increased efficiency of processes of assessment Reduction of communication failures by reduction of patient handover Community based workers who deliver health and social care to adults in the community, including Social Workers, Physiotherapists, Occupational Therapists, District Nurses and support staff for each profession, are now integrated and largely co-located into integrated community teams (ICTs) organised within three locality structures; Gloucester & Stroud, Cotswold and Cheltenham; Forest of Dean & Tewkesbury to ensure a local focus is maintained. An Integration Programme has been in place since 2011, including six work streams that are responsible for providing our Integrated Care Teams with the ability to work across organisational and professional boundaries. These workstreams include HR and Workforce Development, Finance, Performance, IT, Accommodation, and Governance. Their plans have focused on looking at what practical changes are required to the way our organisations work to allow integrated working, with significant change already delivered. In addition to this, there have been a number of service improvement projects, aligned to and enhancing integration. These have included: • • • • • Referral Management Centre developments The Customer Journey Project Living Well Review of the Self Directed Support process South Cotswold and Gloucester pilots with the intention to enhance Integrated Community Teams and to support the work of avoiding inappropriate hospital admissions. 9 Benefits to patient/service user: Faster recovery at home with support Patient is back in the community with their local support network ie. Family friends, carers, GPs and the voluntary sector. Increased independence and quality of life. Benefits to care provider Less duplication through integrated care. Bringing care closer to home. Make best use of hospital based services. (left) Senior reablement worker and community therapist working with a patient in his home 10 Full independence through co-ordinated care After a stay in hospital to recover from a fall, Mrs B had been discharged home and was receiving four calls per day for homecare support. A social worker from the local community team visited Mrs B to complete a review to see how she was progressing and whether or not additional support was needed. Throughout her adult life, Mrs B has lived with a disability where paralysis affects one side of her body. An independent and resilient lady, Mrs B raised her family and, in recent years, nursed her first and her second husband through long illnesses until they died. Ashleigh Intermediate Care Centre Team (back row) occupational therapist, senior reablement worker, unit lead, care leader, community nurse (front row) social worker, district nurse. From the first assessments and learning about Mrs B’s past, it became clear to the social worker that Mrs B has developed good coping strategies over the years to solve the challenges of daily living with a major disability. Mrs B, however, had not been out of her home since her fall and she was fearful of driving again. Her family expressed concerned about her catheter and its possible removal, and Mrs B’s need for exercise and ongoing support. After the social worker talked through the issues with Mrs B, the homecare agency and occupational therapist, it was agreed that the reablement team would support Mrs B for the morning and night calls, with the homecare agency continuing to support the lunch and evening calls. Advice and support were given to make sure that Mrs B could move safely around her home with adjustments to existing equipment. Over a number of weeks, and through the work of the occupational therapist and reablement workers, Mrs B was supported to become more independent and confident in daily tasks, such as washing, dressing, meal preparation and cooking. The lunch-time visit from the homecare agency was replaced with a reablement visit to support Mrs B in regaining these skills further. To help Mrs B better manage her catheter - with a view to removing the need for a catheter altogether – the team’s district nurses became more closely involved in her care. Different catheter equipment proved unsuccessful at home so, with the support of her social worker, Mrs B was admitted to Ashley Intermediate Care Unit in Cheltenham. After three weeks of close supervision by the Unit’s district nurse and other support staff, Mrs B was finally able to have her catheter removed. The impact on Mrs B’s quality of life has been dramatic, and she no longer needs any help at home from carers. 11 Our Vision and Values Our Strategic objectives To secure, develop and deliver innovative, high quality community based services meeting the needs of users To integrate health and social services To develop and strengthen partnerships with communities To support, develop and involve our staff To strengthen our excellent reputation To deliver our contract commitments and provide value for money 12 Where our services are provided “The Community Hospital had a good friendly supportive attitude and that services the ward manager Where our are provided was leading it well and that we wish to thank them all for what they did for my husband.” “The Expert Patient Programme made me realise that people do care and there is help and they will help you to deal with your problems.” 13 Section 2 Page 15……Our priorities for clinical improvement in 2013-14 Page 17…..Clinical effectiveness – improving the quality account of our care pathways Page 17….. Learning from experience Page 18……Putting patients first 14 Introduction In order to identify our priorities for the coming year, in Gloucestershire Care Services NHS Trust we have considered the four aspects of quality, safety, effectiveness and experience. We have used the information available from patient feedback, incident reports and from our staff, to identify the key workstreams for the coming year. Our priorities for clinical improvement in 2013-14 The implementation of the Safety Thermometer has formed a key part of our patient safety plans during 2012-13 and evidencing improvement will continue to be a priority during 2013-14. This is a national programme aimed to reduce harm from: • • • • Hospital and community-acquired pressure ulcers (also known as pressure sores) Falls Urinary tract infections (UTIs) in patients with catheters Blood clots (deep vein thrombosis and pulmonary embolism) The healthcare complications resulting from these issues are recognised across the NHS. Harm from pressure ulcers, falls, urinary catheters and blocked clots, is estimated to affect over 200,000 people each year and the direct costs to the NHS estimated at over £430 million per year. Gloucestershire Care Services is working with other NHS trusts to improve patient safety as part of this national programme. We aim to eliminate all four causes of harm, for every patient, by developing safer systems for in patient and community settings. The programme encourages organisations to address safety issues from the patient’s perspective and adopt an integrated approach across teams and departments to minimise the risk of the four causes of harm. Measuring for improvement Measuring harm-free care from the patient’s perspective is ambitious and is supported by the use of the safety thermometer which is a tool that measures, monitors and analyses causes of patient harms and harm-free care. This enables frontline clinical teams to survey their patients every month, measure the four causes of harm and will build evidence to enable monitoring of their own safety improvement. The use of the tool in 2012-13 has highlighted themes for further quality development including: • • • Catheter care Antibiotic prescribing Review of the escalation threshold for the Early Warning Trigger Tool (QuEST) 15 Data collected from incident reporting is also used to influence improvement work, especially for patients who have fallen or who have pressure ulcers. As we repeatedly measure our patients for harms, we will build a picture of improvement. We will monitor how rapidly this is happening to establish ongoing patient safety work is making a difference to patient care and experience. How this will be achieved CRITERION ACTIONS CRITERION MONITORING AND REPORTING CRITERION ACTIONS Establishing baseline information Using the NHS Safety Thermometer (ST) to measure harms at the point of care enabling clinical staff to know the number of: • Pressure ulcers • Falls • Catheter-associated urinary tract infections • Proportion of patients that are free from harm • Blood clots • Complete the ST for 100% of eligible patients every month for the four harms to establish a baseline. • Use that baseline line information from the safety thermometer and triangulate with incident reporting and case note review. Goal – where do we want to be? We will use the work from the safety thermometer to support the GCSNHST objective to deliver care free from avoidable pressure ulcers, falls, urinary catheter infections and blood clots. • Safety Thermometer data is reported in the quality and performance part of the Trust Board, using the quality dashboard to measure improvement. • The patient safety report is presented to the Integrated Governance Committee • Groups that drive these improvements are: Falls; Pressure Ulcer Group; Quality and Safety Group; Care Quality Forum. • Progress is included in the locality monthly reports and shared with local governance committees. How the goal will be achieved As part of the safety thermometer work, improvement will be tracked over time. The clinical teams are committed to effectively deliver care, free from harm to patients. This is not about starting again but building on successes and integrating within current ways of working. • Completion of safety thermometer on a monthly basis. • Use of the early warning trigger tool on all our inpatient areas. • Risk assessment. • Audit of catheter care plans. • Audit of antibiotic prescribing compliance. • Medicines review for all in patients. • Nutrition and hydration including protected mealtimes in inpatient areas. 