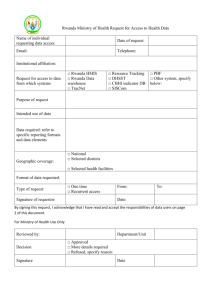
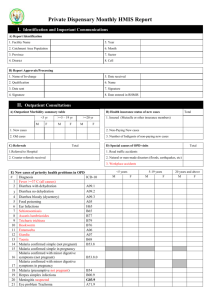
manual
advertisement

MINISTRY OF HEALTH HEALTH MANAGEMENT INFORMATION SYSTEM DATA MANAGEMENT, DEMAND AND USE TRAINER’S MANUAL APRIL 2012 Ministry of Health -Resource Centre April 2012 1 FORWARD National health programs and other partner institutions are working towards achieving goals as stipulated in the Health Sector Strategic and Investment Plan - Monitoring and Evaluation (HSSIP M&E) plan 2010/2011 – 2014/15. In that regard, the Ministry of Health recognizes the importance of using the National Health Management Information System (HMIS) for the successful planning, delivery and implementation of the minimum health services as indicated in the Health Sector Strategic & Investment Plan (HSSP). Both the HSSIP 2010/11- 2014/2015 and the National health policy have emphasized the use of information for decision making and monitoring and evaluating progress. To achieve this, the HMIS should not only be seen as a mechanism for collecting information and passing it to successively higher levels but Information should be used at the level at which it is collected for evidence-based decisions. In a bid to promote utilisation of the data generated from HMIS, Ministry of Health Resource Centre in close collaboration with MOH technical departments, donors and implementing partners has developed harmonized standard data demand and use tools for training in data management , analysis and interpretation and use at national, district and health facility levels. In designing the data demand and use manual, the Ministry is emphasising that, any data to be recorded at a service level must have a use (i.e ability to enforce action), efforts should be made to make better use of existing data at all levels through practical analysis and improved presentation of data and utilization. This is to be achieved by everyone remembering that HMIS is intended to provide information for action-it is like a bell that is intended to sound a warning to all data users of the result of the data. The HMIS provides strategic information for decision makers who may then combine this information with other strategic information from other agreed upon sources to make evidence-based decisions. The MOH warmly recommends its partners to use the HMIS data demand and use manuals as an important tool that will help promote the ongoing developments and Ministry of Health -Resource Centre April 2012 2 strengthening of the health management information system in Uganda.These tools should be utilized appropriately at the various levels of Health Care Service delivery to instil a culture of collection and utilization of quality data for evidence-based decision making. It is my appeal that the various health institutions and departments across the country use the standard and harmonized processes in this manual during the implementation to improve the Health Care Service delivery at all level in Uganda Please feel free to send feedback to improve this manual. The official email to which concerns can be addressed is hmisdatabank@yahoo.com. FOR GOD AND MY COUNTRY Dr. Aceng Jane Ruth Director General Health Services Ministry of Health -Resource Centre April 2012 3 ACKNOWLEDGEMENTS: The Data demand and use manual –have been developed by the Ministry of Health – Resource Centre in collaboration with the Ministry of Health technical programmes, districts, and various HMIS Implementing Partners. The MOH-Resource Centre is grateful to all stakeholders including local governments, organizations and individuals who have given assistance and supported the planning, development and finalization of the DDU Manual. The following individuals in particular contributed at different stages in the development of the Manual: Technical Team members who participated in the development of the Manual: Name Title/Organization Name Title/Organization Dr. Eddie Mukooyo Assistant Commissioner Resource Center Aguti Evelyn Francis Training officer/Coordinator – PREFA Mr Ally Kibwika Assistant Commissioner- Human Resource Development Lyazi Micheal Ivan M&E officer PREFA Ms. Caroline Kyozira Principal Biostatistician Mary Namuyomba Kayunga District HMIS –FP Natseri Nasan Data Manager/WHO John Kissa Statistician /RC Allan Nsubuga Statistician /RC Yawe Moses Nakaseke District Biostatistician Joel Kisubi Program management specialist USAID M&E Manager - STOP Malaria Dennis Businge M&E Director /STAR EC Kayanja Edward Luweero District HMIS-FP Areke James Stephen Soroti District Biostatistician Etoma Chalres Masindi District Biostatistician Kusiima Wilson Buliisa District HMIS FP Iteset Ruth Atiro Kaberamaido District HMIS FP Asiimwe Patricia Hoima District HMIS FP Bright Asiimwe Wandera Kayongo Emmanuel Flavia Kazibwe Andrew Anguko Dr. Ebony Quinto Dr. Suzie Nasar Project M&E officer STOP Malaria Project Data officer STOP Malaria Project M&E specialist – Malaria consortium M&E specialist- National Malaria Control Program Malaria Advisor PMI/CDC Ssetuba Abasolom Strategic information officer STAR – South West Angida Teddy Senior Statistician – Mulago National Referral Hospital Kasozi Sam HIS Analyst – CDC Opolot Francis Kumi District HMIS –FP Anna Collator Awor Statistician – CDC Thomas Emeetai Data Manager/STRIDES Dr Moses Walakira Director SI/STAR SW Nakamya Phellister M&E Specialist – UCCM secretariat Training Officer, PREFA Evelyn Aguti Frances Ministry of Health -Resource Centre April 2012 4 LIST OF ACRONYMS: DHMT: District Heath Management Team DHO : District Health Officer DHT: District Heath Team HCT: HIV Counselling and Testing HMIS: Health Management Information System HSD: Health Sub-District HSSIP: Health Sector Strategic and Investment Plan HSSP: Health Sector Strategic Plan HUMC: Health Unit management Committee IPD: In-Patient Department MDG: Millennium Development Goals MOH: Ministry Of Health OPD: Out-Patient Department UNMHCP: Uganda National Minimum Health Care Package VHT: Village Health Team WHO: World Health Organization Ministry of Health -Resource Centre April 2012 5 Table of Contents FORWARD.................................................................................................................................................... 2 ACKNOWLEDGEMENTS: ............................................................................................................................ 4 Table of Contents .......................................................................................................................................... 6 INTRODUCTION AND ORGANIZATION OF THE GUIDE ........................................................................ 9 GENERAL INTRODUCTION ......................................................................................................................... 9 PURPOSE OF THE MANUAL ..................................................................................................................... 10 HOW TO USE THIS MANUAL ................................................................................................................... 10 CONTENTS OF THE MANUAL .................................................................................................................. 11 OVERVIEW OF REQUIRED TRAININGS................................................................................................... 