Running head: MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 1
advertisement

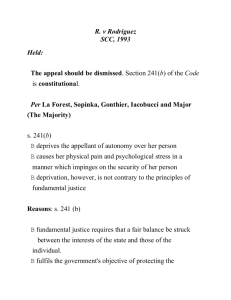
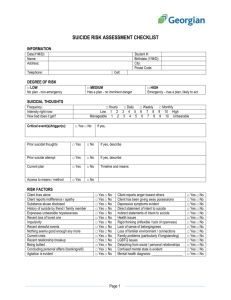
Running head: MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 1 Depression and Suicide: An Underrepresented and Interconnected Mental Health Concern amid Native American Populations Susan Brady University of Colorado Colorado Springs MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 2 Depression and Suicide: An Underrepresented and Interconnected Mental Health Concern amid Native American Populations: “The truth is hard to understand . . . unless, unless . . . you have been yourself to the edge of the Deep Canyon and have come back unharmed.” —a Tewa Indian elder speaking in the 1940s (Laski, 1959) Quantifying the frequency and occurrence of depression and other mental health concerns among Native American Communities often presents a great difficulty. The primary obstacles are that the diagnostic categorizations given carry excessive stigmatization in Native American populations and that the vast preponderance of cases is not counted accurately (Cohen, 2008). People are magnificently complex and complicated. When a label of depression (i.e. a psychiatric condition characterized by such symptoms as an unhappy mood; loss of interests; energy, and appetite; and difficulty concentrating) is employed it indicates the existence of homogeneity in the human experience and a standardization of behavior and symptoms. Simply put, this just isn’t the case (Watson & Breedlove, 2012). Cohen (2008) argues that this inconsistency phenomenon is maintained cross-culturally; depression, sadness, melancholy, grief, heartache, even pain carries distinctive connotations (i.e. meanings, associations, etc.) in other cultures and languages. In Native American languages and dialects, it is reasonable and even rational to state that the lexes of sadness, depression and loneliness are expressive and adjustable rather than analytical and inflexible (Cohen, 2008). Authur Kleinman (1985), a medical anthropologist, cautions that the use of category fallacy (i.e. the assumption that categories in one language carry the same meaning in another) furthers the persistent distrust of western or Indigenous researchers and research being performed. Kleinman (1985) argues that not only are the psychological words (e.g. depression, sadness, etc.) elucidated differently in MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 3 Indigenous societies; they are even comprised and established as distinct “forms of social reality.” This is an especially imperative matter when you consider that most psychological, sociological, etc. studies do not truly consider the diversity of the cultures they are examining (Cohen, 2008). They seem to have limited knowledge or understanding about what some of these matters (e.g. depression, abuse, suicide, and mental illness) constitute in these respective societies and cultures (Cohen, 2008). Depression in Native American communities is reported to be at least as common as in Caucasian populations (Cohen, 2008). In general, Native Americans compared with non-Native Americans are already 28% more likely to commit suicide and in some groups, the number is 10 times higher than the general population (Cohen, 2008). These alarming numbers do not even include suicide attempts. When evaluating other minority populations with Native American communities, the Native American population has an elevated frequency of health risk factors, including suicide (CDC, 2003). These suicidal risk factors include, but are not limited to addiction, mental disorders, recent severe stressful life events, substance abuse, intergenerational mental, emotional, physical and sexual abuse (Middlebrook et al., 2001; Hill (as cited by Vilschick, 2002). There is also evidence that cultural disruption (i.e. socio-historical uprooting from native lands, forcible attendance of boarding schools, loss of native language, and associated weakening of parental and community influence) may perhaps be a significant influencing factor for the elevated rates of suicide amidst Native American communities (Echohawk, 1997; Range et al., 1999). There is a distinct need to assess, recognize and understand suicide from a socio-cultural point of view so that we can identify “culturally specific suicide pathways or trajectories” (Cutcliffe, 2005). This devastating and overwhelming evidence does not just imply that suicide attempts amid Native American communities are taking place, MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 4 but reveals a substantial psychological suffering (Hill, 2009). It is the twenty-first century and we are still excluding and marginalizing Indigenous communities (e.g. Native Americans) from main stream society (Smith, 2012); this happens within the academy as well, along with what researchers choose or choose not to study--this includes the academy of psychology. In these conservative times the role of an Indigenous researcher and indeed of other researchers who are committed to producing research knowledge, who document social injustice, who recover subjugated knowledge, who help to create spaces for the voices of the silenced to be expressed and ‘listened to,’ and who challenge racism, colonialism, and oppression is a precarious responsibility (Smith, 2012). The expectation with this methodical and thematic collation of psycho-sociological based research is that some new data and evidence will be brought