16 Clinical effectiveness – improving the quality of our care pathways Our aim is that service users and their families are supported at home for as long as possible, are well informed about how to best manage their health and have key contact details to access responsive support and advice. Rationale Clearly described pathways of care, developed in partnership with other providers within Gloucestershire will support the delivery of compassionate care throughout the care journey by reducing the number of handovers between teams and provides clear support and guidance to patients and carers as to where to access support. Baseline The focus for pathway development in collaboration with our partners for in the coming year will be: • Support for those with dementia • Respiratory care • Care for the frail older person • Reablement pathway Goal Our aim is that service users and their families are supported at home for as long as possible, are well informed as to how to manage their health and care needs and have key contacts for support and advice. Monitoring and Reporting The Transforming Local Care Committee will oversee and monitor the development of long term condition pathways. Learning from experience Rationale Listening to and learning from the experiences of service users, their families and carers is critical if we are to continue to improve the quality of our services. Baseline The results from the “friends and family test” which forms part of our service user survey programme will provide the baseline from which to develop our work programme. Goals • Together with the Your Care, Your Opinion Group develop our user experience strategy. • Review the methods used to gain views from users and carers and develop a plan for gaining the views of those who may not respond to traditional survey methods and consider for example focus groups, use of technology. • To add the friends and family tests within the staff survey. 17 Monitoring and Reporting The Your Care, Your Opinion Group which includes in its membership the third sector partner agencies and lay members, will monitor progress against our action plan and reporting will form part of experience reports to the Integrated Governance Committee which provides assurance to the Board. Putting patients first The Trust Board are committed to effectively learning from the Public Inquiry relating to the Mid Staffordshire NHS Foundation Trust and supporting documents. We are committed to creating a culture that puts patients at the centre of all we do and ensuring we support our staff to do so. Whilst the reports focus on inpatient care and nursing, our staff are saying that ensuring patients and their families are treated with dignity and respect is everybody’s business. We have reflected on the issues raised and held a number of conversations with staff groups across the county to insure our actions reflect the staff view of the impact of the learning on our organisation. We have developed a plan that was discussed at our Board on the 14 May 2013, and addresses actions in relation to the key aspects of: • • • • • Prevent problems Detect problems quickly Take action promptly Ensure robust accountability Ensure staff are trained and motivated Our progress will be reported both to our Staff Forums and to the Integrated Governance Committee and measured together with the feedback from both patient and staff surveys. This will also be reflected in our Quality Strategy that is being prepared in partnership with clinicians and stakeholders and will be reported in the Quality Account 2013 -14. 18 Section 3 Page 20…..Summary review of quality priorities for 2012-13 Page 25…..Using the expertise of staff through the Top 100 Ideas scheme Page 26…..Quality improvements Page 27…..Infection Prevention and Control Page 28…..Medicines Management Page 30…..Safeguarding Page 31…..Gloucestershire Care Services Volunteer Programme Page 32…..Working with Communities – “Your Care, Your Opinion” Page 33…..Listening, learning and improving Page 34…..Patient stories Page 35…..Care Quality Commission 2012-13 Page 36…..Our compliance with Care Quality Commission standards Page 37…..Complaints and our learning Page 39…..Incident reporting 2012-13 Page 40…..Valuing our staff Page 44…..Quality and performance Page 46…..Same sex accommodation: declaration of compliance 2013-14 Page 46…..Our information governance (IG) toolkit attainment level Page 47…..Data quality Page 47…..NHS number and general medical practice code validity Page 48…..Financial statement Page 49…..How to contact us Page 50…..Amendments and additions to the document following feedback from our partners Page 51…..Appendix A - Statement from Gloucestershire Clinical Commissioning Group Page 53…..Appendix B – Statement from Health and Care Overview and Scrutiny Committee Page 55…..Appendix C – Statement from Gloucestershire LINk Page 57…..Glossary 19 Summary review of our quality priorities for 2012-13 Commissioning for quality and innovation (CQUINs) What are CQUINS? CQUINs are projects agreed between the Commissioners (who buy our services) and the Trust. These projects are established to improve clinical care delivery or the processes that support clinical care. A proportion of Gloucestershire Care Services’ income (£1,952,975 in 2012-13) was conditional on achieving quality improvement and innovation goals agreed between the Trust and our commissioning through the CQUIN payment framework. The Trust received full payment of this income. Patient experience in our community hospitals In April 2012 we said…. Carrying out patient satisfaction surveys and monitoring the results helps to ensure that all service improvements are driven by service user feedback and therefore focused on improving patient experience. Baseline Using the learning reported from the 2011-12 survey will be used to improve or maintain both the quality of service reported and the response rate. Reporting of our progress Regular update reports have been provided to the Information Governance Committee and the Board. Achieving our goal Implement of action plans based upon survey findings 2011-12. Achievement by March 2013 The response rate increased to 420 from the baseline of 234 in 2011-12. The table shows the percentage of positive responses to the five key CQUIN questions. Questions Did the service meet your expectations? Were you involved as much as you wanted in planning your treatment and care? Were hospital staffs available to talk about worries and concerns? Yes 2010/11 Not asked Yes 2011/12 2012/13 Not formally asked 86% 82% 80% 86% 91% 80% 90% How would you rate the privacy on the ward? 61% - very good 27%- good 12% average 60% - very good 32% - good 8% - average 66% - very good 28% - good 5% average How likely is it that you will recommend this service to friends and family? Not asked Not asked 93.2% 20 Reducing risk of Venous Thromboembolism (VTE) In April 2012 we said…. Venous Thromboembolism (VTE) is a significant cause of death in hospitalised patients and adversely affects the quality of life of patients. This initiative will support VTE prevention with the aim of reducing the risk of patients developing the condition during and after their time as an inpatient, building on the quality achievement in the previous year. Our goal By March 2013 90% of all inpatients will have been assessed for their risk of VTE and 90% of those assessed as being at risk will have received appropriate prophylaxis. How we monitored and reported our progress We did this by monthly reporting as part of the quality and performance dashboard. Achievement by March 2013 The practice of providing VTE risk assessment for patients has been successfully embedded into the inpatient areas. The targets for both aspects of this CQUIN have been exceeded. • • • 97.5% of patients had a risk assessed completed 95% of those at risk received prophylaxis Zero attributable VTE’s were identified Falls prevention In April 2012 we said…. Falls have a major impact on quality of life, health and healthcare costs. Reducing falls in hospital will reduce unnecessary increased length of stay. Our goal 90% of patients will have a falls risk assessment within 24 hours of admission and where necessary a care plan developed to detail how we will reduce the risk of falling. How we monitored and reported our progress Monthly update reports given through the quality and performance dashboard. How we achieved our goal We ensured that all the community hospital teams carried out falls risk assessment for all patients. Where a patient is at potential risk, a care plan and patient information concerning falls prevention is provided. Achievement by March 2013 We exceeded the 90% target and evidenced that 98% of patients received a falls risk assessment within 24 hours of admission. For those at risk of falls, 99% had a falls care plan in place within 24 hours of admission. 21 Improving care for those with Dementia In April 2012 we said…. Improved screening for signs of dementia and then appropriate referral. This aides diagnosis and the provision of early treatment and support. Our goal 90% of all those aged 75 years and over admitted to a community hospital will have screening and where appropriate be referred for further assessment. How we monitored and reported our progress This was actioned by monthly reporting through the quality and performance dashboard. Achievement by March 2013 We exceeded the target and achieved initial screening assessment for 98% of eligible patients. Of this group 90% had multi-disciplinary intervention within 3 working days. Introduction of the Safety Thermometer In April 2012 we said…. Safety Thermometer (ST) provides an effective measure and benchmarking of four key areas of harm. Our goal By March 2013 all community hospital ward teams will be submitting data to the national database. How we monitored and reported our progress This was actioned by monthly reporting through the quality and performance dashboard. How we achieved our goal The clinical teams supported by a clinical lead, undertook a monthly census which resulted in information collated by the Performance Team being submitted to the national database. Achievement by March 2013 The target was exceeded with all inpatient and community teams undertaking the monthly census and reporting on the national database by the end of the year. Patient experience escalator In April 2012 we said…. We want to ensure that services provided promoted shared decision making and ensured all were treated with kindness, dignity and respect. Baseline Data from quarter 1 (April-June) - we used the friends and family test to identify good practice. 22 Our goal • To develop and implement a programme of observational audit. • Evidence learning from the 2011-12 survey • Demonstrate leadership from point of care to chair How we monitored and reported our progress This was actioned quarterly through reporting through the quality and performance dashboard. Achievements by March 2013 • 93.2% of those that use our services would recommend us to their friends and family • Action plan from 2011-12 audit agreed and monitored by the Contract Quality Group • Observational audit in place • The use of patient stories developed with the support of our expert patient programme Improving maternal mental health In April 2012 we said…. Ante and post natal screening offered to women can support early intervention and appropriate care. Our Goal That through the use of the maternal mental health pathway we improve outcomes for women with mental ill health during pregnancy and for up to a year following birth Baseline In quarter 1 (April- June) the baseline data was gathered and the number of staff requiring training was identified. How we monitored and reported our progress Through quarterly reporting in the quality and performance dashboard. Achievements by March 2013 • 75% of staff requiring training undertook the appropriate programme. • 95% of women were offered screening. • 83% had initial screening question • 19% had onward referral at end of inpatient stay Improve the number of referrals to the Single Point of Clinical Access (SPCA) from GWAS In April 2012 we said…. Increasing the number of referrals to the SPCA will support effective care close to home and reduce acute admissions. 