AbstrAct than with IM nails. this result is likely multifacto-
advertisement

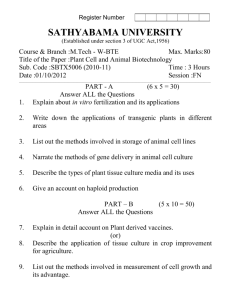
Stabilization of Distal Femur Fractures with Intramedullary Nails and Locking Plates: Differences in Callus Formation Christopher E. Henderson, MD,* Trevor Lujan, PhD,** Michael Bottlang, PhD,** Daniel C. Fitzpatrick, MD,† Steve M. Madey, MD,† J. Lawrence Marsh, MD* Abstract Objectives: This study compared callus formation in distal femur fractures stabilized with locking plates and intramedullar y nails to test the hypothesis that locking plates induce less fracture callus than IM nails. Design: Retrospective case matched study. Setting: Two orthopaedic trauma centers. Patients: 174 distal femur fracture were reviewed to extract cases treated with retrograde IM nails (NAIL group, n=12). These were then individually matched to cases treated with locking plates (Plate group, n=12). Inter vention: Retrograde IM nailing or locking plate fracture fixation. Outcome Measures: Periosteal callus was measured on lateral and antero-posterior radiographs taken at 12 weeks after injur y using validated software to objectively extract the size of peripheral callus from digital radiographs. Results: The NAIL group had 2.4 times more callus area per location (231 ± 304 mm2) than the PLATE group (95 ± 109 mm2, p=0.028). Compared to the PLATE group, the NAIL group had 3.4 times more callus anteriorly (p=0.31), 2.6 times more callus posteriorly (p=0.25), and 2.3 times more callus medially (p=0.16). At 12 weeks after injur y, no or minimal callus for secondar y bone healing (<20 mm2) was present in 20% of callus locations in the NAIL group and in 54% of callus locations in the PLATE group. Conclusion: Significantly less periosteal callus formed in fractures stabilized with locking plates Orthopaedics and Rehabilitation, University of Iowa Hospital and Clinics, Iowa City, IA 52242 ** Biomechanics Laboratory, Legacy Research & Technology Center, Portland, OR 97232, † Slocum Center for Orthopaedics, Eugene, OR, 97401 Corresponding Author: J Lawrence Marsh, MD Department of Orthopaedics and Rehabilitation University of Iowa Hospitals and Clinics 200 Hawkins Drive, Iowa City, IA 52242 Phone: (319)-653-0430; fax (319)-353-6754; email:j-marsh@uiowa.edu * than with IM nails. This result is likely multifactorial and further study of the interaction between construct stif fness and fracture healing in the distal femur is warranted. Introduction Fractures of the distal third of the femur are a treatment challenge despite new fixation options. Fixed angle locking plates have become the most commonly used device for this indication replacing intramedullary nails, blade plates and condylar screws.1 Despite widespread use, there are few studies that directly compare locking plates to more traditional techniques. Locking plates have been developed in conjunction with a minimally invasive biologically friendly insertion technique which allows the plate to be placed without excessive soft tissue-stripping and with minimal disruption of the bone blood supply.1,2 Similar to intramedullary nails these plates are used to span zones of comminution which then must heal with an external callus. They have been designed to limit fracture gap strain with physiologic loads and have improved fixation in osteoporotic, cancellous, or comminuted bone.1-3 One concern with locking plate constructs is that the high stiffness achieved may limit the amount of callus, resulting in delayed healing or nonunion.4-6 For comminuted fractures treated with a bridging technique, peripheral callus is necessary for fracture healing.7-9 To our knowledge there have not been any studies that have directly compared the amount of callus formed with locking plates to that formed with other implants used to treat distal femur fractures such as intramedullary nails. Intramedullary nails have many of the same advantages as locking plates such as percutaneous placement without disruption of blood supply, indirect fracture reduction, success in osteoporotic bone and have been reported to lead to high healing rates in fractures of the distal femur.10-14 There is also evidence that intramedullary nails are less stiff than locking plates.15,16 The purpose of this study was to quantitatively measure callus formation and use it as an outcome assessment to compare two clinical techniques used to stabilize distal femur fractures. We hypothesized that the increased stiffness of locking plate fracture constructs leads to less fracture callus than similar constructs with Volume 30 61 C. E. Henderson, T. Lujan, M. Bottlang, D. C. Fitzpatrick, S. M. Madey, J. L. Marsh