13 TRAINING MODAL /STRUCTURE: ............................................................................................................ 13 PERSONEL and REQUIRED TRAININGS: ................................................................................................... 13 Table of list of participants art various levels ......................................................................................... 15 OUTCOMES OF THE TRAINING ................................................................................................................ 15 INTRODUCTION TO THE WORKSHOP / TRAINNING .......................................................................... 17 SETTING THE STAGE: ............................................................................................................................... 17 MODULE 1: USING DATA TO INFORM POLICIES & PROGRAMS ....................................................... 19 MODULE 2: GENERATING/CREATING DEMAND FOR DATA. ............................................................ 20 Objectives ............................................................................................................................................... 20 DETERMINANTS OF DATA DEMAND: HEALTH FACILITY STAKEHOLDERS’ FORA .................................... 20 MODULE 3: HMIS DATA FLOW, DATA FORMATS AND ANALYSIS METHODS ............................... 23 3.1 DATA FLOW STRUCTURE WITH THE MOH HMIS: ............................................................................. 23 3.2 DATA FORMATS ................................................................................................................................ 24 CATEGORICAL DATA ........................................................................................................................ 24 NUMERICAL DATA............................................................................................................................ 25 3.3. FREQUENCY tables ................................................................................................................... 26 3.4 PERCENTAGES, PROPORTIONS, RATIOS, AND RATES .......................................................... 31 3.5 FIGURES............................................................................................................................................. 35 3.5.1. Bar graph ................................................................................................................................. 36 3.5.3. Histograms .............................................................................................................................. 37 3.5.4. Line Graph ............................................................................................................................... 38 CHECK LIST FOR PRESENTING DATA. ............................................................................................ 40 Ministry of Health -Resource Centre April 2012 6 SESSION 4: DATA MANAGEMENT AND ANALYSIS: ............................................................................. 42 4.1 DATA ANALYSIS FOR VOLUME OF SERVICES: ........................................................................ 42 4.3 DATA ANALYSIS FOR SERVICE UTILIZATION RATES: .......................................................................... 52 4.4 DATA ANALYSIS FOR MONITORING WORK PLAN: ............................................................................ 52 4.5 .Using HMIS data in Epidemic Detection ................................................................................ 53 4.5 Analysis checklist: ....................................................................................................................... 54 4.5 MAPS ................................................................................................................................................. 55 SESSION 5: DATA INTEPRETATION, SHARING INFORMATION AND PROVIDING FEEDBACK ....... 61 5.1 INTERPRETING DATA ......................................................................................................................... 61 5.2 DATA PRESENTATION, SHARING AND FEEDBACKS: .......................................................................... 63 5.3: LINKING DATA TO ACTION ............................................................................................................... 64 ANNEX 1: DATA MANGEMENT AND USE ACTIVITIES AT VAROUS LEVELS...................................... 69 ANNEX II: LIST OF INDICATORS RELATED TO HEALTH SERVICES PROVIDED AT FACILITY LEVEL AND HOW THEY CAN BE PRESENTED: .................................................................................................. 73 ANNEX III: INDICATORS WITH SOURCES OF DATA AT THE HEALTH FACILITY AND HOW THE INFORMATION CAN BE USED:................................................................................................................ 75 6.0. REFERENCES .................................................................................................................................. 95 Ministry of Health -Resource Centre April 2012 7 Ministry of Health -Resource Centre April 2012 8 INTRODUCTION AND ORGANIZATION OF THE GUIDE GENERAL INTRODUCTION Health management information is intended to incorporate all the data needed by policy makers, clinicians and health service users to improve and protect population health. As the HMIS in Uganda has been evolving, there has been a greater need for robust health information. The revised HMIS 2010 addressed most of the gaps which were identified by different stakeholders as the world community and all stakeholders have turned the attention to meeting Millennium Development Goal (MDG) targets, and ever increasing resources are going towards preventing and treating high burden diseases such as HIV and AIDS, Tuberculosis and Malaria. Decision-makers need to be able to measure whether policies and programs are working, and whether progress is being made towards the goals that have been set. Donors are also placing more emphasis on performance, linking the release of funds to performance-based measures. The World Health Organization (WHO) argues that investment in health management information systems (HMIS) now could reap multiple benefits, including: • helping decision makers to detect and control emerging and endemic health problems, monitor progress towards health goals, and promote equity; • empowering individuals and communities with timely and understandable healthrelated information, and driving improvements in quality of services; • strengthening the evidence base for effective health policies, permitting evaluation of scale-up efforts, and enabling innovation through research; • improving governance, mobilising new resources, and ensuring accountability in the way they are used. As more focus has been put on data availability , both health facility and district reporting have greatly improved over the past years, however ,reports from MOH Planning/resource centre supervisions show that the data collected by the health facilities using HMIS is not used locally. The strategy to address this gap was to develop this Data Demand and Use Training Manual which will be used to carry out training to all health workers to promote data demand and utilization at all levels and strengthening Ministry of Health -Resource Centre April 2012 9 data quality control systems. PURPOSE OF THE MANUAL This manual is to be