Balance
advertisement

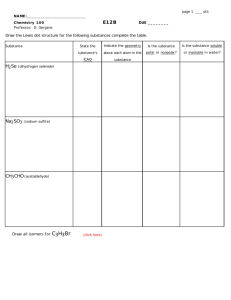
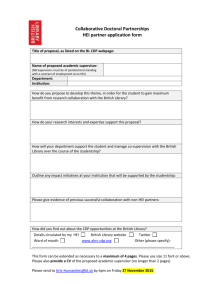
Authors: Mehrsheed Sinaki, MD, MS Susan G. Lynn, MA Balance Affiliations: From the Department of Physical Medicine and Rehabilitation (MS) and the Division of Audiology (SGL), Mayo Clinic, Rochester, Minnesota. Research Article Disclosures: Presented, in part, at the Annual Meeting of the American Society for Bone and Mineral Research, St. Louis, MO, October 3, 1999. Correspondence: All correspondence and requests for reprints should be addressed to Mehrsheed Sinaki, MD, MS, Mayo Clinic, 200 First Street SW, Rochester, MN 55905. 0894-9115/02/8104-0241/0 American Journal of Physical Medicine & Rehabilitation Copyright © 2002 by Lippincott Williams & Wilkins Reducing the Risk of Falls Through Proprioceptive Dynamic Posture Training in Osteoporotic Women with Kyphotic Posturing A Randomized Pilot Study ABSTRACT Sinaki M, Lynn SG: Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: A randomized pilot study. Am J Phys Med Rehabil 2002;81:241–246. Objective: To assess the effect of a proprioceptive dynamic posture training program on balance in osteoporotic women with kyphotic posture. Design: Subjects were randomly assigned to either a proprioceptive dynamic posture training program or exercise only group. Anthropometric measurements, muscle strength, level of physical activity, computerized dynamic posturography, and spine radiography were performed at baseline and 1 mo. Results: At the 1-mo follow-up, three groups were formed on the basis of the baseline computerized dynamic posturography results. In general, groups 1 and 2 had no significant change at 1 mo, whereas group 3 improved balance significantly at 1 mo. Conclusion: The subjects who had abnormal balance and used the proprioceptive dynamic posture training program had the most significant improvement in balance. Improved balance could reduce the risk of falls. Key Words: Balance, Exercise, Falls, Osteoporosis April 2002 Reducing the Risk of Falls in Osteoporosis 241 A lthough pharmacotherapy is essential in the treatment of osteoporosis, its efficacy in prevention of osteoporotic falls and fractures should not be overrated. The skeletal and psychological benefits provided by musculoskeletal rehabilitation are also important. Physical medicine and rehabilitation programs are justifiably fundamental to the management of osteopenia and osteoporosis. Ongoing research is attempting to develop treatment for osteoporosis, and investigators are also focusing on preventive measures, including hormone replacement therapy, exercise, and dietary interventions. An area that has received less attention in the field of osteoporosis research is the prevention of falls. Several studies have shown the life-threatening complications associated with falls.1,2 Approximately 30% of all women and 20% of all men older than 50 yr will fall each year.3 Although multiple factors often contribute to a fall,1 impaired balance is an important element.2,4 Even in relatively healthy, independent-living seniors, there is a high correlation between poor balance control and the incidence of falls.3,5 Nguyen et al.6 reported that body sway was an independent predictor of fracture prevalence in 1479 subjects and concluded that determination of balance was important to the prediction of falls and fracture. Recent studies have focused on balance changes that are likely to occur in the elderly.7,8 Given that impaired balance is associated with an increased propensity to fall,4,9 improvements in balance may reduce that risk. The flexed posturing that often develops in elderly persons may place their center of gravity closer to their limit of stability.5 This feature is also expected in subjects with kyphosis caused by osteoporosis. In a previous study,10 the authors found that patients with osteoporosis who had kyphosis had greater reliance on hip strategies 242 Sinaki and Lynn during computerized dynamic posturography (CDP) than those who did not have kyphosis. They also had more postural sway. Randomized order of trials with and without proprioceptive dynamic posture (PDP) showed no significant changes in postural sway or in balance strategies when subjects used PDP. This study was designed to determine whether such changes could be measured after long-term use of the PDP. The objective of this study was to determine whether an uncomplicated program using