Table 1. Demographic and radiologic criteria used for patient matching are reported demonstrating closely matched NAIL and PLATE pairs intramedullary nails. This hypothesis was tested with a retrospective case matched study design. Patients and Methods Approval from the investigational review board for our institutions was obtained. Patients treated for distal femur fractures between 1998 and 2006 at the University of Iowa and Slocum Center for Orthopaedics were identified by searching the Current Procedural Terminology (CPT) coding records of the hospital for distal femur fracture repair. These diagnoses were confirmed by review of the medical records. One hundred seventy four distal femur fractures were initially identified. Of these forty six were primarily fixed with a femoral retrograde intramedullary nail. Revision cases, periprosthetic fractures below a total hip arthroplasty, patients with incomplete records, missing or poor quality radiographs, or follow up less than 12 weeks were excluded. Fifteen patients met appropriate criteria (NAIL group). 62 The Iowa Orthopaedic Journal Baseline characteristics of the patient and the fracture were identified from the medical record including age, gender, type of fracture fixation, open vs. closed fracture, periprosthetic fracture (above total knee), and comorbidities such as diabetes and smoking. Injury radiographs were reviewed for OTA fracture classification,17 postoperative radiographs were reviewed to confirm documented treatment, and 12 week anteroposterior and lateral radiographs were used for callus measurement. A comparison group of patients treated with locking plates were identified from the original patient cohort (PLATE group). The NAIL group of patients were individually matched to the patients treated with locking plates according to OTA classification, age, gender, open versus closed fracture, periprosthetic fracture, smoking, and diabetes (Table 1). We accepted only exact matches for OTA classification. Three NAIL patients did not have an acceptable PLATE match and were not used. All patients were exact matches for smoking status. Stabilization of Distal Femur Fractures with Intramedullary Nails and Locking Plates Eleven of 12 patients were exact matches based on open versus closed fracture; one patient in the NAIL group had a Gustillo type 1 open fracture and was matched to a closed fracture in the PLATE group. Two of 12 patient matches differed in the presence of diabetes. One periprosthetic fracture in the NAIL group was matched to a nonperiprosthetic fracture in the PLATE group. Patient age was matched closely however exact matches were not possible. The average age difference among matched patients was eight years and only three patient matches differed by greater than 10 years. Four patients had all variables matched, five had only a difference in gender, and three had two variables unmatched, no patient pairs had greater than two unmatched variables. The patient charts and all available radiographs were reviewed for complications including superficial or deep infection, hardware failure or removal, malunion, nonunion, need for revision surgery, and time to weight bearing. Coronal alignment was measured as the angle between a line bisecting the distal femur shaft and a line parallel to the proximal tibial plateau. Normal coronal alignment was considered 5˚-7˚ valgus, and normal sagittal alignment was neutral. Malalignment was defined as greater than a 5˚ deviation from normal coronal or sagittal alignment. Loss of alignment was defined as greater than a 3˚ change in angular measurements between postoperative and follow-up radiographs. The peripheral callus was measured on lateral and antero-posterior radiographs at 12 weeks in all fractures (Figure 1). The callus measurement technique has been previously described and validated.6,18 Briefly, custom software extracted the projected area of periosteal callus by using regional pixel intensities and pixel gradients. Callus size was converted from pixels to metric area by using an implant feature of known dimension. The algorithm has less than a 5% error in measuring callus area and the algorithm strongly correlated with orthopaedic surgeons that manually traced the callus outline (r=0.94).18 In the NAIL group, the projected callus area at the anterior, posterior, medial and lateral location was measured (41 fracture sites). In the PLATE group, callus at anterior, posterior and medial locations was measured (31 fracture sites). Callus at lateral locations could not be measured since the plate was inserted on the lateral