23 Our Goal By the end of the year we will have received 100 referrals to the SPCA from the Great Western Ambulance Service (now South Western Ambulance Service NHS Foundation Trust), by developing effective processes to work in partnership. How we monitored and reported our progress Through the quality and performance dashboard. How we will achieve our goal Working in partnership with the ambulance service will look at pathways to support patients as close to home as possible and in doing so avoid unnecessary hospital admission Achievements by March 2013 We achieved a total of 236 referrals to our SPCA therefore exceeding our target. Provision of seven day services In April 2012 we said…. We aim to firstly enhance the process in community hospitals throughout the week and by doing so, support early discharge from acute hospitals, and secondly prevent unnecessary acute admissions and enable discharge home or to care home seven days a week. Our Goal To develop effective processes supported by clinical teams to ensure where safe to do so patients may be admitted or be discharged from community hospitals seven days a week. How we monitored and reported our progress By monthly reporting through the quality and performance dashboard. How we achieved our goal The goal was achieved through partnership working and our developing Integrated Community Teams to ensure where safe to do so patients are cared for close to home and that unnecessary admissions to acute services are avoided. Achievements by March 2013 • 44% of patients admitted to a community hospitals came directly from home with a further 8% admitted following initial assessment within an acute setting • 17% of total admissions take place over the weekend • 13.8% of discharges take place over the weekend Improve care and support at end of life In April 2012 we said…. That effective planning and communication can enable those at the end of life to be cared for in their place of choice and better support their families and carers. 24 Our goal To effectively utilise the Liverpool Care Pathway (LCP) to record conversations with patients and their families, aiding communication and supporting joint planning and informed choice based on the best evidence. How we monitored our progress Benchmarking data was collected through the clinical audit process in quarter one to establish the number of LCPs in use and if preferred place of care at end of life was recorded How we achieved our goal The negative publicity surrounding end of life care and the LCP in particular brought considerable challenge to this work. Nursing staff supported patients in understanding and ensuring informed consent around care planning and respected choice where patients or families may opt not to use an LCP to record care. Whilst the CQUIN measured LCP use the focus of staff remained on improving care and enabling choice around preferred place of care, ensuring this was effectively document whether or not the LCP was used. Achievements in March 2013 85.5% had LCP in use and 62.15% had preferred place of care at end of life recorded. Using the expertise of staff through the Top 100 ideas scheme In April 2012 we said…. We would challenge staff to submit ideas and innovation that would benefit staff and patients. Our goal Identify the top three ideas then submit these to be supported to implement their plans. How we achieved our goal We worked in partnership with Bristol Business School who led workshops and helped prepare the shortlisted to present to the “Dragon’s Den” panel. We involved our staff forums who undertook the shortlisting. Achievements in March 2013 The joint winners were:Emma Cronin-Preece & Linda Knight Text servicing for the community accessing the Public Health Nursing Service Would help to ensure effective use of staff time as contacts will be requested by clients. Text messaging enhances access in a rural area, those with poor reception and for those who prefer text messaging. Teenagers and parents will have enhanced access to Public Health Nurses and private and confidential advice at their convenience. Ollie Crawford-Paul Swap shop for surplus or stock approaching its use by date Introduction of a swap shop for staff on the intranet would benefit staff, patients and the organisation as a whole providing a means for efficiently redistributing unwanted stores 25 items. It would be particularly useful to the smaller units where the minimum unit of issue of some stock is too large for all the items to be used within their use by date, this will reduce wastage and costs. James Clapp Children’s physiotherapy smart phone app, enabling parents and medical professionals to gain instant information Children, parents, health professionals including GPs, Health Visitors, and Physiotherapists would benefit. Parents and children will have instant access to information on common conditions seen in childhood and the best forms of self-management or accessing treatment. (left to right) Rob Graves Non-Executive Director, James Clapp, Linda Knight, Emma CroninPreece, Ollie Crawford-Paul Next Steps So many great ideas were developed which we would not wish to lose. Many of those are being supported by managers of the teams that submitted their ideas, to trial their ideas in practice. The top three finalists will be supported to develop their ideas and plan the implementation and have identified mentors identified to support them in this process. Quality improvements Gloucestershire Care Services NHS Trust aims to embed the four key aspects of quality, safety, effectiveness and experience, in every day practice. Each member of staff takes all opportunities to consider how they can ensure care provided is safe, effective and delivers a positive experience and where we do not get that right we are open and honest and learn from feedback. 26 Infection Prevention and Control Infection prevention and control is a critical part of patient safety across all services and aspects of care. The commitment demonstrated by our care and hotel services staff, has enabled the Trust to evidence excellent progress in this important area exceeding our targets in each of the following three areas. Number of C.difficle infections Number of MRSA bacteraemia Percentage of staff completing infection prevention and control training Tolerance ≤ 24 0 79.5% Achieved 17 0 84.5% A comprehensive Infection Prevention and Control Annual Report will be presented to the Trust Board in November 2013 and made public through our website. Across our community services monthly audits of hand hygiene practice are undertaken using the adapted Lewisham observational tool observing hand hygiene practice within a clinical area over a period of 20 minutes. Example of a hand hygiene report (based on percentages): Annual average score for observational hand hygiene audits = 98% compliance The Patient Environment Action Team (PEAT) The annual programme of PEAT inspections focuses on the non-clinical aspects of care quality. The results of the 2012 inspections are detailed in Table 2 below and evidence that hospital teams have all maintained or improved on the score achieved in 2011. 27 Moreton District Hospital was not inspected at this time as the visits took place just prior to the move to the new North Cotswold Hospital. This site will be part of the programme of visits for the coming year. Environmental issues identified at The Dilke Hospital caused the team to assess privacy and dignity as “good”. The PEAT team membership includes a member of the infection prevention and control team, and the results clearly demonstrate continued improvement in quality standards. Hospital Environment Food Privacy & Dignity Cirencester Hospital Excellent Excellent Excellent Tewkesbury Hospital Excellent Excellent Excellent Dilke Memorial Excellent Excellent Good Lydney & District Excellent Excellent Excellent Stroud General Excellent Excellent Excellent The Vale Hospital Excellent Excellent Excellent TABLE 2 Moving from PEAT to Patient Led Assessments of the Care Environment (PLACE) The ending of PEAT inspections and their replacement by new patient led inspections, to be known as Patient-Led Assessments of the Care Environment or PLACE was announced by David Cameron on the 6 January 2012. The focus of the revised process will continue to be cleanliness, buildings/facilities, privacy and dignity, and food, but there are a number of changes to the detail of the assessment, the scoring methodology and the assessment process and crucially the number and responsibilities of the patient representatives. The Trust will be part of this new process in 2013 and will be reporting on the outcome within future Quality Accounts. Medicines Management Prescribing medication is the most common healthcare intervention. Medicines management governs the way in which medicines are selected, procured, prescribed, administered and reviewed, in order to optimise the contribution made to producing informed and desired outcomes of patient care. Getting the use of medicines right or optimising the use of medicines is essential to improve the outcome for patients. The Head of Medicines Management is a member of the Countywide Antimicrobial Stewardship Group which has a clear work plan to improve antibiotic prescribing and reduce the risk of resistance. A monthly antibiotic audit was introduced across all on inpatient wards to assess 5 key elements of antibiotic prescribing. The results of this audit are published on the monthly dashboard and non-compliance followed up with individual prescribers. Prudent and appropriate antibiotic prescribing will continue to be a focus through 2012-2013. 