proprioception along with exercises such as a PDP training program could improve balance11 in osteoporotic women with kyphotic posture. METHODS Subjects After we obtained Institutional Review Board approval, seven women between the ages of 70 and 83 yr with osteoporosis who had been evaluated in our osteoporosis clinic were asked to participate in the study. Subjects who met the inclusion criteria were enrolled in the study. The study included only local women who were older than 65 yr and had a diagnosis of osteoporosis confirmed through radiographic changes of the spine (such as ballooning of disks, anterior wedging, nontraumatic compression fractures of vertebral bodies, loss of horizontal trabeculae, and end-plate opaqueness) and measurement of the bone mineral density of the spine with dual photon absorptiometry.12 Subjects were included if their thoracic kyphosis, measured on standing lateral radiography of the spine, showed a Cobb angle of 50 – 65 degrees.13 Subjects had to sign an informed consent statement and be willing to return for follow-up. Subjects were not included in the study if they had a history of any progressive neurogenic or myopathic disorder that was known to impair motor function or if they were receiving drugs known or presumed to affect the central nervous system or equilibrium, such as sedatives or anxiolytics. Other drugs that prohibited a subject’s participation in this study included diazepam (Valium), lorazepam (Ativan), alprazolam (Xanax), flurazepam (Dalmane), triazolam (Halcion), phenobarbital, secobarbital (Seconal), butabarbital (Butisol), chlorpromazine (Thorazine), promazine (Sparine), thioridazine (Mellaril), trifluoperazine (Stelazine), and prochlorperazine (Compazine). Subjects were also excluded if they used drugs known to affect muscle strength (e.g., corticosteroids) or if they abused alcohol. At baseline, all subjects had assessment of their level of pain (scale of 0 –10, with 0 being no pain), physical activity level, CDP, and muscle strength. Subjects kept a daily diary of their pain level during the 4-wk study and were monitored at 2 wk to assess their level of physical activity to make sure they were following the exercise program but not adding any additional strenuous activities. At the end of 4 wk, each subject’s pain level, physical activity level, CDP, and muscle strength measurements were again evaluated. The subjects were randomly assigned to one of two groups. One group received back extensor strengthening exercises only. The other group received the same exercise program plus PDP training with the use of a 2-pound weighted kyphoorthosis to be worn daily for 2 hr only during ambulatory activities (Posture Training Support) (Fig. 1).14 Participation in this study was strictly voluntary, and no remuneration was offered or provided to participants. After preliminary assessment of the data, the group that had PDP training was subdivided into two groups on the basis of their baseline scores of CDP:15 those who had a normal composite score on baseline CDP and those who had an abnormal compos- Am. J. Phys. Med. Rehabil. ● Vol. 81, No. 4 Figure 1: Posture Training Support (PTS). All subjects assigned to use the PTS were asked to follow the exercise program that is integral to use of the PTS. The PTS is a weighted kypho-orthosis that is applied to the back at the level of the scapulae. It encourages the use of back extensor muscles and helps to shift the center of gravity to aid in repositioning the spine to maintain upright posture as normal as possible. (Modified from Posture Training Support,14 with the permission of Mayo Foundation.) ite score on baseline CDP. Therefore, the three study groups were group 1 (exercise therapy only and abnormal baseline CDP), group 2 (exercise plus PDP training, normal baseline CDP), and group 3 (exercise plus PDP training, abnormal baseline CDP). Assessments CDP. CDP assesses both sensory organization and motor control components of balance. CDP is a safe, noninvasive procedure that takes approximately 20 min to perform.15 In our study, the sensory organization part of CDP was used to assess balance. The motor control section of CDP was not used because it was not found to be useful in a previous study.10 In this study, the clinician performing CDP was blind to the study group assignment of the subjects. All subjects underwent the CDP test twice in succession; the first CDP test was performed without use