into the light. This literature review will primarily address two areas within the realm of psycho-sociological study and within Native American communities--depression and suicide. Depression: Cohen (2008) argues that mental illness is not a uniquely individual crisis; it is also a manifestation of collective bonds and associations, one’s natural (i.e. physical) environment and the socio-political and fiscal structure in which one resides. Additionally, Hill (2009) argues that the experiences of Native Americans on the questions of stress, (i.e. an imbalance between perceived demands and a person’s appraisal of their ability to cope with the demands) depression and suicidal thoughts are rooted in “historical and contextual elements […such as…] historical trauma, colonialization, and the loss of connectedness and cultural practices” (Lazarus, 1993; Hill, 2009). Furthermore, detrimental socio-demographic considerations including economic hardship, violent behavior, and socio-cultural suffering (i.e. “forced relocation and acculturation, societal prejudice, and systematic genocide”) suggest that Native American populations are at MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 5 elevated risk for mental illness and inveterate stress (Rieckmann et al., 2004). Extreme social change (past or recent) damages community integration and kinship and amplifies the risk for depression as well as suicide (Durkheim as cited in Middlebrook et al., 2001). Native American and Euro-American communities are both subject to environmental and biochemical depression. However, there are numerous factors involved in the etiology (i.e. the study of the causes of diseases) of depression that are each more predominant or exclusive to Indigenous communities (See Table 1 below) (Cohen, 2008). Table 1: Etiology of Depression in Native American and First Nations’ Communities Consequences of reservation and urban lifestyle Alcoholism Poverty Battering, rape, child abuse Racism and prejudice from Anglo society and internalized as self-hatred History of abuse perpetrated within residential schools and the church Grief from loss of family members to suicide, violence, or disease Grief from loss of lifestyle, language, and culture Grief from tragic history of one’s tribe and ancestors Loneliness, including separation from family, tribe, land, and nature PTSD (Post-Traumatic Stress Disorder) from any of the above, sometimes spanning generations PTSD from military service and lack of traditional preparation for or healing from the terrors of war Traditional causes Initiatory illness, “the wounded healer” Lack of meaning and purpose Breach of taboo Soul loss Witchcraft/sorcery MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 6 While various illnesses, both physical and psychological, are associated with the above etiological traditional causes, it would probably not be broadly acknowledged or recognized amid today’s Native American populations (e.g. depression vs. soul loss). Cohen (2008) stated that the expression “soul loss” should not be a revelation to those concerned with the treatment or personal experience of depression; “the depressed person appears hollow, without the spark and joy of life.” Even without the knowledge of a particular taboo, a breach could be the source of the depression (Cohen, 2008). However, Cohen (2008) contends that a “lack of meaning and purpose is pandemic today and may be the psychological root of many cases of depression.” From an Indigenous perspective, each life has a purpose, significance and a mission (Cohen, 2008). When a life is unbalanced and inconstant, an individual may experience any number of afflictions. For example, in the Navajo community, a person may experience depression because he or she is suffering from a spiritual imbalance (Rieckmann et al., 2004). This potentially imbalanced volatility can be initiated by neglect to themselves or relationships and can produce anxiety, mood disturbances and depression (Rieckmann et al., 2004). When considering the wide range of treatments for depression there is an obvious differentiation in Western and Indigenous/Native American methods (See Table 2 below). Table 2. Differences between Western and Native American Mental Health Workers Western Methods Native American/Indigenous Focus on disease and diagnostic categories Focus on health and positive words Therapist practices a profession learned through books, Counseling ability may be an inborn gift, may be academic study, and internship conferred through initiation and ceremony, developed in dreams and visions, or learned by observing or apprenticing to noted healers MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 7 Hierarchical view: therapist is an expert and Egalitarian view: all people have challenges; transference authority; transference is common is uncommon Oversight by licensing boards Oversight by community Interventions generally have a serious tone Humor is common Healing accomplished through insight, interpretation, Healing accomplished through insight, interpretation, and/or medication plant medicine, prayer, ceremony, and transpersonal help from spiritual powers; therapist may acquire new skills or power to help a particular patient Therapy practiced in an office Therapy practiced in nature or in a sanctified space Treatment may be prolonged, continuing for years One to four sessions, generally on successive days Advertising, marketing, and networking are keys to Therapist has no shingle, advertising and marketing success may