28 An Accountable Officer for Controlled Drugs has been appointed to meet the legislative requirements of establishing an NHS Trust. This person has responsibility for the safe and effective use of controlled drugs across the Trust. A very successful Medicines Management Conference was held in November 2012. It was attended by approximately 100 staff and covered key areas including the legal aspects of prescribing and administration, the rights of medicines administration, record keeping and antibiotics. It is hoped to repeat this in future years. A Medicines Management training program for clinical staff is currently being run by the clinical pharmacist at Cirencester Hospital. This event has been welcomed by staff and it is planned to roll this out across all our services. During this year a review has taken place of all medicines held as stock on the inpatient ward. The purpose of the review was to ensure evidence based prescribing was being adhered to with the countywide drug formulary and to provide continuity of care across all inpatient sites. The review has reduced the amount of inappropriate stock being held on wards and reduced wastage. This review has dovetailed with the introduction of bedside medicine lockers which supports a personalised care and maintenance of independence during an inpatient stay. The organisation continues to support non-medical prescribing to support service development and improve patient and care experience. During 2012-2013 10 registered nurses started their Independent non-medical prescribers through local Universities. We continue to provide a range of educational sessions to support Non-Medical Prescribers programme across the organisation meet their continuing professional development needs. In the future the use of e-learning will be considered to allow a wider range of topics to cover. Plans for 2012-13 include a focus on medicines management training and missed dose audits. 29 Safeguarding In line with both national and local drivers this last year has seen considerable movement towards a more integrated approach to Safeguarding Adults and Children. This has culminated in the formation of a joint operational group, and both named nurse leads are now co located to facilitate closer working. The Trust continues to increase the numbers of staff who have accessed training relevant to their role and now has 16 trainers who have completed a train the trainer course hosted by GCC to enable the delivery of foundation level training within our localities. To increase the Safeguarding profile a Safeguarding Children’s newsletter has been developed, which will be replicated for Safeguarding Adults and the first of a series of poster campaigns ‘No Pressure Ulcers’ was run with positive feedback from clinical staff. Both Adult and Children’s Services continue to fully participate in multi-agency meetings within the county. The Named Nurse for Safeguarding Children and specialist safeguarding team provide supervision to all health staff involved in child protection cases. Health visitors and school nurses as front line practitioners working with children and families receive specialist safeguarding supervision. In addition group supervision is provided to staff with Sexual Health Services and Minor Injury Units. The Director of Nursing represents the Trust on both the Gloucestershire Safeguarding Children’s and Adults Boards and key professionals attend the sub committees. There is an ongoing robust programme of local and multi-agency safeguarding children training for staff caring for children and vulnerable adults. Declaration In April 2012 the Trust published a declaration about how the Board assures themselves that safeguarding arrangements are in place. The Trust Board continues to take its safeguarding responsibilities very seriously. • • • • • Gloucestershire Care Services NHS Trust meets the statutory requirement with regard to the carrying out of criminal records checks (DBS) Disclosure Barring Service. Child protection policies and systems are up to date and robust including a process for following up children who miss outpatient appointments and a system for flagging children for whom there are safeguarding concerns. All eligible staff are required to undertake safeguarding training and attendance is monitored in line with mandatory training policy and reported to the Trust Board. In addition, a review of other training arrangements will be completed and will incorporate the emerging recommendations from the national review of safeguarding training. The named doctor, named nurse responsible for safeguarding are clear about their roles and have sufficient time and support to undertaken them. The Executive Director of Nursing is the Board level Director for safeguarding. 30 Safeguarding - Preventing Pressure Ulcers 2012 /13 marked the launch of several new initiatives to support existing activity relating to Pressure Ulcer (sore) prevention. As part of our participation in the South West NHS Patient Safety forum a change in our risk assessment and related clinical records resulted in much clearer information relating to level of risk and prevention strategies, that have been positively received by staff. All pressure ulcers are reported via our electronic incident reporting system, and are subject to an initial investigation by the Named Nurse Safeguarding (Adults). The incidents are reported on the performance dashboard, which demonstrates a reduction in the number of pressure sores acquired while an individual is in the care of GCS. Linked to this was the development and launch of a Safeguarding and Pressure Ulcers policy which clearly described employee’s responsibilities and a countywide multiagency approach to management. This policy is now reflected in a countywide policy hosted by GCC and has also been adopted by partner health agencies. The Tissue Viability Team also hold training and education sessions. Gloucestershire Care Services Volunteer Programme Volunteers work across our organisation providing valuable support to improve the patient experience in hospitals, clinics and within a patient’s own home. They help to build a stronger relationship between members of the local community and our services, helping to tackle health inequalities and promoting healthy lifestyles. Patients benefit from improved well-being, higher selfesteem, lower levels of social inclusion and improved self-management skills. The Trust Volunteer Service policy was written and published in April 2012, which included some work collating a database of the volunteers in the organisation. Prior to this volunteering was managed in each locality and there were no centralised records of the volunteers in the organisation. The policy is due for review April 2013. A volunteer co-ordinator was appointed on an 18 month secondment with the purpose of supporting volunteers with induction and training as well as ensuring all essential employment checks were undertaken to protect the patient. A volunteer database was compiled which includes records of Disclosure Barring Service (DBS) checks. Since September the Volunteer Coordinator has been working on updating this list of volunteers and ensuring all those who need them have a current Disclosure and Barring Service check (previously CRB checks). 31 Total Number of volunteers September 2012 Total Children's services Cirencester Hospital Expert Patient Programme Forest Hospital North Cotswolds Hospital Podiatry Speech and Language Therapy Stroud Hospital Stroud Physiotherapy department Tewkesbury Hospital Vale Hospital 278 20 84 5 7 19 1 47 12 1 44 0 December 2012 326 17 95 7 29 29 3 42 18 0 45 25 March 2013 358 18 101 7 29 29 3 47 31 0 54 22 Since September the following processes have been drawn up to help support those who wish to offer their time to volunteering: • • • • • • Advertising Recruitment (including Volunteer Agreement) Person specification and task lists Induction (including corporate and local induction, handbook and welcome pack) Training Problem solving guidance There is a volunteering page on the organisation website for the public to find out about volunteering for the organisation and contact details for enquiries and to apply. The e-mail address that has been set up to receive general enquiries and a point of contact for the service is: careservices@glos.nhs.uk. Working with Communities – “Your Care, Your Opinion” A “Your Care, Your Opinion” Committee has been established within the Trust that ensures active two-way communication with local communities. The purpose of the committee is to raise awareness of the services provided by the Trust and that service development is informed by learning from user experience. In doing so it focuses on the elements of care that are critical to service users and that underpin the delivery of the commitments made within the NHS Constitution (March 2012). The work of the Committee is informed by the key national and local drivers for patient experience, with particular reference to the NHS Outcome Framework, the NHS Patient Experience Framework and the Trust Vision and Values. They focus on the elements of care delivery that service users tell us are important to them: 32 Care planned with the user that respects their values, preferences and expressed needs Professionals ensuring care is coordinated and integrated Clear information and communication Care with compassion that supports physical and emotional comfort Active involvement of family, carers and friends Support through transition and ensuring continuity Ease of access to care Listening, learning, improving User Experience Survey Programme The patient experience programme has over the past year (2012-13) seen an increase in the use of surveys to gain an understanding of the views of patients/service users regarding their care. More than 50 patient experience surveys were carried out across the organisation during the year including the in patients survey using “real time” electronic data collection. The overall responses to the core questions included in each survey show a high level of satisfaction reported by those receiving care. Our patient experience surveys have shown that the majority of our patients feel that they are being treated with respect and dignity and that they are involved with decisions about their care and treatment. Patients tell us that they are being communicated with well; understanding what staff are telling them, being able to ask questions and being listened to by staff. More than 90% of our patients tell us they feel that they are being treated in a safe environment. One of the re-occurring themes is that patients say they do not always know how to feedback about the service they have received, in terms of offering compliments or making a complaint. To address this a review is under way of the current Complaints, Concerns, Compliments and Comments (4Cs) information leaflet, with a view to simplifying the content and renaming the leaflet so it is clear to service users about how they can provide feedback. Patient stories 33 During 2012/13 Gloucestershire Care Services (GCS) began work on Patient Stories; a new method of involvement with our patients and their relatives or carers to strengthen our public and patient involvement. Patient Stories provides a unique method of gaining the views of “I’ve learnt coping service users as it does not rely on strategies, communication surveys or questionnaires which skills alongside many other may answer questions the useful techniques and to organisation feels important, but become a better selfallows the participant