of the Posture Training Support, and the second test was done with the PosApril 2002 ture Training Support. A subject’s positioning on the forceplate remained consistent throughout all testing as judged by the placement of the feet in relation to a grid affixed to the footplate. Indices of postural stability assessed were the composite score and the average scores of all trials of subtests 5 and 6. Repeat testing was done 1 mo later and followed the same protocol. The sensory organization portion of the CDP test attempts to isolate each of the three sensory systems involved in maintaining balance to determine a patient’s ability to use the systems effectively. The patient stands with a safety harness in place on a platform facing a colored visual surround and is asked to maintain balance. Each trial is 20 sec long, and up to three trials can be performed for each subtest. The feet are placed in a position that provides a broad base of support. Pressure transducers under the footplate, with calculations for height and weight of the subject, allow measurement of the degree of postural sway relative to the 12.5 degree cone of stability. A score of 0 represents instability to the point of falling or having to step. A score of 100 represents no sway. A single transducer measures shear force or horizontal displacement on the platform. Horizontal forces on the platform increase relative to vertical force when the subject flexes at the hips rather than at the ankles to maintain balance (Fig. 2). Sensory subtests 5 and 6, the most difficult of the subtests, involve elimination of inaccuracy of visual and somatosensory cues. Reliability of the sensory organization tests has been assessed through evaluation of the same 45 subjects on different days; this showed a less than 10% improvement on sensory conditions 5 and 6.15 Standardized Radiographic Evaluation. Each subject had lateral thoracic and lumbar radiographs obtained at baseline to determine Figure 2: Six subtests of the sensory organization test of computerized dynamic posturography. Subtests become progressively more difficult as sensory information is altered. (From Lynn et al.10, with the permission of the American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation.) Cobb angle and kyphosis and at 1 mo to determine any significant radiographic changes (i.e., fracture or subluxation).16 Strength Measurements. Back extensor strength was measured at baseline and 1 mo (without knowledge of the subject’s other laboratory results) with a strain-gauge isometric dynamometer (BID-2000, Mayo Clinic, Rochester, MN), according to a standardized technique. This device provides a safe, reliable (coefficient of variation, 2.33%), and valid (P ⫽ 0.001) method of evaluation.17 Dominant and nondominant maximal grip strength was measured to evaluate changes in general muscle strength. A JAMAR dynamometer (Jamar, Jackson, MI) was used to determine maximal grip strength at baseline and 1 mo. This device has been used in several other studies to measure grip strength.18,19 Knee extensor strength assessment consisted of measuring 10 maximal repetitions (i.e., the maximal weight that can be moved through a full range of motion for 10 repetitions) with sandbag weights ranging from 1 to 25 pounds. Subjects were seated on a table with their body positioned in 90 degrees of hip flexion Reducing the Risk of Falls in Osteoporosis 243 TABLE 1 Baseline and 1-mo characteristics Group Subject Age, yr Balance (CDP), normal ⱖ68 Height, cm Weight, kg 0 0 1 mo 0 1 mo 153 145 38 37.8 38 37.3 60 49 155 153.8 59 64.5 61 64.5 145.9 153.5 154 54 61.0 63.6 54.2 61.0 63.6 Exercise only, abnormal baseline CDP 1 70 153 2 82 147 Exercise, PDP, normal baseline CDP 3 71 153.5 4 70 152.8 Exercise, PDP, abnormal baseline CDP 5 81 145.8 6 74 153.5 7 83 154 1 mo PAS, 0-18 Pain, 0-10 Change 0 1 mo 0 1 mo 58 52 ⫺2.0 ⫹3 6 3 7 6 10 5 7 4 77 88 82 86 ⫹5 ⫺2 2 6 6 8 10 10 4 2 33 58 56 70 71 74 ⫹37 ⫹13 ⫹18 2 4 4 7 6 8 9 6 8 4 2 5 CDP, computerized dynamic posturography; PAS, physical activity scale; PDP, proprioceptive dynamic posture training (includes use of a Posture Training Support); 0, baseline. and 90 degrees of knee flexion with the palmar aspect of the hand resting on the subject’s thigh. Weighted sandbags were placed on the dorsum of the talocalcaneal joint; the weight selected allowed a maximum of 10 repetitions with periods of 5 sec holding and 5 sec resting. Subjects were