used in all HMIS data management and use trainings aiming at standardizing the training given to all actors involved in planning, implementation and use of the HMIS data in Uganda. This manual provides facilitators in Data management and use with user-friendly, modifiable training components to adapt for different contexts at different levels of training. The modules can be presented as suggested, or separated to supplement existing material of a similar topic. Regardless, this guide will assist facilitators in ways to best incorporate data demand and use concepts into the various health workers trainings in the different diseases areas. The overall learning objectives of the training manual include: Improving the understanding of the role of data in decision making, the context of decision making, the determinants of data use, and the importance of data sharing and feedback at all levels . Building skills for applying data demand and using tools To build skills in data analysis and interpretation, data presentation, and data feedback; and To gain hands-on experience in linking data to the decision-making process at all levels HOW TO USE THIS MANUAL This training manual should be used as the main document for all the trainings organized by the various stakeholders/partners involved in the HMIS data training, data managements and use. A copy of the training manual should be given to all trainers / supervisors at all levels. This manual is for the trainers only. Health workers, Records assistants or officers participating in training sessions at district level do not need a copy of the manual. These may be given key message sheets or the health facility data management and manual for the users. Ministry of Health -Resource Centre April 2012 10 Basic assumption: For any Health worker to be trained in data demand and use, the staff has to be knowledgeable or was trained in the revised HMIS (2010) and also the HMIS reporting channel. It is also advisable that this training in Data use can be integrated in the HMIS Roll out training of the revised HMIS (2010) manuals. The staff trainees should know the Uganda National Minimum Health Care Package (UNMHCP) at their respective levels. Training should be held at government institutions and where possible, should be in a health facility that has been collecting HMIS data for the previous year. This will enable the participants to have a chance to use that same health facility data in the practical examples. National training of trainers will use examples of previous computerised data stored at MOH Resource Centre. The health facility training will be followed up by intensive, regular supervision at the facilities integrated into the health system support supervision visits. Since this manual will be beneficial only if all the trainers fully understand the HMIS forms which are the source documents for the data, trainers should have copies of HMIS tools and summary reports submitted to the district and National level for demonstration purposes. All references have been made to the HMIS forms in the HMIS health facility manual of 2010. A list of the training documents required include the following: a. HMIS health facility manual 2010 b. HMIS district manual 2010 c. MOH-Resource Centre Monitoring and Evaluation manual d. Standard Operating Procedures for health information e. HSSIP 2010/11 – 2014/15 (specific indicators packages pages 151-153). CONTENTS OF THE MANUAL This manual is composed of five sections: 1: Using data to inform policies & programs, 2. Generating/creating demand for data, Ministry of Health -Resource Centre April 2012 11 3. Understanding information flow, data formats and analysis methods, 4. Data management and analysis, 5. Data interpretation, action, sharing information and providing feedback Each section covers specific issues relating to the HMIS data. This arrangement facilitates the training activities to be presented in a more organized and logical flow. The trainers should ensure that they have previously read through this guide to acquaint themselves with the contents. Trainers should endeavour to follow the instructions provided for their use in italics and shaded in borders as highlights for training. Remember: It is critical that all trainers follow this guide closely when delivering the training. The content has been written carefully and builds on significant experience of HMIS Trainings by different stakeholders and has been approved by the MOH-RC. Good trainers are animated, keep their audience engaged, adopt participatory practical approaches in the training using available HMIS data, and follow the content of this guide closely. Ministry of Health -Resource Centre April 2012 12 OVERVIEW OF REQUIRED TRAININGS TRAINING MODAL /STRUCTURE: The CASCADE model training is to be used. Training and sensitization will be carried out at 3 levels with different objectives for each level (see below). The aim of these trainings is to ensure all involved understand the scope and importance of their data and use it in their day today activities for planning and decision making. The National level TOTs (trained for 2 days at the central level) will cascade the training to the districts level team. The district TOTs will then do the on job training at the health facilities. On average, districts with less than 30 facilities can have a maximum of four trainers. For the districts with more than 30 facilities, a ratio of five (5) health facilities to 1 trainer will be used to get the required number of trainers responsible or cascading the training to lower levels. The Districts Trainers will be selected /identified in consultation with Biostatistician and/or HMIS focal persons of the districts. Trainers will be selected based on training ability and skill, with Biostatistician, surveillance and HMIS focal person as essential trainers. These are to be trained for three days at the APPROPRIATE training centre, followed up by supervision during basic training by the Regional /National level master trainers when they are cascading the training to the health facilities. The whole DHT will be involved in the district training of trainers but only selected people will be picked out to cascade the training to lower levels. The team trained at the district will cascade the training to the health facilities as an on - job training. The participants for the activities from Central to health facility are defined (see below). PERSONEL and REQUIRED TRAININGS: The course should be delivered to teams from the health facilities or districts level. Each team should include both data users and data producers. Data users are health professionals- DHT members, Health Facility In charges, clinicians, midwives, nurses and other key health decision makers who use data to inform the health delivery system. Data producers are professionals who acquire and analyze health data and prepare them for distribution to audiences of users. These include Biostatisticians, malaria focal persons, HMIS focal persons, records assistant, record officers, data clerks, or researchers Ministry of Health -Resource Centre April 2012 13 (at times, this role is also carried out by a data user). The team approach has proven effective because it ensures that all of those involved understand their respective roles in data demand and use, and how the roles interact with each other. Understanding that team training