Suicide Risk Assessment Checklist – Georgian College
advertisement
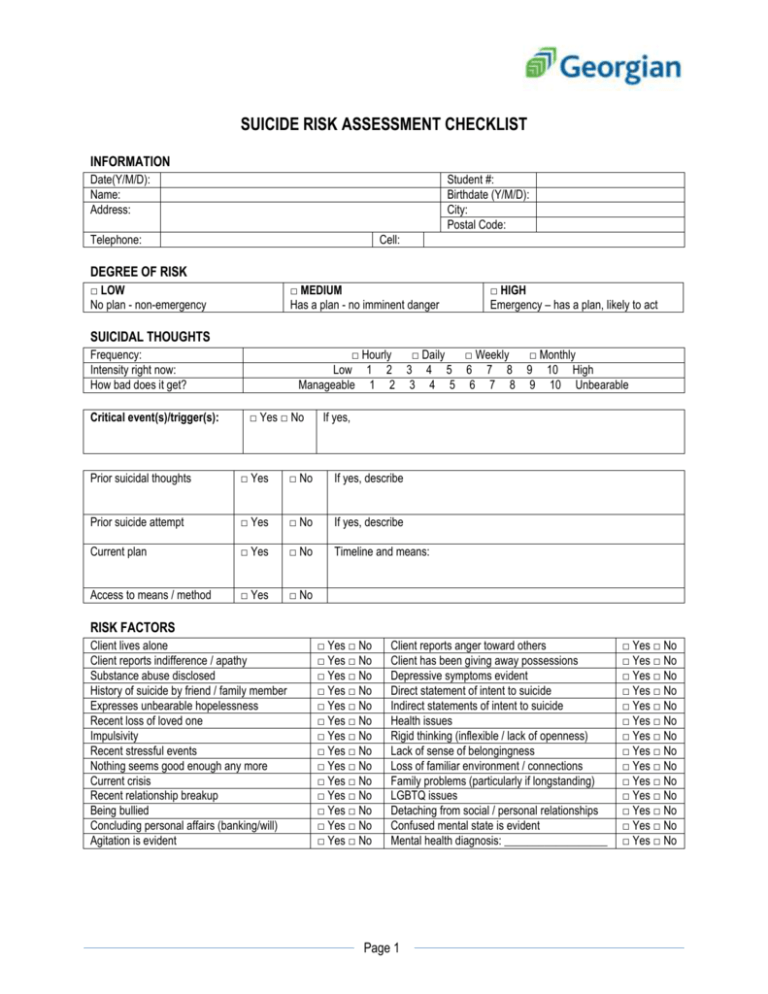
SUICIDE RISK ASSESSMENT CHECKLIST INFORMATION Date(Y/M/D): Name: Address: Student #: Birthdate (Y/M/D): City: Postal Code: Telephone: Cell: DEGREE OF RISK □ LOW No plan - non-emergency □ MEDIUM Has a plan - no imminent danger □ HIGH Emergency – has a plan, likely to act SUICIDAL THOUGHTS Frequency: Intensity right now: How bad does it get? Critical event(s)/trigger(s): □ Hourly □ Daily □ Weekly □ Monthly Low 1 2 3 4 5 6 7 8 9 10 High Manageable 1 2 3 4 5 6 7 8 9 10 Unbearable □ Yes □ No If yes, Prior suicidal thoughts □ Yes □ No If yes, describe Prior suicide attempt □ Yes □ No If yes, describe Current plan □ Yes □ No Timeline and means: Access to means / method □ Yes □ No RISK FACTORS Client lives alone Client reports indifference / apathy Substance abuse disclosed History of suicide by friend / family member Expresses unbearable hopelessness Recent loss of loved one Impulsivity Recent stressful events Nothing seems good enough any more Current crisis Recent relationship breakup Being bullied Concluding personal affairs (banking/will) Agitation is evident □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No Client reports anger toward others Client has been giving away possessions Depressive symptoms evident Direct statement of intent to suicide Indirect statements of intent to suicide Health issues Rigid thinking (inflexible / lack of openness) Lack of sense of belongingness Loss of familiar environment / connections Family problems (particularly if longstanding) LGBTQ issues Detaching from social / personal relationships Confused mental state is evident Mental health diagnosis: __________________ Page 1 □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No CONTRAINDICATIONS A viable support system is available Moral / religious restraints against suicide History of physical / emotional wellbeing Upon recovery, satisfying life situation exists □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No Maintaining contact with significant others Signs of affective openness and rapport Positive attitude toward personal responsibility Is receiving mental health care □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No Available resources: ACTION TAKEN Advised of emergency department Provided crisis line / Good Talk contact information Accompanied to emergency department Contacted CMHA Mobile Crisis Team Contacted police / 911 Contacted family doctor Contacted family / friends / partner Consulted with ____________________________________________ Position ________________________ Counselling appointment scheduled Other (describe): Consent form(s) attached □ Family □ Friend □ Physician □ Therapist □ Other: ______________________ □ Consent refused FOLLOW UP PLAN Therapist: Date (Y/M/D): Page 2 □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No







![Suicide Warning Signs and What to Do [DOC]](http://s2.studylib.net/store/data/010144476_1-4957ca456e56c4f2d4792a0046125d72-300x300.png)