instructed to extend the leg, without a jerking motion or extending of the spine, within an arc of motion until the heel was parallel to the floor. A 5-sec rest period was allowed between contractions until all 10 repetitions were completed. The maximal weight lifted was documented in pounds and converted to newtons, and the process was repeated on the contralateral leg. Physical Activity Level. Lifetime history of physical activity was assessed by a face-to-face interview, without knowledge of the subject’s muscle strength or bone mineral density, and by a questionnaire based on our previously published standardized scale (Physical Activity Score) that reflects the total level of daily physical activities, including homemaking (0 – 6), job (0 – 6), and sports (0 – 6).20 This questionnaire was designed to assess the level of daily physical activity by converting the amount of weight lifting and walking involved in house- 244 Sinaki and Lynn work, job, and sports into METs (1 MET is the metabolic oxygen requirement under basal conditions, which is equal to the basal metabolic rate).20,21 For instance, the category of homemaking considers shopping and cooking as activities after a daily job away from home, whereas if a person’s job is homemaking, the scale considers that more housework, laundry, and perhaps child care are done during the day. Tables from the American Heart Association were used to assign METs to a subject’s daily activities.21 For example, activities that require 1.5–2 METs are considered to be very light and were scored as 0, whereas activities that require 8 –10 METs or more were considered very heavy and were scored as 6. The reproducibility of this scale was evaluated by six physicians who independently scored the same 10 volunteer women on each of three activities.20 For those 10 subjects, the median interexaminer coefficient of variation was 19%, which is acceptable for clinical follow-up.20 All evaluations for this study were performed by the same examiner. The reproducibility of technique for the same examiner has demonstrated a coefficient of variation of 2.3%.17 Level of Pain. Each subject’s level of back pain was measured with a pain scale of 0 –10. During a face-to-face interview at baseline, each subject was asked to state her perceived level of back pain on a scale of 0 –10 (0, no pain; 10, high pain). Each subject kept a daily diary of her perceived level of back pain during the 4-wk study period. Level of back pain was again assessed at the end of the study by face-to-face interview. RESULTS Characteristics of the subjects at baseline and 1 mo are depicted in Tables 1 and 2. For the age group of the subjects included in this study, normal scores are above 68 on CDP. The results of the CDP evaluation are summarized in Figure 3. Small gains in the CDP composite score were evidenced in group 1 (exercise only) at the 1-mo test. The two patients in group 1 had abnormal composite scores on the baseline CDP test. The change in the composite score from baseline to 1-mo follow-up was insignificant. One patient had worsening in the CDP score from baseline level. The two patients in group 2 (PDP ⫹ exercise) had normal composite scores on the baseline CDP test. Am. J. Phys. Med. Rehabil. ● Vol. 81, No. 4 TABLE 2 Baseline and 1-mo strength measurementsa BES, newtons Group Subject Age, yr 0 4 wk Hip extension (R/L), newtons 0 4 wk Exercise only, abnormal baseline CDP 1 70 111.2 97.9 13.3/8.9 13.3/8.9 2 82 62.72 57.8 0/0 0/0 Exercise, PDP, normal baseline CDP 3 71 62.72 62.72 0/0 0/0 4 70 186.8 235.7 31.1/31.1 44.5/44.5 Exercise, PDP, abnormal baseline CDP 5 81 93.4 155.7 0/0 0/0 6 74 97.9 97.9 0/0 0/0 7 83 129 177.9 0/0 17.8/22.2 Hip flexion (R/L), newtons Grip (Dominant/Nondominant), KES (R/L), newtons newtons 0 4 wk 0 4 wk 0 4 wk 22.5/22.5 44.5/44.5 22.5/22.5 66.7/66.7 44.5/44.5 44.5/44.5 80.8/66.7 44.5/44.5 227/178 222.4/178 244.6/204.6 231.3/182.4 22.2/31.1 66.7/66.7 48.9/44.5 89/89 22.2/31.1 40/35.6 53.4/53.4 80.1/80.1 120.1/89 182.4/200.2 133.4/93.4 182.4/204.6 44.5/44.5 111.2/111.2 35.6/35.6 44.5/44.5 111.2/111.2 66.7/66.7 44.5/31.1 44.5/31.1 66.7/66.7 66.7/66.7 44.5/53.4 53.4/57.8 146.8/155.7 222.4/177.9 191.3/177.9 133.4/160.1 244.6/133.4 177.9/155.7 BES, back extensor strength; CDP, computerized dynamic posturography; KES, knee extensor strength; PDP, proprioceptive dynamic posture training (includes use of a Posture Training Support); R/L, right/left; 0, baseline; 