be considered unethical; Patient finds therapist by word-of-mouth and by being in the right place at the right time Fixed fee for services No fees, flexible fees, or donation are common; selfless generosity of healer and patient promotes successful outcome Sessions have fixed length Sessions have no fixed length; may last minutes or hours Therapist never touches the patient Massage, laying on of hands, or other physical gestures may be part of the treatment Focus on coping with, managing, or curing mental Focus on returning to a state of confidence, balance, disease beauty, well-being, and harmonious family and community relations MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 8 As exhibited in the above table, there are critical differences between the Indigenous methodologies and most of the Western methodologies in approaches to therapy and healing (Cohen, 2008). According to Cohen (2003), a customary Native American therapy and counseling option for depression often involves consulting with a sagacious and perceptive elder; the session may or may not include the individual’s spouse or family members. The session could employ various methods of focus: inspiring and constructive words, affirmative imagery, the elder may advise cognitive adjustments in the patient’s mind or may attempt to concentrate on encouraging and hopeful images in his or her own mind to “exert an invisible, transpersonal influence on the patient” (Cohen, 2008; Cohen, 2003). These methods are not what one would typically find in the Western psychology academy, but there are researchers and academics that pursue these ways of doing, thinking, knowing and being. Smith (2012) stated there are researchers that determinedly and resolutely choose to investigate the marginalized members of society; these researchers may come from the very communities that have been cast to the margins of the social order. Sometimes referred to as ‘insider’ research, there is a section of the academy that is concerned with studying the marginalized communities and exposing microcosms of the bigger picture or as paradigms of the societal and cultural pediment (Smith, 2012). This research is necessary if aid is to be found in reducing depression in Native American communities. Suicide: There is a distinct socio-historical perspective that influences and contributes the link between connectedness, a sense of belonging and the instances of suicide in Native American populations, but this matter is yet to explored to its proper depths (Strickland, Walsh, & Cooper, 2006; Hill, 2009). Hill (2009) contends that a sense of belonging is a complicated and intricate MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 9 issue that reflects the interconnected psychological, sociological, physical, and spiritual bonds and unions of individuals, families, and communities. There is a profound transcendent relationship between family, community, nature, the Creator, land, environment, ancestors, and the time-honored customs of life and existence. This deep-rooted relationship is an elemental and central purpose of the Native American community and culture (Struthers et al., 2003 as cited in Hill, 2009). The core risk factors for attempted suicide in adults are depression, alcohol abuse, substance abuse and separation or divorce (National Institute of Mental Health [NIMH], 2004 as cited in Hill, 2009). Frisch and Frisch (2002) characterized suicide as “purposefully taking one's own life” and suicidal ideation as “thoughts of taking one's life”. Alcantara and Gone (2007) contend that by and large, the proportion of suicide ideation and attempts to suicide completion is devastatingly excessive, with a far greater number of cases of suicide ideation and attempts transpiring in comparison to completed suicides. According to Hill (2009), individuals who complete a suicidal act are three times more likely to be men than women. Completers plan the suicide act, whereas suicide attempters tend to act impulsively. Highly lethal methods are more likely to be used by completers compared with suicide attempters. Completers generally select a setting which is isolated to limit disruption, compared with attempters who may notify family and friends and act out their suicide plan in the presence of others (Hill, 2009). However, women are more likely to report a history of attempted suicide, at a ratio of 3:1 (NIMH, 2004 as cited in Hill, 2009). Suicide is a critical public health concern in the United States with current statistics demonstrating that it is the tenth leading cause of death in American society (CDC, 2010). MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 10 In view of the substantial individual and collective toll of death by suicide, the twentyfirst century has observed a substantial increase in nationwide awareness directed with regard to the prevention of suicide (Alcantara & Gone, 2007). Alcantara and Gone (2007) argue that suicide is identified and understood not only as a point of trepidation and worry for individuals and their relations, but also of the community as a whole; this is in conjunction with the cumulative urgency and much needed prioritization of suicide studies, investigations and prevention programs. It is ironic that any ‘‘treatment’’ for suicide must most certainly occur before the actual event of suicide and a postmortem facilitation of intervention is unmistakably impractical and not possible, because suicide prevention cannot be rendered for the dead (Alcantara & Gone, 2007). Because of