may be cost prohibitive, the next best option is to provide separate training for data users and data producers from the same levels of the health systems. This type of training can be conducted as an add-on to previously scheduled meetings to minimize travel costs. If this option is selected, trainers should emphasize the links between data users and data producers and in cases where there is insufficient staff to cover the roles separately, modules should be adapted to ensure the producer/user understands both roles. To ensure ongoing functioning of health facilities alongside the training, the health workers from a particular health facility when the district TOTs are carrying out the on job training will be trained in two groups, one team for the first allocated days and the next team in the next allocated days. For example :-The training for a health centre II which lasts for one day will take two days to have all health workers at that facility trained , one team trained on Day 1 and the other on the Day 2. Ministry of Health -Resource Centre April 2012 14 Table of list of participants art various levels Training National / Regional Level Participants National trainers DHT trainers/supervisors The maximum number of participant per training is 40 Facilitators Resource centre and central level partners. District Level DHT , HSD Health InCharge Records people for hospitals and HSD. not to exceed 30 participants National trainers trained in the National TOT Health facility Level All health workers at the health facility. districts biostatistician, districts HMIS focal person or HSD HMIS focal person – sampled supervision by the National level master trainers Objective To equip the central trainers/supervisors with appropriate knowledge and skills to sensitize and train the DHTS in data demand and use and oversee /guide the implementation in the districts .To discuss the rollout of the training to the lower health units in the district and ongoing data ownership and utilisation at the point of collection.-(Duration 2 days) To equip the district trainers/supervisors with appropriate knowledge and skills to train and supervise the HSD, hospitals and lower health facilities in data management, demand and use. equipping the district , Hospital and HSD Health workers with skill of data use an analysis at their level. (Duration 3 days ) Equip the health workers with skill of data use at the health facility focusing on translating data into useful information. Duration 2-4days depending on the level of the health facility ) OUTCOMES OF THE TRAINING After completing of this course, participants at all levels are expected to be able to: • Understand the importance of using data locally • Analyze the volume and mix of services provided and identify seasonal changes in disease patterns • Graph key demographic characteristics of their catchment population; calculate targets for key health services as per HSSIP 2011/2015 • Use HMIS data to monitor the utilization coverage of key services • Use HMIS data to monitor stock out of essential drugs • Use HMIS and Community Mapping data to monitor the performance of health facility Ministry of Health -Resource Centre April 2012 15 ORIENTATION TO THE WORKSHOP: Check List during Training in Health Facilities Health Centre II (1 day) 1. 2. 3. 4. 5. 6. 7. Uses of data at Health Centre II data sharing meetings HMIS data flow frequency tables percentage ratio bar charts 8. pie charts 9. histograms 10. 11. 12. 13. 14. line graphs analysis of volume of service stock level epidemic data analysis for service utilization and coverage data interpretation and action Health Centre III (2 days ) 1. 2. 3. 4. 5. 6. 7. uses of data at health centre III data sharing meetings HMIS data flow frequency tables percentage ratio bar charts 8. pie charts 9. histograms 10. line graphs 11. using HMIS data to detect epidemics 12. analysis of volume of service 13. stock level 14. feedbacks and action 15. data analysis for service utilization and coverage 16. data analysis for service utilization coverage rates 17. data interpretation and action Ministry of Health -Resource Centre Health Centre IV/Hospital (4 days) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Uses of data all levels data sharing meetings HMIS data flow HMS data use barriers data formats frequency tables percentage ratios rates bar charts 11. pie charts 12. histograms 13. line graphs 14. scatter diagrams 15. map 16. data analysis for service utilization coverage 18. data analysis for service data analysis for service utilization and coverage 19. data analysis for service utilization coverage rates 20. Data interpretation Data use supervision 21. linking data to action 22. Providing Feedback April 2012 16 INTRODUCTION TO THE WORKSHOP / TRAINNING Members introduce themselves with a brief background of what they do and . how they use data Review of the participants expectations: Laying the ground rules Key highlight and facts on data use Sharing of the field experience from some participant in regards to data management and use .(each participants should give examples from their respective facilities) Ice breaker The trainer should put emphasis on working principles for HMIS data management and use. 1. 2. 3. 4. Any data to be recorded at a service level must have a use (action) Efforts should be made to make better use of existing data at all levels through practical analysis and improved presentation of data. Use of computerization should be encouraged and supported for database maintenance and report generation. Improvement in health data generation and use at the various service levels should be undertaken in support of efforts to improve service task performance and should be seen as a by-product of such performance improvement. SETTING THE STAGE: Highlight to note for facilitators: The collection and reporting of data through the HMIS is useful only if, at every level of the health system, the data is processed, presented and interpreted so that appropriate action can be taken to improve the functioning of the health system and the health status of the population. “Action” does not necessarily mean “change.” If after thorough analysis, one concludes that things are fine as they are, appropriate action is to ensure that things continue as they are. Most often, however, a good HMIS will pick up opportunities for improvement, even when things are going all right in general. Ministry of Health -Resource Centre April 2012 17 A routine system will use well-chosen indicators to warn unit heads, health facility Incharge, senior officers, DHT and district councils that certain aspects of the system need attention. Analysis of data is a continuum that starts with processing the data: Looking at the numbers, Re-organizing them, Re-grouping them, Doing calculations to get to ratios and rates, and calculating pre-defined indicators that reflect progress towards the health set out objectives and goals. Next, the data needs to be presented in ways that make it accessible for a large audience, often only interested in the main trends and findings. Interpretation of the processed and adequately presented data is best done by those that face the daily reality represented by the data. The distinction between data processing, presentation and interpretation is somewhat artificial, and often one goes through several iterations of the whole process or parts of it before feeling confident enough to decide on appropriate action. Ministry of Health -Resource Centre April 2012 18 MODULE 1: USING DATA TO INFORM POLICIES & PROGRAMS USES OF DATA TO THE HEALTH SYSTEM Each member should contribute and probably giving examples to their own health facility settings this can be an ice breaker. Group Activity 1: Divide the team in groups of at least 4 members. Give an Activity of needs assessment of the use of Health data at different health level and various stakeholders 1. Health unit level: Make discussion of what is the use of data, tailor the discussion to the specific levels 2. To identify disease patterns at your facility, in the community, district, etc and identify epidemics, outbreaks and notifiable diseases e.g. cholera, Ebola etc. 3. Helps the in charge of health units to plan for drugs needs , and drug supply chain management , lead time and time quantification of drugs 4. Plan for human resource management as per patient ratio 5. Leave schedules of the staff and daily rostra as per patients’ patterns are identified. 