1 newton ⫽ 0.2248 lb. a 0 strength indicates subject was able to lift only the extremity tested with no additional weight. These patients did not have improvement at the 1-mo follow-up test. The change in the composite score from baseline was 1.5. The three patients in group 3 (PDP ⫹ exercise) had abnormal composite scores on the baseline CDP test. However, significant improvements were achieved at the 1-mo follow-up test when the CDP composite sensory score became normal in all cases. The average change in the composite score from baseline Figure 3: Changes in balance, tested with computerized dynamic posturography, from baseline to 1 mo in seven subjects (A–G). Group 1, exercise therapy only; group 2, exercise plus proprioceptive dynamic posture training, normal baseline computerized dynamic posturography; group 3, exercise plus proprioceptive dynamic posture training, abnormal baseline computerized dynamic posturography. April 2002 to 1 mo was 22.7. Comparison of the three groups showed a significant change in the CDP composite score in group 3 only. Comparing this change between groups, there was a significant difference between groups 3 and 1 (22.7 vs. 0.5) and groups 3 and 2 (22.7 vs. 1.5). No changes were found in balance strategy score in any of the groups. The physical activity score was measured at baseline and 1 mo to monitor the subjects’ day-to-day activities during the study period. With the study exercise program taken into account, all subjects increased their level of physical activity by 1 point from baseline. In addition, subjects in groups 2 and 3 increased their level of physical activity by an additional 1 point through the use of the PDP program. Of interest, five of the seven subjects had increased their day-today level of physical activity. Also of interest, all subjects had decreased back pain on follow-up. Body weight stayed about the same in all subjects. Tables 1 and 2 provide all the variables that were checked at baseline and 1-mo follow-up evaluations. DISCUSSION This study was designed to evaluate the effect of a user-friendly method to improve balance in subjects with osteoporosis and kyphotic posture. Several studies have evaluated strategies for prevention and treatment of osteoporosis through increasing peak bone mass and muscle strength. Increasing age, changes in proprioception, and reduction of muscle strength contribute to the risk of falls. The risk of falls decreases after participation in lower extremity strengthening exercises in older individuals.22 One study showed significant improvement in quadriceps strength but did not show any improvement in balance.23 In this study, a proprioceptive technique applying a weighted kypho-orthosis was used to determine whether balance could be improved without a specific effort to increase muscle strength. Muscle strength increases after 6 wk of participation in a strengthening exercise program.24 The duration of the current study was intentionally 1 mo—not long enough to increase muscle strength substantially but long enough to improve muscle recruitment, if any. We planned our study on the basis of Reducing the Risk of Falls in Osteoporosis 245 balance and kyphotic posture. After baseline CDP was performed, however, we noted that even the subjects with kyphosis could have good balance without strong back muscles in comparison with the rest of the subjects. We concluded that proprioception had to play a role because the weighted kypho-orthosis (Posture Training Support) was placed at the T10 level. The weighted kypho-orthosis placed at that level may act through local effect on proprioception of related intervertebral joints (T8, T9, and T10, the commonly involved vertebral bodies) and maintain the gravity line to help balance sensory organization. Therefore, improvement of balance and rehabilitation of proprioception for postural changes may function independent of an increase in muscle strength. The follow-up for this study was not long enough to show postural changes, but follow-up radiographs were obtained to rule out significant radiographic changes such as fracture or subluxation. However, after completion of the study, one control subject (subject 1, group 1) returned to us for physical therapeutic intervention. After 3 mo, she had a decrease in kyphosis (confirmed by radiographic examination) and improved balance. It was of interest that all subjects had a reduced level of pain after