cortex. If multiple fractures could be observed on one cortical location, periosteal callus was measured at all fracture sites and an average was taken. The amount of callus at each location (anterior, posterior, medial) was compared between the NAIL and PLATE group. Fractures were stratified by OTA classification, open vs. closed, and union vs. nonunion for further comparison. Statistical analysis was performed using Fisher’s exact test and Student’s t test. All com- Figure 1. Periosteal callus measurement in matched plate and nail cases at week 12. A) No periosteal callus on medial cortex. B) Bridging periosteal callus on lateral cortex. parisons were two-tailed and the significance level was set at 0.05. Results The results of the chart review and matching process are presented in Table 2. No significant differences were found between the NAIL and PLATE groups baseline characteristics. Ten fractures in each group were treated with a minimally invasive approach with closed reduction of the metaphyseal fracture, two fractures in each group required open reduction of an articular component or irrigation for open fracture. In the NAIL group seven fractures were treated with Trigen retrograde femoral nails (Smith and Nephew; Memphis, TN), four with Stryker T2 retrograde nails (Stryker; Kalamazoo, MI), one with a Synthes Retrograde Femoral Nail (Synthes; Paoli, PA), and one with a GSH (Smith and Nephew; Memphis, TN). All IM nails were crosslocked with a range of one to four cross lock screws distally (avg = 2.3) and zero (one nail) to two cross locks proximally (avg = 1.2). The nail diameters ranged from 11.5 - 13 mm (avg = 12.6mm) and all nails were inserted after overreaming the canal by 0.5 to 1.5 mm (avg = 1.2). The locking plates utilized included five Less Invasive Stabilization System (LISS; Synthes: Paoli, PA), four Synthes LCP compression plates (Synthes; Paoli, PA) and three PERILOC Distal Femur Plates (Smith and Nephew; Memphis, TN). Of these plates, seven were constructed of stainless steel (Synthes LCP compression plate, PERI-LOC Distal Femur Plate) and five were titanium (LISS, Polyaxial Volume 30 63 C. E. Henderson, T. Lujan, M. Bottlang, D. C. Fitzpatrick, S. M. Madey, J. L. Marsh Table 2. Clinical results and complications comparing patients treated with intramedullar y nails (NAIL) to locking plates (PLATE) NAIL (averages) Follow up Age 67 weeks (12-144) Weight 89 kg (57-109) Fall - 10 MVC - 2 Mechanism of injury Knee ROM 2º-97º Time to weight bearing 97 kg (57-157) Fall -10 MVC -1 Crush – 1 0º-99º 1/12 (8%) Sagittal malalignment ∆ Alignment >3º Delayed union Secondary surgery 0.63 0 3/12 (25%) 0.59 0 1/12 (8%) 2/12 (17%) 0 0 4/12 (33%) 2- nonunion revision 2- crosslock removal 2/12 (17%) 1- nonunion revision 1- total knee arthroplasty distal femur plate). The plates ranged in size from nine to 13 holes, average plate size was 10 holes. Several subgroups were analyzed in an attempt to identify factors that may affect callus formation. We found no obvious relationship between nail diameter, amount of overreaming, canal fill, or the number of proximal or distal crosslock screws. We also could not identify a difference in callus formation in stainless steel compared to titanium plates, or screw/hole ratio. Statistical analysis was limited by small group numbers. Peripheral callus was found to be significantly greater in the NAIL group compared to the PLATE group at 12 weeks postoperatively. The average callus per fracture location in the NAIL group was 233 mm2 and in the 64 The Iowa Orthopaedic Journal 0.77 0.54 1.0 1.0 1.0 1.0 1/12 (8%) Nonunion 0.65 11 weeks 0 5º-10º coronal malalignment Infection 65 years (25-96) 12 weeks p value 57 weeks (16-120) 63 yrs (23-87) PLATE (averages) 1/12 (8%) 1/12 (8%) 0.64 PLATE group was 95 mm2 (p = 0.04) [Figure 2A]. The NAIL group had more callus formation on the anterior, posterior, and medial cortices (p = 0.25, 0.31, 0.16) [Figure 2B]. The NAIL group had 226 ± 236 mm2 of callus on the lateral cortex. The largest amount of callus was found at the medial cortex and the smallest amount of callus was found at the anterior cortex in both groups. In the 12 matched pairs, the NAIL group had a greater average callus amount in eight of the pairs (67%) and the PLATE group had a greater average callus amount in four of the pairs (33%) at week 12 (p = 0.22). The average amount of callus per femur varied widely in both groups. The NAIL group varied from 37 mm2 to 953 mm2 (mean=231 mm2) and the PLATE group varied Stabilization of Distal Femur Fractures with Intramedullary Nails and Locking Plates Figure 2. Average callus size in