6. Timely essential drug stock outs and malaria endemicity patterns. 7. Provide timely immunization vaccine coverage, quantification , net distribution plans and all community intervention 8. Important source of information for the year work plans and budgeting purposes. 9. To assess whether the intervention had outcomes and assess impacts 10. Guide implementation of interventions such as malaria control intervention e.g. health education areas and community outreach plans Ministry of Health -Resource Centre April 2012 19 MODULE 2: GENERATING/CREATING DEMAND FOR DATA. Objectives 1. To understand the determinants of data use at all levels 2. Understand the barriers of data use at various levels. 3. To understand the importance of improving data-informed decision. 4. To shares ways of translating the data use knowledge into practise at various levels of data collection. Activity for National and District TOTS: Facilitators notes: the trainees have already highlighted the use of data in section one, the trainer should now understand why then is the data not used even after the trainees being able to understand that this data is useful. (i.e. putting knowledge into practice). The aim of the activity is for the National/ District TOTs to understand the way for creating demand for data and barriers of data use at various levels of the health systems and ways of approaching these barriers such that when they are cascading the training they can share the problems and practical solutions to the various levels within their districts. GROUP ACTIVITY 1: Divide the team in groups of 4 to maximum of 8 members: 1. Each group gives 3-5 ways or strategies which can be used to create demand for data at various levels. (5-10minutes) 2. In these same groups members should give reasons why this is currently not happening? (why is HMIS data no used at the point of collection, what are the barriers for data use (510minutes) 3. What are the visible solution to these barriers: After each exercise an interval is given for at least a group to present to all members. Alternatively all the exercise can be done at once and presentations done at the end. DETERMINANTS OF DATA DEMAND: HEALTH FACILITY STAKEHOLDERS’ FORA The following key activities can drive data demand at the health facility: Ministry of Health -Resource Centre April 2012 20 Facilitators notes: This is additional information to the discussion of the trainees in the above exercise as per health guidelines DHO / Health facility In Charges are responsible for verification and analysis of administrative and service delivery reports. The generated reports from the HMIS data are to be used for health facility performance review and improvement, planning, and resource mobilization. The Health Information Assistant / Records assistant or designated person is responsible for submission of the health facility reports to the HSD and DHO. Each report should be received at the HSD office by the date due. During the monthly health facility meetings, performance review should focus on the information from the data generated from the health units, sub districts and districts so that actions are evidence based. The health facility quarterly assessment reports will be used for performance review during the quarterly HUMC meetings, whereas the annual district /sub district performance report will be presented and discussed during the annual district / Sub County stakeholders’ forum. During this meeting the forum should also focus on looking at what the data is saying as per the services provided and how they are utilised – the performance review should look at things like immunization coverage- why are mothers not bringing the children for immunization (for example if immunisation is low), do the mother attend ANC, how is the IPT2 uptake , what is the leading cause of deaths in our community , what can we do to prevent the diarrhoea outbreak seen as per the health data from the health facility, etc? Issues of timeliness, completeness and accuracy of the reports can also be mentioned when discussing the session of HMIS. There are potential disastrous consequences if data is missing, poor quality or lately reported. Imagine inaccurate stock reports have led to under quantification at district/national level, late reports can lead to un noticed disease out breaks leading to loss of many lives. Ministry of Health -Resource Centre April 2012 21 Each health facility in the country has a defined catchment area, for which it is responsible for coordinating delivery of services to implement the HSSIP. Stakeholders from the community up to politicians need and should have access to data on which to base decisions and advise given to the community during their community engagement platforms on issues like: (a) Prioritization of household income (e.g. should I buy a mosquito net or use the money for something else, what is mobile phone ownership more that availability of a latrine at the household) (b) Budgeting for programs at the sub-County, Town Council, district and National level. If the data is not available, analyzed, interpretable and shared with the relevant parties, wrong decisions can be made with possibly dangerous consequences. All stakeholders in the catchment area of the facility can come together to discuss health and health related issues affecting them quarterly each year. In these meetings, data should be shared. Group activity 2: What is the immediate action within your reach which can be done to improve/promote data use at your level. Ministry of Health -Resource Centre April 2012 22 MODULE 3: HMIS DATA FLOW, DATA FORMATS AND ANALYSIS METHODS Objectives: At the end of this session the learners should be able to: 1. Describe data on terms of frequencies distribution, percentages and proportions 2. Use figures to present data 3. Calculate the frequencies, percentages, proportions, ratios, rates for the major variables in the top ten diseases. 