to tell their manager and I still use many story in their own words without of the skills that I learnt from direction or agenda from the interviewer. Story telling in this way is seen as a very powerful method of gaining views and feedback of the care and services received, the stories will provide us with valuable information regarding the care provided by GCS. We will be able to use this information to inform and support service development or improvement initiatives and importantly to celebrate good news and promote where the experience and/or outcome of the care received has been positive. The story can be in the form of a written transcript of the conversation or an audio or video recording and there are various methods by which the Patient Story can be shared all depending on the consent and wishes of the participant. We anticipate sharing the story with the teams of the services involved, at our Trust Board meetings, during staff induction and training and also on our internal and external websites. Although this project has started on a small scale, several patients and “I write to bring your carers have already kindly participated and shared their attention the outstanding experiences with us. GCS would like care given to my husband. to thank all those people who have Their visits were reassuring taken the time to work with us to and comforting. We built up improve our services. To date the a good rapport and majority of our Patient Stories have friendship with the nurses been provided by members of the Expert Patient Programme, five members of the group have given very positive feedback about the skills, strategies and strengths they gained during the programme and the overwhelming message has been about how this has enabled them to feel more fulfilled and independent with better management of their condition. 34 “The excellent service was provided efficiently and professionally. Staff were consistently on time and provided appropriate support, guidance and information at a time when it was most needed.” We have also received two stories from relatives of patients who have had inpatient stays at our Community Hospitals; the common theme running through these stories is around the importance of clear and reliable communication between not only the clinical staff and the patient and family but also between members of the multidisciplinary team. As an organisation we have been able to review some of our processes, we have put in place training and updates for staff and have also introduced a new role of Care Communication Co-ordinator at one of our Community Hospitals. These measures will be reviewed and assessed in due course. Care Quality Commission 2012-13 The Care Quality Commission (CQC) is the regulator for all care provided with hospitals, care homes and within people’s own homes. During 2012-13 the CQC undertook three inspections of services provided by the Trust. The full reports of these inspections are available via the CQC website www.cqc.org.uk. Visits from the Care Quality Commission (CQC) The North Cotswold Hospital The North Cotswolds Hospital was inspected by a team from the Care Quality Commission (CQC) on the 26 July 2012. During the inspection care was observed, staff were interviewed and records reviewed all supported by conversations with patients and families. The following essential standard of care where assessed and the hospital considered fully compliant. • • • • • Consent to care and treatment Cooperating with other providers Safeguarding people who use services from abuse Staffing Complaints The following essential standards were also assessed during that visit and some improvement noted as required. • Clinical records 35 • Care and welfare of people who use services The learning from this visit was shared across all our community hospitals and as a result, the following actions are being implemented: • Review of clinical record keeping by our internal auditors • Review of clinical records to develop a single record used by all professionals Locally the visit led to significant service changes taking place including extended documentation auditing, updating of staff on the resuscitation policy and adaption of the intentional rounding process. The Matron is monitoring the actions underway to ensure full compliance be evidenced when CQC next visit the site. The Dilke Hospital The Dilke Hospital was reviewed by the Care Quality Commission on the 30th August 2012 in response to a previous visit. The review was intended to provide assurance that action had been taken to ensure compliance against the following essential standards: • • • • • • Respecting and involving people who use services Care and welfare of people who use services Meeting nutritional needs Safeguarding people who use services from abuse Supporting workers Records The review found the Dilke Hospital to be meeting all essential standards. The initial visit led to a number of service changes including introduction of care coordinators from within the multi-disciplinary team, regular review meetings with patients and relatives, including a daily “ward round” for relatives and a review of communication processes. The Trust were delighted that these actions evidenced improvement when reviewed. Hope House Hope House, Sexual Health Services were inspected by the Care Quality Commission on the 20th March 2012 and were found to be compliant within the essential standard assessed. People's personal records, including medical records, should be accurate and kept safe and confidential. This review was undertaken as part of a national programme of inspection relating to assurance with practice associated with termination of pregnancy. The inspection found that the Trust met the part of the regulation which was the subject of this review in relation to the use of the HSA1 forms by doctors. Our compliance with Care Quality Commission standards Gloucestershire Care Services NHS Trust is required to register with the CQC and its current registration status is unconditional. The CQC has not taken enforcement action against Gloucestershire Care Services during 2012-13. 36 Complaints and our learning In 2012 - 13 the Trust received a total of 88 formal complaints. This compares to 76 formal complaints in the previous year. Figure 1: Complaints by Quarter 35 30 COMPLAINTS BY QUARTER 29 28 25 20 18 15 24 21 18 13 10 13 5 0 Q1 Q2 Q3 Q4 2011-12 Q1 Q2 Q3 Q4 2012-13 Given the relatively low numbers of formal complaints received, trend analysis is difficult, of note, however is: • • • Of the complaints received, approximately 30% related to community hospital inpatient and minor injury unit services and 25% related to Out of Hours Services. Just fewer than 40% of formal complaints received in 2012/13 related to ‘treatment issues’. Approximately 14% related to complaints about the doctors attitude and the treatment received or prescribed by the Out of Hours Service. Key to the Trust’s approach to the management of complaints is ensuring that lessons are learnt and appropriate actions are taken where improvement is needed. The Integrated Governance and Quality Committee have a role in overseeing this. Some examples of the learning from complaints and the investigations undertaken are summarised below. Example of Learning from Complaints Stroud General Hospital discharge planning and arrangements: • Formal contact meetings are now held with patients and families within the first 48 hours of admission to improve and aid communication and enable families to be a part of the care planning process Unitary multi-disciplinary team notes have been developed to include Occupational Therapy records Communication and information sharing with the Community Nursing teams following discharge: • Referral protocols have been reviewed to ensure that the community nursing teams 37 • • have adequate information regarding patients clinical needs prior to discharge from hospital The Community Nursing teams now make routine telephone contact with all patients known to have new/short term catheter in situ as soon as possible in order to advise them how and when to make contact if they need support or advice The Community Nursing teams have implemented changes to their practice in recording messages and actions taken Communication between the Health Visiting Teams and service users where referral to Gloucestershire County Council (GCC) is required: • • The Health Visiting teams now ensure that parents are given the referral guidelines and correct information for any services they refer into The Health Visiting Service has implemented action to ensure that telephone messages are dealt with in a timely manner Addressing delays in specialist assessment involving Children’s’ Occupational Therapy: • The service has used the feedback to instigate a complete review of the service to create a fully integrated team with a single point of access. To ensure improved communication with service users, the team have worked in partnership with Gloucestershire Carers Association and agreed a series of update letters to be sent to families, keeping them fully informed of their case progress. Timeliness of our response to Complaints We make contact with individuals making a complaint and agree the review process and the timeframe in which they can expect to receive a response. For the year 2012-13, 97.7% of response letters were sent to the complainants within the agreed timeframes. This represents a significant improvement on 2011/12. Q1 2012 Q2 2012 Q3 2012 Q4 2012/2013 2011/12 No % No. % No. % No % No % Response Time Within Agreed Timescale > by 1-3 days >4 days C/F 0 Total 28 No % 28 100% 18 100% 27 93.1% 13 100% 86 97.7% 54 75.0% 0 0% 0 0% 1 3.4% 0 0.0% 1 1.1% 4 5.6% 0 0% 0 0% 1 3.4% 0 0.0% 1 1.1% 14 19.4% (2) 100% 18 100% 29 100% 13 0.0% 100% 88 100% 72 100% 38 Incident Reporting 2012-13 It is the Trust policy that staff report all adverse incidents using our Datix database which is a computerised system for logging and analysing all incidents across the organisation. An adverse incident is any event which affects a patient, member of staff, visitor or contractor which could have, or actually has caused harm while he or she is under our care or on the Trust premises. A high reporting rate within an organisation is evidence of a positive reporting culture, especially when this is linked with a low level of serious harm incidents in the Trust. The level of serious harm sustained as a result of an incident is approximately 0.29% of the total number of incidents reported. Our incident reporting processes have enabled us to develop a comprehensive quarterly governance report which provides data on trends in relation to patient and staff safety incidents and provides reporting at team, locality and Board level. The Trust has a duty to report all patient related safety incidents and near misses to the national database – the National Reporting