NAIL and PLATE cases. A) The NAIL group had over 2-fold more callus than the PLATE group (p=0.04). B) Distribution of mean callus area at each cortical location. Circular depiction of callus area scaled to the cross-sectional area of an average human femur.29 from 0 mm2 to 227 mm2 (mean=87 mm2). Several of the fractures in the NAIL group formed a large amount of callus exceeding 500mm2 at a single anatomic site. No fractures in the PLATE group formed this large amount of callus. A considerable number of fractures treated with locking plates formed no or very little callus. Ranking periosteal callus by size increments of 20 mm2 demonstrated that 17/31 (55%) fracture sites (ant, post, med on AP and Lateral radiographs) in PLATE cases had between 0-20 mm2 of callus, while only 9/41 (22%) fracture sites (ant, post, med, lat on AP and Lateral radiographs) in NAIL cases had between 0-20 mm2 of callus (p<0.01) [Figure 3A]. There were similar differences between the NAIL and the PLATE groups at all anatomic locations with the largest difference found anteriorly [Figure 3B]. There was no significant difference in peripheral callus formation between open versus closed fractures. Open fractures had an average of 135 mm2 compared to 83 mm2 in closed fractures (p = 0.35). There was no significant difference in callus between cases stratified by the OTA classification. The more comminuted fractures were 33A3 - 103 mm2 and 33C3 - 125 mm2 and the less comminuted 32A2 - 24 mm2 and 33C1- 89 mm2 (p=0.07). There were no hypertrophic nonunions, in fact the four fractures that went on to nonunion formed very little callus (Nail four: 40 mm2, Nail nine: 187 mm2, Plate seven: 6 mm2, Plate nine: 0 mm2). One nonunion was in an open fracture, two were in patients with diabetes, and none of the nonunion patients were smokers. Two of the nonunions were in a case matched pair. All of the nonunions occurred in the most comminuted classifications, 32A3 or 33A3. Given the small number of nonunions we could not identify other obvious mechanical or biological factors that contributed to this adverse outcome. Discussion Despite the widespread use of locking plates to fix distal femur fractures, evidence has not emerged demonstrating that these devices are superior to previously established methods. A systematic review comparing traditional plating, intramedullary nails, and locking plates found no observed differences between implants in the rate of nonunion, infection, fixation failure, or revision surgery.19 However subgroup analyses suggested an increased risk of fixation failure and revision surgery with locking plates compared to conventional plates but a reduced infection rate.19 Herrera et al. in a systematic review of 29 case series with a total of 415 distal femur fractures found a 1.5% rate of nonunion with intramedullary nailing compared to a 5.3% rate with locked plates.20 In a prospective study, intramedullary nails and locking plates were found to have equivalent functional outcome scores.14 Secondary bone healing requires only relatively stable fixation that results in some interfragmentary movement to stimulate callus formation.7 There has been recent concern that locking plates may be too stiff suppressing the callus necessary for bridging by secondary healing.4-6 In distal femur fractures treated with locked plates, Lujan et al. demonstrated asymmetric callus, with the majority of callus forming medially away from the plate where there is more motion. Less callus was found with stiff stainless steel constructs and those with more holes Volume 30 65 C. E. Henderson, T. Lujan, M. Bottlang, D. C. Fitzpatrick, S. M. Madey, J. L. Marsh Figure 3. Periosteal callus distribution: A) At 12 weeks post surger y, 54% of PLATE cases had no or ver y little callus (≤20 mm2). B) Percentage of fractures with callus size greater than 20 mm2 at each cortical location. filled compared to less stiff titanium constructs and those with empty holes near the fracture gap.6 Sanders et al. reported more nonunions in stainless steel plates, 23%, compared to titanium plates, 7% (p=0.05).4 Locking plate constructs can be several fold stiffer than external fixators and they can be as stiff as traditional plating constructs designed to promote primary bone healing by restricting interfragmentary motion.21-23 Biomechanical studies have evaluated the stiffness and interfragmentary motion of intramedullary nails and locking plate constructs, however there have been no direct comparative studies. Bottlang et al. showed only 0.2 mm of motion with axial loading under body weight with a locked plate construct.15 A study of