3.1 DATA FLOW STRUCTURE WITH THE MOH HMIS: The HMIS involves the following processes: collection of data, processing it for conversion into useful information, analyzing and discussing it assess the current status of services and using it to set appropriate strategies and targets for improvement. The flowchart in Figure 1 shows the different steps in data collection and transmission, as well as analysis and feedback. At the level of Health center, health workers keep a record of activities and patients seen on the provided HMIS forms in all different area( i.e OPD, ANC, pharmacy, etc) , the records officers/assistant or health in-charge for Health centre II collects monthly summary reports. This data is submits to the HSD and the HSD submits the aggregated data for all its health facilities to the districts. The district aggregates all the data from all the HSD and submits to the National level. These reporting structures are well laid out in the HMIS health facility manual (2). Ministry of Health -Resource Centre April 2012 23 Village Health Teams (VHT) 3.2 DATA FORMATS In analysing our data, it is important to determine the type of data that we are dealing with. This is crucial because the type of data used largely determines the type of techniques that should be used to put this information into use Some of the variables may have produced numerical data, while other variables produced categorical data. CATEGORICAL DATA There are two types of categorical data: they are nominal or ordinal Example NOMINAL DATA CATEGORIES SEX Male , female Tested Taken to the lab, not taken to the lab ORDINAL DATA CATEGORIES Ministry of Health -Resource Centre April 2012 24 Anemia Severe, moderate ,mild age group Under 5, above 5 Level of knowledge Good , average , poor NUMERICAL DATA When do we talk of Numerical data? We speak of NUMERICAL DATA if data is expressed in numbers. There are two types of numerical data: Discrete or Continuous. How do I differentiate discrete data from continuous data? DISCRETE DATA are a distinct series of numbers. For example: DISCRETE DATA VALUES Number of malaria cases per day 0, 1, 2, 6, 19, etc. Number of clinic visits 2, 4, 10, 0, 3, etc. Number of pregnancies per woman 2, 3, 5, 0, 5, 4, etc. Number of new attendants per day 40, 45, 100 etc CONTINUOUS DATA come from variables that can be measured with greater precision, depending on the accuracy of the measuring instrument, and each value can increase or decrease without limit. For example: a) Height (to 2 decimal point) b) Temperature (in degree Celsius, OPD register specifically for malaria patients, patient Form 5) c) Children’s weight ( in the immunization register) VALUES a) 12.12, 9.95, 45.13, 6.99, 28.78, etc, b) 37.5, 37.8, 39.2, 40.1, 36.9, etc, Ministry of Health -Resource Centre April 2012 25 HOW CAN WE PRESENT DATA? Data can be presented as: • Frequency distributions • Percentages, proportions, ratios and rates • Figures. • Measures of central tendency 3.3. FREQUENCY tables Example 3.3.1: categorical data frequency distribution To identify the number of females and males patients attending the out patient clinic at Kasaana H.C IV for the month of December 2010.The results are presented in the following frequency distribution: Sex Frequencies Male 200 Female 300 Total 500 A frequency distribution is calculated by simply totalling the number of responses in each category, that is tallying from the OPD register all the male patients. This summary is also on HMIS form 105. You should always check that the total number of responses agrees or tallies with the number of subjects (respondents). Category for missing sex are not allowed in the HMIS and should be noted as a data quality check. For example if the total number of patients seen in December was 505, one will expected that the total of females and males should be 505. 3.3.2. Exercise for the Health facility trainees: To identify what family planning methods were used by mothers in Kiryandongo hospital, Mothers were asked what family planning method they were using. The results from the Maternal health register are presented in the below: Ministry of Health -Resource Centre April 2012 26 Method Number Abstinence 16 Condoms 47 Injectables 1 Norplant 1 Pill 35 None 300 Total 400 What can you conclude from the data? High light discussion answers to exercise 3.1: By looking at the frequency distribution above you can conclude that 75% or three out of four of the mothers are not using family planning. For those who are using family planning methods, Condoms and pills are the most commonly used methods with 47% and 35% respectively. Category Number Using FP Method 100(25%) Not using any method Number 300(75%) Total 400 FP method Number Abstinence 16 Condoms 47 Injectables 1 Norplant 1 Pill 35 Total 100 Ministry of Health -Resource Centre April 2012 27 Example/ exercise 3.3.3: Health in charge from 148 different public health facilities were asked the following question during the National support supervision visit to the districts .How often have you run out of medicines for the treatment of malaria in the past 6months? This was a closed question with the following possible answers: never, 1 to 2 times a month (rarely), 3 to 5 times a month (occasionally), more than 5 times a month (frequently). The number of responses in each category was totalled to give the following frequency distribution: Categories Number of Health facilities Never 47 Rarely 71 Occasionally 24 Frequently 6 Total 148 In this example, the data are ORDINAL. The ordering of the categories is important as eachcategory from top to bottom indicates increasing severity of the problem. The frequency distribution results indicate that most health facilities rarely experience shortages of Anti-malarial drugs, but that it is an occasional problem in about one sixth of the health facilities and a severe problem in a few. B. Numerical data frequency distribution Procedures for making frequency distributions of numerical data are very similar to those for categorical data, except that now the data have to be grouped in categories. The steps involved n making a frequency distribution are as follows: Ministry of Health -Resource Centre April 2012 28 1. Select groups for grouping the data. 2. Count the number of measurements in each group. 3. Add up and check the results. When grouping data, the way the groups are selected can affect what the results are going to look like. There is little substitute for common sense here, but it may be necessary to change the grouping if you suspect the information is being hidden by a poor selection of the groups. Example 3.3.2 Seven Health centres of Bukedea district are submitting numbers of malaria cases per week using the HMIS 033b and the HMIS focal person is to summarise the data. Compare the health facility and district weekly summaries of the same data as presented in Table below. H.F. 1 9 cases H.F. 2 12 H.F. 3 11 H.F. 4 13 H.F. 5 14 H.F. 6 13 H.F. 7 16 H.F. 1 16 cases H.F. 2 16 H.F. 3 18 H.F. 4 19 H.F. 5 16 H.F. 6 21 H.F. 7 25 District weekly summary: Week 1 88 cases Week 2 131 cases Ministry of Health -Resource Centre April 2012 29 H.F. 1 28 cases H.F. 2 28 H.F. 3 28 H.F. 4 32 H.F. 5 21 H.F. 6 19 H.F. 7 12 Week 3 168 cases All Health Facilities data show an increasing amount of malaria cases, but the improving situation showed in health facility 6 and 7 in the third week cannot be reflected in the weekly summary for the district. It would therefore be better to use the health facility data if you want to indicate when and where exactly the numbers of reported malaria cases started going down/up and which health facility is contributing a bigger problem. GROUPING NUMERICALDATA: How do we group numerical data? When grouping data the following rules are important: - The groups