and Learning System. As incidents are investigated, the learning from such is shared widely and used to inform changes to policy or work practice across the organisation. Incident Types 2012/13 Clinical incident Communication Records, Information, Confidentiality Discharge, Transfer, Appointment Estates, staffing, infrastructure Fire incident Personal Accident Security incident Violence, Abuse or Harassment Vehicle incident Waste Environmental Incident TOTALS Q1 349 100 55 127 76 13 376 49 43 5 8 1,201 Q2 436 86 60 139 105 14 393 43 58 9 9 1,302 Q3 553 63 67 133 75 3 440 51 49 5 7 1,446 Q4 470 97 62 135 66 6 440 49 45 10 14 1,394 Total 1808 346 244 534 322 36 1649 192 195 29 38 5,343 The analysis of incident type mirrors the national picture that falls and pressure ulcers are the highest recorded concerns as reported by the National Reporting and Learning System (NRLS). The category ‘clinical incident’ includes ‘pressure ulcers’ and the category ‘personal accident’ includes patient falls. These figures also include pressure ulcers which are inherited from other care providers. This year has seen the development of a new process to monitor the management of pressure ulcers. The nature of this new process has meant that management of this category of incident is discussed and shared as well as monitored. The Trust is confident that this proactive approach will see the number of acquired pressure ulcers fall in the future, working with other agencies to look at a reduction across the care pathway. This approach also ensures that any safeguarding concerns associated with a patient developing a pressure ulcer are identified and acted on. 39 Serious Incident Requiring Investigation (SIRI) reported via STEIS The Trust has continued to develop its learning from Serious Incidents Requiring Investigation (SIRIs) reported via the Strategic Executive Information System (STEIS) database. Management of these incidents is monitored to ensure they are investigated in a timely manner to ensure learning is shared with the service as quickly as possible. All incidents classified as SIRIs must have to be reported to our Commissioners within 24 hours of being notified, require an interim report, which is submitted to the commissioner within three days and, depending on the grade of the incident, a final report and action plan submitted to the commissioner within either 45 or 60 working days. Monitoring of the action plan also occurs to ensure correction actions are undertaken and learning is embedded. During 2012‐2013, 14 of the 5343 reported incidents were classified as serious. These required more detailed investigation and were reported on the STEIS database. The majority of these incidents relate to pressure ulcers. As part of our quality drive to reduce the incidence of pressure ulcers, all acquired grade 3 and 4 pressure ulcers are treated as serious incidents requiring investigation. Valuing our staff The Trust appreciates that its success is built on its workforce and it recognises how important it is for staff to feel valued and to enjoy their work. We know that highly performing, highly productive staff that are happy and feel supported in their roles will ensure that we continue to provide the highest quality care to our patients. We are committed to supporting our staff to achieve their potential and to develop their skills, providing access to training and appropriate development opportunities. Our Staff We have a diverse, highly skilled and experienced workforce that helps us provide the highest quality care to our patients. As of March 2013, the Trust employed in excess of 2500 staff (excluding bank staff). Age profile The majority of staff (64%) are aged between the ages of 40-60 years with a further 8.5% aged over 60. This is reflective of the age profile of the NHS as a whole. Generally, the age profile of staff becomes older as the pay bands get higher. Gender profile By gender, 92% of staff are female reflecting the traditionally female bias in caring roles. The proportion of men in the organisation is greater in higher pay bands. Ethnicity profile 95% of the workforce is White British, 2% are White non-British, and 3% are from a BME background. The ethnic profile of the staff is not quite reflective of the county profile, where 90% of people are White British. 40 Disability profile 0.8% of staff are listed on the Electronic Staff Record (ESR) as having a disability. However, 12% of staff disclosed a disability in the 2011 staff survey compared to a national average of 16%. Religion/ Belief profile Just over half the staff have not disclosed their religion/belief in the ESR. Of those who have disclosed, the majority (38%) are Christian. There are small numbers of staff with other beliefs 4% are atheist, and 3.5% cite their religion/belief as ‘other’. Sexual orientation profile Half the staffs have not disclosed their sexual orientation on the ESR. Of those who have disclosed, 49% are heterosexual, 0.2% are gay, 0.2% lesbian and 0.25% bisexual. Marriage/ civil partnership profile 63% of staff are married, 0.14% are in a civil partnership and 24% are not married or in a civil partnership. The remainder have not disclosed their marital status. Supporting our staff The Trust has a comprehensive set of Human Resources policies which clearly set out equal opportunities for employment and promotion, based on abilities, qualification and abilities for the post. This includes a clear whistleblowing policy called “It’s Okay to Ask Why” reflecting the commitment of the organisation to seek feedback from staff on any concerns and issues they identify. From April 2013 the Trust has been accredited as meeting the Investors In People Standard (IIP). The principle strengths noted within the assessment were the: • • • • • • • • • • Clarity of vision and values. Sound and visible business planning. Engagement with members of the team and recognising and affirming their contributions. Good practice in appraisal and performance management provides a sound base for development. Senior leaders and many in local and specialist service senior roles are effective role models. Ideas and suggestions are being sought from around the organisation and evaluated. There is much encouragement for career development at all levels. Mandatory training. Support for sound practice and positive behaviours across the whole team provide a bedrock for delivering effective performance There is a commitment for analysis, evaluation and honest reflection The organisation is also registered as a ‘Mindful Employer’ and has been accredited as a two tick employer. The Two Tick accreditation means that all those applying for positions within the Trust with a disability, are guaranteed an interview, if they meet the minimum requirements of the role. In addition, the organisation is developing an action plan to support its intention to sign the “Time for Change” pledge. Stress-awareness training is available for all staff through our ‘Lighten Up’ programme. This is a holistic approach to rebalancing life and work, with practical tools for managing pressure. We 41 particularly encourage staff who have raised stress as an issue (or have been absent from work due to stress), to enrol on the programme. In addition to the nationally recognised Lighten Up programme, The Trust provides access to an employee assistance programme (EAP) and Occupational Health Service for all our staff. The EAP is provided by an external company and offers staff and their families a free 24 hours helpline and counselling service. The Occupational Health Department, “Working Well” provides a free confidential health advice service to staff. Advancing Diversity The Trust is in the process of implementing the NHS Equality Delivery System (EDS). Working on a series of peer reviews and internal assessments, the EDS provides a comprehensive method for meeting the requirements of the Equality Act (2010). This truly participative approach will provide the basis for stronger links with our communities. We now have a clear direction for how we can strengthen our performance to raise the quality of our services for all our service users and particularly more disadvantaged and vulnerable people in Gloucestershire. Based on this the Trust has developed its equality objectives, focused around four goals: • • • • To mainstream equality in business development processes To improve the quality of evidence on equality in the organisation To improve our dialogue with external stakeholders especially those with protected characteristics or in vulnerable groups To ensure we have a diverse workforce who actively promote equality in their work and beyond Engaging with Staff To increase staff engagement across the organisation nine staff forums have been set up across the organisations business units, which are open for all staff to attend. Staff from each of the forums are elected by their colleagues to sit on the organisation’s staff council. The staff council which is attended by a Non-Executive Director has strong links to the Trust Board and they meet together on a bi-annual basis. The terms of reference for both the staff forums and staff council have been determined by staff in order to encourage as much participation has possible. The terms of reference of the Staff Council include: • • • • • • Highlighting issues of particular concern to staff and make proposals on how to address these Consulting upon proposed organisational objectives Reviewing the performance of the organisation Commenting upon key organisational decisions Making proposals on how to improve the services of GCS Influencing and constructively challenging the Board The Trust has a Joint Negotiating and Consultative Forum (JNCF) that meets at least bi-monthly, where terms and conditions of employment and Human Resources policies are negotiated and discussed. The Chief Executive, Director for Adult Services along with the Head of human resources are members of this forum. The following trade unions are represented: Unison, Unite, Chartered Society of Physiotherapy (CSP), Royal College of Nursing (RCN), British Dental Association (BDA), Society of Chiropodists and Podiatrists (SCP), and the British Medical Association (BMA). 42 Staff Development Building the skills and competencies of our workforce is key to unlocking potential and efficiencies, improving quality and efficiency for the future. As an employer, we are committed to developing a flexible and productive workforce through effective skills utilisation of the existing workforce. In the coming year we plan to:• • • • • • • Further expand our apprenticeship and work experience schemes Review our succession planning/ career pathways Develop the capacity and capability of the volunteer workforce. Further develop management and leadership skills, competencies and behaviours Continue to invest in developing the clinical skills of our workforce to meet local need Further develop the roles of Integrated Support Workers Develop a more flexible and responsive Contingent Workforce Staff survey The Trust is an active participant of the National staff surveying programme but we did not actively survey our staff in 2012 because we were still part of the Primary Care Trust who were exempt from participating in the survey during that year. We have however undertaken an internal survey of staff at the beginning of 2013 and will be reporting the findings to the Board in July 2013. The survey did incorporate the “Friends and Family” test, so we look forward to hearing what our staff have to say about working for this organisation. 