gap motion comparing short and long cross locked supracondylar nails showed fracture gap motion ranging from 1.8 mm to 13.6 mm depending on nail length and the number of proximal cross lock screws.24 These studies indicate that locking plates can be substantially stiffer than intramedullary nails but there have been other biomechanical studies where the differences are less clear.15,16,25,26 Locking plate constructs appear to have an asymmetric but greater axial displacement than nails with varus loading, however nails have greater total gap motion, especially in response to torsion and shear stress resulting in increased shear strains.15,16,24-26 In this case matched study an overall smaller amount of callus was formed by fractures treated with locking plates and there were a greater number of plate cases that formed little or no callus in the absence of identifiable biologic differences. In comparison to intramedullary fixation, a locking plate fracture construct may decrease the amount of callus formation by limiting 66 The Iowa Orthopaedic Journal interfragmentary motion. The fractures that failed to unite formed very little callus indicating that bridging periosteal callus is necessary for fracture healing. We found that the least callus was anterior in our plated fractures and the most callus was medial. The anterolateral position of the locking plate may limit the callus formed anteriorly and laterally by proximity of these cortices to the plate with increased local stiffness relative to the medial cortex which is farther from the plate. The IM nails in this study had an average of 1.2 proximal cross lock screws leading to less stability and more interfragmentary motion than if they had more locking screws.24 The preparation for and insertion of the nails may also have been factors that stimulated callus in the NAIL group compared to the PLATE group due to extravasation of medullary contents. This offers another plausible reason for the differences in callus seen in this study. Regardless of the reason, the results suggest that in metaphyseal fractures of the distal femur treated without anatomic reduction and compression fixation which require external callus to heal, locking plates produce less callus than IM nails. One important limitation to the study is that there were an equal number of nonunions in both groups and we acknowledge that fracture union is the critical endpoint. However to the extent that union requires callus, measuring callus could predict subsequent delayed or nonunions, determine the need for secondary intervention, and assess differences in implants and techniques with a smaller number of patients than would be necessary for union as an outcome. The differences in callus between the two groups was also not as clear and distinct as looking at the series wide average would suggest. Stabilization of Distal Femur Fractures with Intramedullary Nails and Locking Plates Several nail cases made a large amount of callus resulting in a wide standard deviation. In addition, in four of the matched pairs the plated cases actually had more callus than the nailed cases.This study has several other limitations. It is a retrospective design and a number of patients had to be excluded due to inadequate follow up or poor radiographs resulting in small patient numbers. The majority of our supracondylar femur fractures have been treated with locking plates since 2002, which limited the number of nail cases available for study secondary to a standing hospital policy to destroy radiographs after seven years of storage. Despite our rigorous matching criteria it is possible that patient or biological factors within a matched pair differed enough to effect callus formation to a greater degree than method of fixation. Measuring callus on plain radiographs has limitations including using a two dimensional study to estimate what is a three-dimensional biological process, however radiographs have been shown to effectively approximate callus growth.6,18,27 It is possible that biologic or other mechanical factors not identified in this study contribute to increased callus formation with IM nails. Therefore the results of our study should be interpreted with caution and used as a starting point for further investigation. In conclusion, in this study locking plates used to bridge fractures of the distal femur led on average to less callus formation than IM nails. Further study of the interaction between construct stiffness and fracture healing in the distal femur is warranted. References 1. Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am 2006 Dec: 88 Suppl 4:189-200. 2. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma 2004 Sep: 18(8):488-93. 3. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 2002. 84:1093-110. 4. Sanders et al. Titanium versus stainless steel locked plates for distal femur fractures: is there any difference? Orthopedic Trauma Service, Florida Orthopedic Institute, Tampa Florida, USA. Orthopaedic Trauma Association 2008 abstract. 5. Henderson CE, Bottlang M, Marsh JL, Fitzpatrick DC, Madey SM. Does locked plating of periprosthetic supracondylar femur fractures promote bone healing by callus formation? Two cases with opposite outcomes. Iowa Orthop J 2008: 28:73-6. 6. Lujan T, Henderson CE, Madey SM, Fitzpatrick DC, Marsh JL, Bottlang M. Locked plating of distal femur fractures leads to inconsistent and asymmetrical callus formation. JOT in press. 7. Claes LE, Heigele CA, Neidlinger-Wilke C, Kaspar D, Seidl W, Margevicius KJ, Augat P. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res 1998 Oct: (355 Suppl):S132-47. 8. Duda GN, Sollmann M, Sporrer S, Hoffmann JE, Kassi JP, Khodadadyan C, Raschke M. Interfragmentary motion in tibial osteotomies stabilized with ring fixators. Clin Orthop Relat Res 2002 Mar;(396):163-72. 9. Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br 1985 Aug: 67(4);67:650-5. 10. Hartin NL, Harris I, Hazratwala K. Retrograde nailing versus fixed-angle blade plating for supracondylar femoral fractures: A randomized controlled trial. ANZ J Surg. 2006 May: 76(5): 290-4. 11. Armstrong R, Milliren A, Schrantz W, Zeliger K. Retrograde interlocked intramedullary nailing of supracondylar distal femur fractures in an average 76-year-old patient population. Orthopaedics 2003 Jun: 26(6):627-9. 12. Dunlop DG, Brenkel IJ. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury 1999 Sep: 30(7):475-84. 13. Fitzpatrick DC, Door nink J, Madey SM, Bottlang M. Relative stability of conventional and locked plating fixation in a model of the osteoporotic femoral diaphysis. Clin Biomech (Bristol, Avon). 2009 Feb;24(2):203-9. 14. Markmiller M, Konrad G, Sudkamp N. FemurLISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res 2004 Sep: (426):252-7. 15. Bottlang M, Doornink J, Fitzpatrick DC, Madey SM. Far cortical locking can reduce stiffness of locked plating constructs while retaining construct strength. J Bone Joint Surg Am 2009 Aug;91(8):198594. 16. Augat P, Penzkofer R, Nolte A, Maier M, Panzer S, v Oldenburg G, Pueschl K, Simon U, Buhren V. Interfragmentary movement in diaphyseal tibia fractures fixed with locked intramedullary nails. J Orthop Trauma 2008 Jan: 22(1):30-6. 17. Orthopaedic Trauma Association Committee for Coding and Classification. Fracture and Dislocation Compendium. J Orthop Trauma 1996;10(suppl):51-5. Volume 30 67 C. E. Henderson, T. Lujan, M. Bottlang, D. C. Fitzpatrick, S. M. Madey, J. L. Marsh 18. Lujan TJ, Henderson CE, O’Donovan M, et al. in ASME Summer Bioengineering Conference Lake Tahoe, CA, June 17-21; 2009, Abstract #206826. 19. Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma. 2006 May: 20(5):366-71. 20. Herrera DA, Kregor PH, Cole PA, Levy B, Jonsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: Systematic review of 415 cases (1981-2006). Acta Orthopaedics 2008 Feb: 79(1):22-7. 21. Peindl RD, Zura RD, Vincent A, Coley ER, Bosse MJ, Sims SH. Unstable proximal extraarticular tibia fractures: a biomechanical evaluation of four methods of fixation. J Orthop Trauma 2004 Sep: 18(8):540-5. 22. Wagner M. General principles for the clinical use of the LCP. Injury 2003 Nov: 34 Suppl 2:B31-42. 23. Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP—how can stability in locked internal fixators be controlled? Injury 2003 Nov: 34 Suppl 2:B11-9. 68 The Iowa Orthopaedic Journal 24. Sears BR, Ostrum RF, Litsky AS. A mechanical study of gap motion in cadaveric femurs using short and long supracondylar nails. J Orthop Trauma 2004 Jul;18(6):354-60. 25. Heiney JP, Barnett MD, Vrabec GA, Schoenfeld AJ, Baji A, Njus GO. Distal femoral fixation: A biomechanical comparison of trigen retrograde intramedullary (I.M) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate. J Trauma 2009 Feb: 66(2):443-9. 26. Bong MR, Egol KA, Koval KJ, Kummer FJ, Su ET, Iesaka K, Bayer J, Di Cesare PE. Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplasty 2002 Oct: 17(7):876-81. 27. Augat P, Merk J, Genant HK, Claes L. Quantitative assessment of experimental fracture repair by peripheral computed tomography. Calcif Tissue Int 1997 Feb: 60(2):194-9. 28. Stephenson P, Seedhom BB. Cross-Sectional geometry of the human femur in the mid-third region. Proc Inst Mech Eng H 1999;213(2):159-66.