must not overlap, otherwise there is confusion concerning in which group a measurement belongs. - There must be continuity from one group to the next, which means that there must be no gaps. Otherwise some measurements may not fit in a group. - The groups must range from the lowest measurement to the highest measurement so that all of the measurements have a group to which they can be assigned. - The groups should normally be of an equal width, so that the counts in different Ministry of Health -Resource Centre April 2012 30 groups can easily be compared. Sometimes, however, it is valid to choose groups that are of different widths, for example if you are interested in specific age groups relating to HIV treatment (e.g., less than 1 year, 1 to 4 years, 5 to 14 years). The advantage we have is that the new HMIS has standardised the categorised as per need for comparability across health units and districts. When you start summarising data it is better to make too many groups than too few. This is because during data analysis you can combine groups to form new categories without having to go through all your data again, whereas if you have too few groups you have to go back to your raw data to make more groups. A larger number of groups will generally give a more precise picture, but when using too many groups one can lose the overview. As a general rule choose round numbers for the lower values of the group limits. For example: 1.00-9.99, 10.00-19.99, 20.00-29.99, or: 0-4; 5-9, 10-14, etc. 3.4 PERCENTAGES, PROPORTIONS, RATIOS, AND RATES 3.4.1. PERCENTAGE Instead of presenting data in frequency tables using absolute numbers it is often better to calculate percentages. Percentages standardise the data, which means that they make it easier to compare them with similar data obtained from another health facility or district. Example 3.4.1 82 health facilities in Wakiso district are supposed to submit the number of patients treated for malaria per month. (HMIS 105 – row 27, summary on HMIS 123 for the district). Data for September 2011 submitted Ministry of Health -Resource Centre to the district was summarised. TheHMIS April 2012 31 focal person presented both the frequency distribution and percentages (or relative frequencies): Table3.4.1: Distribution of health facility according to number of patients treated for malaria in one month Number of patients Number of clinicsa Percentage 0 to 19 25 31% 20 to 39 3 4% 40 to 59 5 6% 60 to 79 11 14% 80 to 99 19 24% 100 to 119 10 12% 120 to 139 4 5% 140 to 159 3 4% Total 80 100% a Data from two health facilities is missing – no reports received. Note: Usually you do not include missing data in the calculation of percentages. The frequency of responses in each group is calculated as the percentage of those study elements for which you obtained data However, the number of missing data (e.g., heath units which never reported or wards whose data was not received) is a useful indication of the adequacy of your data collection. Therefore this number should be mentioned, for example as a note to your table. As footnote on the above table indicate that 2 health units never submitted reports. Facilitators NOTE: Points to note: Point 1: The percentage of the cases Ministry of Health -Resource Centre April 2012 32 Is a more processed piece of information and better expresses the contribution of the cases of interest in a denominator. Enables comparison of the data of one health facility with those of another. Example of comparison of the data between two health facilities. For example, if a Health facility has reported 10 cases of pneumonia and another health facility has reported 30 cases, one may conclude that the second health facility has seen more cases. But, if the first has seen 400 patients and the second clinic has seen 1200 patients during the same period, the calculation of the percentage of pneumonia cases shows that the percentage of pneumonia cases in Both health facilities is the same (i.e., 2.5%).The formula for calculating the percentage of the cases is: Percentage of the case = Total number of the case x 100 / Total number of patients Point 2: Caution on interpreting percentages if the total number is small!! One should be cautious when calculating and interpreting percentages if the total number is small, because, one unit more or less would make a big difference in terms of percentages. As a general rule, percentages should not be used when the total is less than 30. Therefore it is recommended that the number of observations or total cases studied should always be given together with the percentage. Example: The Laboratory personnel in Kibaale H.C IV went for leave in the month of July 2011, the total number of blood slides examined for malaria in this Health facility for this month was recorded as 20. The positive slides were 10 which correspond to 50%. If the positive had been found to be 11 instead of the 10 due to a mistake in counting, then the relative frequency would have been 55% which already makes a difference of 5%. However if the total number of slides examined had been 200, out of which 100 are positive, (50%), then one slide more or less i.e. (101 0r 99) would not have made a such a Ministry of Health -Resource Centre April 2012 33 big difference in terms of percentages Examples of percentages which can be computed from the HMIS Number of under malaria cases as a percentage of total malaria cases Number of lab test as percentage of total suspected malaria cases Number of malaria positives as percentage of all malaria tests done Number of IPT2 as a percentage of new ANC attendance Number of specific family planning methods as percentage of all FP patients seen. Number of pregnant women tested positive for HIV as percentage of all pregnant women tested for HIV. 3.4.2. PROPORTIONS What is a proportion? A PROPORTION is a numerical expression that compares one part of the study units to the whole; a proportion can be expressed as a FRACTION or in DECIMALS. 3.4.2.1: Example of proportion Out of a total of 55 patients diagnosed with malaria in the OPD at Kyamulibwa H.C.II on a specific day , 22 are adults and 33 are children less than 5 years . We may say that the proportion of children among the malaria cases is 33/55 or 3/5, which is equivalent to 0.60. Note that when a proportion expressed in decimals is multiplied by 100, the value obtained is percentage. In the example, 0.60 is equivalent to 60%. 