43 Quality and Performance Quality and Performance achieved within our Adult Services CRITERIA Out of hours Primary Care Centre emergency face to face consultation within 60 minutes Adult Community Services - % treated within 8 weeks Adult Speech And Language Podiatry Adult Physiotherapy Adult Occupational Therapy Special Nurses: Percentage treated within 8 weeks Parkinson’s nurses Diabetes nurses Bone Health Service Musculoskeletal Service Cancelled operations for non-clinical reasons not offered a binding date within 28 days Cancelled operations Minor Injury Units (MIUs) % seen waiting less than 4 hours % seen waiting less than 2 hours Bed Occupancy: All Community Hospital medical beds Occupancy Average wait of for access to service Adult Physiotherapy Combined Specialist and Non Specialist Wheelchair Service Podiatry TARGET 2012/13 95% 98% 95% 95% 95% 95% 99% 97% 97% 99% 95% 95% 95% 95% 100% 99% 98% 98% 0% 0% 98% 98% 99.9% 97.2% 90% 92.4% 2 weeks 2 weeks 2 weeks 3.6 0.8 2.0 The red status declared for Adult Physiotherapy and adherence to the locally agreed access target of 2 weeks, is predominantly due to waiting list pressures within a specific locality which was worsened by difficulties with recruiting. This has since been resolved with a successful recruitment into the locality. 44 Quality performance achieved within our children’s’ services CRITERIA Community Services - % treated within 8 weeks Paediatric speech and language Paediatric physiotherapy Paediatric occupational therapy Breastfeeding Prevalence at 6 – 8 weeks Neo-Natal Hearing Screen Screens offered Completed by 5 weeks Average wait for access to service Occupational Therapy Physiotherapy Speech and Language Therapy TARGET 2011-2012 YTD 95% 95% 95% TARGET 52% TARGET 99% >95% TARGET 2 weeks 2 weeks 2 weeks 97% 99% 99% ACTUAL 52% ACTUAL 100% 98.6% ACTUAL 1.5 weeks 1.1 weeks 1.9 weeks 2012-2013 YTD 99% 100% 98% 50% 100% 98.9% 1.7 weeks 1.6weeks 1.9 weeks The prevalence of breast feeding at 6-8 weeks fell significantly during 2012-13 to 50% from the previous year’s 52%. The inherited 2 week prevalence rate was 74.1% at 2011/12 outturn but had reduced to 60% by 2012/13 outturn (a fall of 14.1%). Collaborative work with Gloucestershire Hospitals, Children’s Centres and Public Health Commissioners is addressing this public health problem. Targets for 2013-14 will include a minimum drop off rate between 2 weeks and 8 weeks for the Trust, specific targets for poor performing children centre areas, and countywide joint-provider prevalence targets. 45 Same sex accommodation: declaration of compliance 2013-14 The Trust is pleased to confirm that we are compliant with the government’s requirement to eliminate mixed-sex accommodation, except when it is in the patient’s overall best interest, or reflects their personal choice. Every patient has the right to receive high quality care that is safe, effective and respects their privacy and dignity. Gloucestershire Care Services NHS Trust is committed to providing every patient with same sex accommodation, because it helps to safeguard their privacy and dignity when they are often at their most vulnerable. We have the necessary facilities, resources and culture, to ensure that patients who are admitted to our hospitals will only share the room where they sleep with members of the same sex and same sex toilets and bathrooms will be close to their bed area. Sharing with members of the opposite sex will only happen when clinically necessary (for example where patients need specialist equipment), or when patients actively choose to share. This achievement is regularly monitored and if our care should fall short of the required standard, we will report it. We will also set up an audit mechanism to make sure that we do not misclassify any of our reports. The review of compliance forms part of our annual audit programme and for the reporting period 2012-13 there were no breaches of compliance. Our Information Governance (IG) toolkit attainment level Information Governance is the way by which the NHS handles all organisational information, but particularly personal and sensitive information about patients and employees. It allows organisations and individuals to ensure that personal information is dealt with legally, ethically, confidentially, securely, efficiently and effectively, in order to deliver the best possible care. In the information Governance Toolkit there are three levels of assessment across 41 requirements, these cover the way in which organisations ‘process’ or handle information. The attainment levels are cumulative starting with Level 1 and rising to Level 3. In 2012-13, NHS Gloucestershire (including Care Services), achieved 69% compliance against the requirement of the annual Information Governance Toolkit (version 10) assessment with 40 out of the 41 requirements achieving Level 2 statement of compliance for Connecting for Health. This compares to 67% compliance against the annual Information Governance Toolkit (version 9) in the previous year. 69% is the upper point of Level 2 which shows very good processes in place across the organisation. The Trust has developed an Information Governance improvement plan for 2013-14 for submission to Connecting for Health. This lays out plans to deliver to Level 2 on all 41 requirements during 2013-14. This will be supported by a data mapping programme and the collation of a detailed information asset register. 46 The Information Governance Management and Technology Steering Group oversee the progress of this work and provide assurance through to the Integrated Governance Committee. Participation in clinical audits During 2012-13 no national clinical audits and no national confidential enquiries covered NHS services that Gloucestershire Care Services NHS Trust provided. However a number of services contributed information to national audit programmes where the participation was then by Gloucestershire Hospitals NHS Trust. These are as follows: • • • Parkinson’s Disease – Specialist Nursing Parkinson’s Disease – Speech and Language Services (SALT) National Hip Fracture database National Clinical Audit No. Of cases submitted Parkinson’s Disease audit: participation by specialist nursing service 30 Parkinson’s Disease audit: participation by speech and language therapy service 10 National hip fracture database: patient outcomes at 120, 365 days post-surgery 1065 % Of Total Report Number reviewed submitted Publication of 100% report awaited Publication of 100% report awaited 100% Actions taken as a result of the audit On-going participation to Yes by be confirmed by Gloucestershire Commissioners. Hospitals Consideration being Foundation given to participation in Trust more relevant National Fracture Liaison database Data Quality Good quality information underpins the safe and effective delivery of patient care and is essential to support improvements in care quality. TPP SystmOne has recently been selected under a national procurement process as the new community system. This will allow clinicians to collect clinical data and enter data directly into the system. This will improve both the data collection and quality. Deployment is planned to commence in June 2013. NHS Number and General Medical Practice Code Validity The Trust submitted records throughout the reporting period to the secondary uses services (SUS) for inclusion in the hospital episode statistics which are part of the latest published data. The 47 percentage of records in the published data, which included a valid NHS number, are detailed below and measured against the national average. Admitted patient care Outpatient care Accident and Emergency care GCS 99.7% 99.9% 98.0% National Average 99.1% 99.3% 95.1% Status The percentage of records in the published data which included the patients’ valid general medical practice code is measured against the national average as detailed in the following table. Admitted patient care Outpatient care Accident and Emergency care GCS 100% 100% 100% National Average 99.9% 99.9% 99.7% Status Clinical Coding Error Rate The Trust will not be reporting on the clinical coding error rate as GHNHSFT undertakes this activity on our behalf. GHNHSFT monitor and report the clinical coding error rate as part of the national audit requirements. Our Participation in Clinical Research The number of patients receiving NHS services provided or sub-contracted by the Trust in 2012-13, that were recruited during that period to participate in research approved by a research ethics committee was 47. Financial Statement During 2012-13 Gloucestershire Care Services Trust provided and/or sub-contracted 54 NHS services. Gloucestershire Care Services NHS Trust has reviewed all the data available to them on the quality of care in all of these NHS services. The income generated by the NHS services reviewed in 2012-13, represents 100% of the total income generated from the provision of NHS services by 2012-13. 48 How To Contact Us We really value your feedback so if you have any questions or comments about the content of this report please write to: Mrs E J Fenton Director of Nursing Gloucestershire Care Services NHS Trust Edward Jenner Court 1010 Pioneer Avenue Gloucestershire Business Park Brockworth Gloucester GL3 4AW Email liz.fenton@glos.nhs.uk If you have any comments, concerns, complaints or compliments about the services we provide, please do not hesitate to contact the: Patient Advice & Liaison Services (PALS) on: 0800 151 1508. 