this Alcantara and Gone, (2007) argue that it is elementary then to discover reliable methods of suicide prevention. This is an imperative for those individuals that might be persuaded to proceed to elevated “suicide risk zones” (Alcantara & Gone, 2007). With this brought to light, the identification of risk factors (i.e. factors that increase the probability of a specific negative outcome) and protective factors (i.e. factors that decrease the probability of a specific negative outcome in the presence of risk factors) within a psychological, biological and sociological framework is crucial in revealing the points of intervention and what determines any one individual’s capacity for suicidal tendencies (Alcantara & Gone, 2007; Giles, 2013). It is also critical that these frameworks realize that specific person-focused intercessions especially those which include the act of “victim blaming” should be severely prohibited; instead the primary focus should be on the problematical and complex interactions of the people and their environment (Alcantara & Gone, 2007). However, the recent emphasis on suicide prevention endeavors has unfortunately been rather arduous and has experienced delay in reaching Native American communities at the greatest risk. Optimistic MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 11 results, though projected, are not warranted or secured (Alcantara & Gone, 2007). Freedenthal and Stiffman (2004) findings suggest that there may indeed be a geographical based set of factors that influence Native American communities either to or away from acts of suicide and suicidal ideation. In their research of both reservation-based and urban-based individuals, there was a statistically significant heightened level of suicidal ideation among those individuals who had spent at least two-thirds of their lives on a reservation versus those individuals who had spent at least two-thirds of their lives in an urban environment; however, Freedenthal and Stiffman (2004) did find that their suicide attempts over their lifetime, both urban and reservation-based individuals, was equal indicating that there may be an Indigenous cultural or societal component connection to increased levels of suicide, suicide attempts, and suicidal ideation. However, what was so strikingly different was the contrast in the inventories of risk factors that correlated respectively with each of the urban-based and reservation-based samples: Urban-Based Risk Factors for Suicide and Attempted Suicide found by Freedenthal and Stiffman (2004): History of physical abuse A friend attempting or completing suicide Family history of suicidality Reservation-Based Risk Factors for Suicide and Attempted Suicide found by Freedenthal and Stiffman (2004): Depression Conduct Disorder Cigarette smoking Low self-esteem Family history of substance abuse Lower perceived social support Single-parent household Perceived discrimination MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 12 While very few studies with the exception of that by Freedenthal and Stiffman (2004), have investigated and even considered “perceived discrimination” as it connects to suicidal actions and tendencies. Discrimination, prejudice and conventional distress have been formerly cited as risk factors for suicidal conduct and behaviors in Native American communities (Johnson, 1994). Hill (2009) argued that ultimately balance, connectedness or disconnectedness within the community, which is more often the case, is often at the core of the depressive and suicidal behaviors among Native American populations. Discussion: Alcantara and Gone, (2007) described some of the more deeply rooted ecological and generational origins of depression and suicide in Native American communities. The legacy of colonization (referred to as historical trauma, soul wound, intergenerational trauma, historical legacy, American Indian holocaust, and historical unresolved grief) has been offered as a paradigm for understanding and explaining the alarming prevalence rates of mental disorders and social problems—with much attention devoted to its role in suicide—that have beleaguered Native American populations for generations both past and present (Alcantara & Gone, 2007). This literature review of the psychological, biological, and social risk factors for suicide and depression in Native American communities demonstrates that the factors affecting and influencing Indigenous persons to an elevated risk zone are intricate, deep and very complicated. Risk factors for suicide and depression do not exist in seclusion; they exist intersectionally and as an amalgamation of factors. It is a network of “genetic linkages, psychiatric conditions, Native identity, social support networks, attitudes toward education, cultural continuity, spirituality, and MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 13 socioeconomic factors” that are associated and interconnected with depression and suicidality in Native American populations (Alcantara & Gone, 2007). Beck, Walters, and Francisco (1990) argued that one of the most central concepts that Native American people impart is the belief and connection to the philosophies of balance and imbalance. Beck, et al. (1990) explained that “disease is seen as a part of the total environment which includes the individual, the community, the natural world, and the world of ancestors and spirits.” The problem is that the basic and fundamental methodologies, ontologies, axiologies, and epistemologies of Native American