participation in the simple back extension exercise program, regardless of group randomization, and that five of the seven subjects had increased their dayto-day level of physical activity. Perhaps these two factors are related in that with less pain subjects were inclined to be more active (Table 1). CONCLUSION The results of this randomized, controlled pilot study suggest that persons with osteoporosis who have abnormal balance and kyphotic posture could benefit more from proprioceptive dynamic rehabilitation with a 246 Sinaki and Lynn weighted kypho-orthosis and back exercise than from back exercise alone. A considerable improvement in balance was noted in subjects who did exercises with PDP training. Improved balance reduces the risk of falls. Although the number of subjects in this study was small, the results are interesting, and further investigation on a larger scale would be helpful. ACKNOWLEDGMENTS We thank the Donaldson Charitable Trust and Marjorie Atwood for support of our research related to osteoporosis and musculoskeletal health. We thank Sandra Fitzgerald for technical support and data compilation. REFERENCES 1. Tinetti ME, Speechley M, Ginter SF: Risk factors for falls among elderly persons living in the community. N Engl J Med 1988;319:1701–7 2. Overstall PW, Exton-Smith AN, Imms FJ, et al: Falls in the elderly related to postural imbalance. BMJ 1977;1:261– 4 3. Hindmarsh JJ, Estes EH Jr: Falls in older persons. Causes and interventions. Arch Intern Med 1989;149:2217–22 4. Wolfson LI, Whipple R, Amerman P, et al: Stressing the postural response. A quantitative method for testing balance. J Am Geriatr Soc 1986;34:845–50 5. Horak FB, Shupert CL, Mirka A: Components of postural dyscontrol in the elderly: A review. Neurobiol Aging 1989; 10:727–38 6. Nguyen TV, Sambrook PN, Kelly PJ, et al: Body sway and bone mineral density are predictors of fracture prevalence: The Dubbo Osteoporosis Epidemiology Study (abstract). J Bone Miner Res 1992;7:S112 7. Hobeika CP: Equilibrium and balance in the elderly. Ear Nose Throat J 1999; 78:558 – 62, 565– 6 8. Matheson AJ, Darlington CL, Smith PF: Further evidence for age-related deficits in human postural function. J Vestib Res 1999;9:261– 4 9. Wolfson L, Whipple R, Derby CA, et al: A dynamic posturography study of balance in healthy elderly. Neurology 1992; 42:2069 –75 10. Lynn SG, Sinaki M, Westerlind KC: Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil 1997;78:273–7 11. Folz TJ, Sinaki M: A nouveau aid for posture training in degenerative CNS disorders (abstract). J Neurol 1992;239 (suppl 2):S20 12. Wahner HW, Riggs BL: Methods and application of bone densitometry in clinical diagnosis. Crit Rev Clin Lab Sci 1986; 24:217–33 13. White AA III, Panjabi MM: Clinical Biomechanics of the Spine, ed 2. Philadelphia, Lippincott, 1990, pp 128 – 68 14. PTS: Posture Training Support (brochure Y32255). Jackson, MI, Camp International, 1993 15. Nashner LM: Computerized dynamic posturography, in Jacobson GP, Newman CW, Kartush JM (eds): Handbook of Balance Function Testing. St. Louis, Mosby Year Book, 1993, pp 280 –307 16. Itoi E: Roentgenographic analysis of posture in spinal osteoporotics. Spine 1991;16:750 – 6 17. Limburg PJ, Sinaki M, Rogers JW, et al: A useful technique for measurement of back strength in osteoporotic and elderly patients. Mayo Clin Proc 1991;66:39 – 44 18. Sinaki M, Wahner HW, Offord KP: Relationship between grip strength and related regional bone mineral content. Arch Phys Med Rehabil 1989;70:823– 6 19. Mathiowetz V, Weber K, Volland G, et al: Reliability and validity of grip and pinch strength evaluations. J Hand Surg (Am) 1984;9:222– 6 20. Sinaki M, Offord KP: Physical activity in postmenopausal women: Effect on back muscle strength and bone mineral density of the spine. Arch Phys Med Rehabil 1988;69:277– 80 21. Kottke FJ: Common cardiovascular problems in rehabilitation, in Kottke FJ, Stillwell GK, Lehmann JF (eds): Krusen’s Handbook of Physical Medicine and Rehabilitation, ed 3. Philadelphia, WB Saunders, 1982, pp 787– 808 22. Nelson ME, Fiatarone MA, Morganti CM, et al: Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA 1994;272:1909 –14 23. Malmros B, Mortensen L, Jensen MB, et al: Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporos Int 1988;8:215–21 24. Muller EA: Influence of training and of inactivity on muscle strength. Arch Phys Med Rehabil 1970;51:449 – 62 Am. J. Phys. Med. Rehabil. ● Vol. 81, No. 4