49 Amendments and additions to the document following feedback from our Partners Gloucestershire Care Services NHS Trust values the feedback we have received from our partners on the Quality Account (Draft for Consultation). This document has now been finalised with the following amendments and additions as a result of the feedback received. • • • Quotes from patients and carers included Tables reviewed and data presented in a format to aid understanding Section added regarding the value of volunteers 50 APPENDIX A Gloucestershire Clinical Commissioning Group Comments on the Gloucestershire Care Services Quality Account 2012/13 Gloucestershire Clinical Commissioning Group (CCG), on behalf of its predecessor NHS Gloucestershire, has taken the opportunity to review the Quality Account prepared by Gloucestershire Care Services (GCS) for 2012/13. We are pleased that GCS has been working closely alongside NHS Gloucestershire and the shadow CCG during 2012/13 to maintain and further improve the quality of commissioned services. GCS has co-operated in building new clinical and managerial relationships in preparation for the CCG to take over commissioning responsibility from 1st April 2013. GCS has been receptive to challenges and concerns, engaged with the development of initiatives such as the Joint Formulary, Map of Medicine and Your Health, Your Care strategy – our shared vision for the future. They have demonstrated commitment to further improvement of the safety, effectiveness and patient experience of services across a wide range of services, particularly in falls reduction in Community hospitals. The CCG welcomes GCS’s strong focus on patient experience and quality of care, which demonstrates a joint commitment to delivering high quality compassionate care. We look forward to developing a whole health and social care community clinical programme approach towards commissioning and delivering services, with a strong emphasis on clinical leadership and engagement. Integrated care will be delivered according to agreed pathways and standards, with strong user and carer involvement being evident from prevention to end of life. There are robust arrangements in place with GCS to agree, monitor and review the quality of services. The Quality Review Group continues to meet monthly and brings together managers and clinicians from both GCS and Gloucestershire CCG. We have received assurance throughout the year from GCS in relation to key quality issues, both where quality and safety has improved and where it occasionally fell below expectations with remedial plans put in place and learning shared wherever possible. The priorities for 2013/14 have been developed in partnership and Gloucestershire CCG endorses and supports proposals set out in the Quality Account to increase staffing levels in Community Hospitals and will fund recruitment into vacant nursing posts. Gloucestershire CCG would like to see a more ambitious programme to improving the quality of the services provided by GCS for 2014-15, which is reflected in the Quality Account. GCS are in a strong position to manage both present and future challenges, and to work with Gloucestershire CCG to deliver best value effective care for the people of Gloucestershire. 51 Gloucestershire CCG can confirm that we consider that the Quality Account contains accurate information in relation to the quality of services that Gloucestershire Hospitals NHS Foundation Trust provides to the residents of Gloucestershire and beyond. Dr Charles Buckley Clinical Commissioning Lead for Quality Marion Andrews-Evans Executive Nurse and Quality Lead 52 APPENDIX B Health and Care Overview and Scrutiny Committee Comments on the Gloucestershire Care Services NHS Trust Quality Account 2012/13 The county council has restructured its overview and scrutiny committee structure to better fit with the commissioning structure in place within the council. Therefore the Health, Community and Care OSC was decommissioned in April 2013, and from the start of the new council in May 2013 the Health and Care Overview and Scrutiny Committee (HCOSC) became effective. It is important to note that this new committee, with predominantly new membership, has not yet had much opportunity to engage with the GCS NHS Trust. However as Chairman of the HCOSC I am happy to offer some comments on this Quality Account. I am aware that it is difficult within the prescriptions of this type of report to achieve a balance between sufficient information such that the report is readable and informative (too little information and it is meaningless; too much and it is unwieldy and ultimately uninformative). The structure of this QA is much improved on last years and offers a good insight into the work of the Trust. However, despite the improvement, it is still difficult to get an impression of how the Trust’s overall performance can be measured against outcomes, i.e. what difference has this made to the patient/service users? Given the importance of the reablement and telecare/health agendas, I would have expected their contributions/impact to be explicit within the QA, and it was disappointing to see that this was not the case. It is good to note that staff input is valued and I welcome the Top 100 ideas scheme and look forward to hearing how these ideas are being progressed. It is also good to note that the number of (community hospital) patients engaging with the patient survey has increased; and that the Trust is taking forward the learning opportunities identified though the complaints process. Learning from customers is a valuable tool in understanding how the patient experience can be improved; but it will be important to understand whether this learning is improving patient outcomes. I welcome the integrated approach that the Trust is taking to safeguarding issues. The Great Western Ambulance Service (GWAS) was acquired by the South Western Ambulance Service NHS Foundation Trust (SWAST) in February 2013 and I would have expected to see this reflected in the commentary of the report. I am aware that the Single Point of Clinical Access (SPCA) is an effective resource to ensure that the patient receives the right care in the right place, and aims to reduce admissions to the Acute Hospitals. However, the QA only refers to GWAS in this regard and, whilst it is good to see that the number of referrals from the ambulance service has increased, it would have been helpful to see the number of referrals from across the wider health professional community, e.g. GPs. 53 To give the Incident Reporting section more context it would be helpful to know the number (percentage) of incidents against the overall patient and staff throughput across the Trust through the year. I look forward to working with the Trust and would like to take this opportunity to thank the Trust for engaging with the Health, Community and Care OSC in the last council. Cllr Steve Lydon Chairman Health and Care Overview and Scrutiny Committee 54 APPENDIX C Gloucestershire Local Involvement Network’s (LINk) Response on NHS Gloucestershire Care Service’s DRAFT Interim Quality Account 2013 Gloucestershire LINk welcomes the opportunity to comment on the draft NHS Gloucestershire Care Service’s 2013 Quality Account. The following comments have been compiled by a number of LINk members. Although we are able to comment on a number of areas within this draft report, we are limited in other areas as Quarter 4 data was not available. It is likely that a number of these comments are not relevant in relation to the final version of the Quality Account, but the cessation of LINk on 31st March 2013 made further comments impossible. We do not feel that this draft report gives sufficient information for the average lay reader to appreciate the full extent of the quality of the services provided by Gloucestershire Care Services. It would benefit from more details about the services, such as the community hospitals, and some quotes from patients and carers about the care they have received during 2012/13. The layout of the report has a number of tables to illustrate the data information, however, the lack of any graphs makes it difficult to visually see the relevant trends and prevalence rates that appear over time/will further enhance the understanding of the data information. In this draft there is an absence of qualitative information and including such information would significantly increase the quantitative and qualitative mix that reflects patient experiences and stories (good and bad) of your services. There is no reference to use of volunteers although we are aware that volunteers are welcomed by the trust and used in a number of venues. We were concerned to notice a rising number of clinical incidents Q1-Q3. It is possible this is due to a different method of recording but if so this should be clearly stated in the text. Throughout the report there is a clear need to expand on areas so as to give a full and comprehensive picture. We think that the report would benefit from expanding the narrative statements, in particular to cite how identified actions would be taken forward. We know that GCS works with a wide range of partners including the voluntary and community sector to deliver services to the public at large but there is no indication of this in the draft report. We would like to see a little more detail on how the GCS Quality objectives will be delivered in 2013/14 in the final report, including the engagement and involvement of people and communities. 55 There is no mention of the use of the National Institute for Health and Care Guidance (NICE) or implementing NICE guidance within the report and we would feel there should be to measure quality of GCS (i.e. against NICE Quality Standards). Barbara Marshall Chair of Gloucestershire LINk 28th March 2013 56 GLOSSARY BME C.difficile CQC CQUIN EAP ESR GCCG GCSNHST GHNHSFT GWAS HCOSC JNCF LCP LINk MAS MIU MRSA MUST NICE NHS OT PALS Black and Minority Ethnic Communities Clostridium difficile Care Quality Commission - The CQC regulates care provided in Hospitals, Care Homes and people’s own homes. This is the National Commissioning for the Quality and Innovation Payment framework which links part of the organisation’s income to quality improvement Employee Assistance Programme Electronic Staff Record Gloucestershire Clinical Commissioning Group Gloucestershire Care Services NHS Trust Gloucestershire Hospitals NHS Foundation Trust Great Western Ambulance Service Health and Care Overview and Scrutiny Committee Joint Negotiating and Consultative Forum Liverpool Care Pathway for end of life care Local Involvement Network Memory Assessment Service Minor Injuries Unit Meticillin resistant Staphylococcus aureus Malnutrition Universal Screening Tool National Institute for Health and Care Guidance National Health Service Occupational Therapy Patient Advice and Liaison Service helps the NHS to improve services by listening to what matters to our patients, their families and carers, answering questions and helping to resolve concerns as quickly as possible PEAT PLACE QA SHA SIRI SLT SPCA ST STEIS VTE Q1 Q2 Patient Environment Action Team Patient Led Assessments of the Care Environment Quality Account Strategic Health Authority Serious Incident Requiring Investigation Speech and Language and Therapy Single Point of Clinical Access NHS National Safety Thermometer Strategic Executive Information System which monitors serious incidents Venous-Thromboembolism (Deep vein thrombosis or pulmonary embolism) Quarter 1 – 1st April - 30th June Quarter 2 – 1st July – 30th September Q3 Q4 Quarter 3 – 1st October – 31st December Quarter 4 – 1st January – 31st March 57