populations are not being researched, investigated or examined enough to meet an ever growing epidemic. The academy educates and expects that its research will direct and control societal renovation and change; however, when considering that the crucial and significant issue at hand is that academic research has not shown or established that it can truly benefit Indigenous communities. Instead the prospective “benefits” rarely, if ever, reach the Indigenous communities or are used as deceptive maneuvers or strategies in order to pressure or compel the communities into surrendering their traditional values, vacating their homes, being stripped of their languages and being deprived of basic power over choices and judgments in their own lives (Smith, 2012). Ultimately, the research academy “exists within a system of power” (Smith, 2012). There is an imperative demand not just for Indigenous research, but Indigenous researchers to explore these matters of depression and suicide amid Native American communities. It is fundamental that both Indigenous and non-Indigenous researchers should create and establish an ecologically, culturally and ethnically sensitive psycho-bio-social framework; this framework is not only essential in establishing much needed interventions for depression and suicide, but to actually reduce the number of risk factors and to dramatically MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 14 increase the number of protective factors available to Native American communities. The Native American communities need an ecologically, culturally and ethnically sensitive psycho-biosocial framework that expresses and illustrates even the most elementary and deep-rooted belief practices so that their culture and society can be restored to a place of balance, connection, and unity. MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 15 References Alcantara, C., & Gone, J. (2007). Reviewing suicide in Native American communities: Situating risk and protective factors within a transactional-ecological framework. Death Studies, 31, 457-477. Beck, P. V., Walters, A. L., & Francisco, N. (1990). The sacred: ways of knowledge, sources of life (Redesigned ed.). Tsaile, Ariz.: Navajo Community College Press. Centers for Disease Control. (2003). Health status of American Indians compared with other racial/ethnic minority populations—selected states, 2001—2002. Centers for Disease Control. (2010). Fast stats. Suicide and Self-Inflicted Injury. Cohen K. Honoring the medicine: The essential guide to Native American healing. New York, NY: Ballantine Books; 2003. Cohen, K. S. (2008). At the canyon’s edge: Depression in American Indian culture. Explore: The Journal of Science and Healing, 4, 127-135. Cutcliffe, J. (2005). Toward an understanding of suicide in First-Nation Canadians. Crisis, 26(3), 141−145. Echohawk, M. (1997). Suicide: The scourge of Native American people. Suicide and LifeThreatening Behavior, 27, 60−67. Freedenthal, S. & Stiffman, A. R. (2004). Suicidal behavior in urban American Indian adolescents: A comparison with reservation youth in a southwestern state. Suicide and Life-Threatening Behavior, 34, 160–171. Frisch, N., & Frisch, L. (2002). Psychiatric mental health nursing (2nd ed.). New York: Delmar. Giles, J. (2013, November 13). Introduction to Gender. Psychology of Women. Lecture conducted from University of Colorado Colorado Springs, Colorado Springs. MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS 16 Hill, Doris Leal. (2009). "Relationship between sense of belonging as connectedness and suicide in American Indians." Archives of Psychiatric Nursing 23, 65-74. Johnson, D. (1994). Stress, depression, substance abuse, and racism. American Indian and Alaska Native Mental Health Research, 6, 29–33. Kleinman, A., Good, B. (1985) Culture and depression: Studies in the anthropology and cross-cultural psychiatry of affect and disorder. Berkeley, CA: University of California Press; 492. Laski V. Seeking Life. Austin, Tex: University of Texas Press; 1959:128. Lazarus, R. S. (1993). Coping theory and research: Past, present, and future. Psychosomatic Medicine, 55, 234–247. Middlebrook, D., LeMaster,P., Beals, J., Novins, D.,& Manson,S. (2001). Suicide prevention in American Indian and Alaska Native communities: A critical review of programs. Suicide and Life-Threatening Behavior, 31, 132−149. Range, L., Leach, M., McIntyre, D., Posey-Deters, P., Marion, M., Kovac, S., Banos, J., & Vigil, J. (1999). Multicultural perspectives on suicide. Aggression and Violent Behaviors, 4, 413−430. Rieckmann, T. R., Wadsworth, M. E., & Deyhle, D. (2004). Cultural identity, explanatory style, and depression in Navajo adolescents.. Cultural Diversity & Ethnic Minority Psychology, 10, 365-382. Smith, L. T. (2012). Decolonizing methodologies. London, UK: Zed Books. Strickland, C., Walsh, E., & Cooper, M. (2006). Healing fractured families: Parents' and elders' perspectives on the impact of colonization and youth suicide prevention in a Pacific Northwest American Indian tribe. Journal of Transcultural Nursing, 17, 5−12. MENTAL HEALTH AND NATIVE AMERICAN POPULATIONS Watson, Neil V., and S. Marc Breedlove. The mind's machine: foundations of brain and behavior. Sunderland, Mass.: Sinauer Associates, 2012. Print. Wilson, S. (2001). What is an indigenous research methodology?. Canadian Journal of Native Education, 25, 175-179. 17



![Suicide Warning Signs and What to Do [DOC]](http://s2.studylib.net/store/data/010144476_1-4957ca456e56c4f2d4792a0046125d72-300x300.png)