3.4.3. RATIOS What is a ratio? A RATIO is a numerical expression that indicates the relationship in quantity, amount or size between two or more parts. In Example 5 above the ratio of adults with malaria to children with malaria is 22:33, or 2:3 Ministry of Health -Resource Centre April 2012 34 3.4.4 RATE What is a rate? A RATE is the quantity, amount or degree of a disease or event measured over a specified period of time Facilitators note: Mention this for knowledge in health facility II and III training. To be emphasised/detailed for the district TOTs (Biostatistician HMIS focal person, Hospital and H.C IV) Commonly used rates in the health sector are: Birth Rate The number of live births per 1000 population over a period of one year Death Rate The number of deaths per 1000 population over a period of one year Infant Mortality Rate The number of deaths of infants under one year (IMR) deaths of age per 1000 live births over a period of one year Maternal Mortality Rate The number of maternal pregnancy-related in one (MMR) year per 100,000 total births in the same year Incidence Rate The number of new cases per population over a specific period of time (usually a year) Prevalence Rate The number of existing cases per population over a specific period of time (usually a year) 3.5 FIGURES. From The HMI S many descriptive tables can be generated. It may gain readability if this most important data is presented in figures .The most frequently used figures for presenting data includes • Bar charts • Pie charts For categorical data • Histograms • Line graphs for numerical data • Scatter diagrams • Maps Ministry of Health -Resource Centre April 2012 35 3.5.1. Bar graph Bar charts are a way of presenting a set of numbers by the length of a bar; they are used to make comparisons among individual items. They enable the observer to compare the values visually. The bars are not joined together, but separated by a space. This diagrammatic arrangement is used when an axis deals with information that is qualitative or non-continuous in nature, such as different diseases, different facilities, etc.... The categories being compared are conventionally drawn vertically (column charts), but can be presented horizontally as well. We can draw simple or multiple bar charts. In the latter, more than one variable is displayed. Facilitators guide: Read through example 2 for the trainees: put it up on a flip chart or project it. We will now look at examples of the above mentioned figures that can be used for presenting data: The data from example/exercise 4.2.3 can be presented in a bar chart, using either absolute frequencies or relative frequencies or for percentages. FIGURE 3.5.1: BAR GRAPGH SHOWING FREQUENCY OF SHORTAGE OF ANTIMALARIA DRUGS IN 148 HEALTH FACILITIES SUPERVISED IN THE LAST QUARTER. Number of Health facilities 80 70 60 50 40 30 20 10 0 Never Rarely Occasionally Frequently Ministry of Health -Resource Centre April 2012 36 FIGURE 2 SHOWS A BAR CHART COMPARING THE TOTAL NUMBER OF DELIVERIES, THE NUMBER OF DELIVERIES WITH COMPLICATIONS AND THE NUMBER OF DELIVERIES REFERRED, IN DIFFERENT H.C IV OF WAKISO DISTRICT 90 80 70 Number 60 50 40 30 20 10 0 NAMAYUMBA H.C.IV Total deliveries WAKISO H.C.IV KASANGATI H.C.IV Number of deliveries with complications NDEJJE H.C.IV BUWAMBO H.C.IV Number of deliveries referred One can also compare the same category in different places or points in time. 3.5.2. Pie charts When do we use pie charts? A pie chart can be used for the same set of data, providing the reader with a quick overview of the data presented in a different form.Pie charts can be used to show the mix of family planning services provided, the mix of diseases diagnosed, the mix of different ARI cases, of different Malaria laboratory diagnoses, etc. A pie chart illustrates the relative frequency of a number of items. All the segments of the pie chart should add up to 100%, so that sphere represents 100%, a hemisphere 50% (half of the pie) and a quarter 25% and so on 3.5.3. Histograms Numerical data are often presented in histograms, which are very similar to the bar charts which are used for categorical data. An important difference however is that in a Ministry of Health -Resource Centre April 2012 37 histogram the ‘bars’ are connected (as long as there is no gap between the data), whereas in a bar chart the bars are not connected, as the different categories are distinct entitles. The data of 3.5.4. Line Graph What is a line Graph? Line Graph is used to show the trend of an indicator (e.g. # people served, number of under five malaria cases etc) over time. How do I draw a line Graph? FACILITATORS GUIDE: Go through the following steps with a job aide for health centre II and III, for the H.C IV and hospital this is directed using excel package on the computer. The assumption is all national trainer should be technical lead in drawing basic graphs using excel. Steps for H.C II and III training: (Grid Job aide provided) Step 1. Using the line chart template below, label the small boxes below the horizontal line (called horizontal axis) to correspond to the months of data that your graph will represent. In this template, the graph can cover a period of 18 months. Step 2. Now you need to scale the left vertical line (called vertical axis) appropriately and label the marks on it. Depending on the expected values of your indicator, you need to determine a maximum to mark the highest limit of your vertical axis. For example, if you want to plot the trend of OPD patients served in your HF and during the past six month, if the maximum monthly value has been 600, choose 720 (i.e. 600 + 20%*600) as the maximum value on the vertical axis. Then, label the vertical axis marks to start at 0 and finish at the maximum (720 in our example). Note: if the monthly variation of the indicator is expected to be low, instead of starting at 0, you can start at a higher value, but you need to keep this point in mind at the time of Ministry of Health -Resource Centre April 2012 38 interpretation. Step 3. Plot the value of your indicator from each month (from the sources that you’ve already identified, for example total OPD patients (i.e. new attendance and re-attendance as per the OPD register summarised on the HIMS 105) on the chart. For each month, put a dot on the graph to show the value of the indicator (total OPD patients served) for each month. Step 4.Connect all the dots that you have plotted on the graph. This line will show the trend of your selected indicator over the past few months. For the next month(s), you only need to make a new dot showing the new value of your indicator and connect the dot to the previous month. Continue to do the same for each month to monitor the future trend of the indicator and to see whether your interventions have been effective in changing the trend. Facilitators’ Notes: need to mention that: You can plot two related indicators in one chart and have two different trend lines in one graph. For instance, you can plot the # OPD cases and<5 cases on the same graph. Plotting more than one trend on one graph (if selected appropriately) can give you additional insight that can facilitate the interpretation of data. Ministry of Health -Resource Centre April 2012 39 Exercise: Draw a line graph to present the data below: Facilitators: The trainer should be aware that the time is the X axis and DPT3, or DPT3 targets or DPT 3 cumulative is the Y-axis. The graph have more than one line plotted on a single graph be only month. month Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec target DPT 3 # of 80% cumulative DPT3 501 401 401 1002 921 520 1503 1236 315 2004 1651 415 2505 2165 514 3006 2767 602 3507 3177 410 4008 3687 510 4509 4194 507 5010 4506 312 5511 4962 456 6012 5266 304 CHECK LIST FOR PRESENTING DATA. When using any of the above mentioned tools to present data, check for the following: 1. Do I have a title? The data presented should have a title. The title must be brief and self-explanatory, expressing all the information that is being presented. The meaning of the title should be immediately obvious to readers, without having to refer to a text for an explanation 2. The headings of columns or rows in tables should be clear and concise. 3. Axes of graphs and diagrams should be properly defined and clearly labeled with their scales. The vertical axis of a graph is known as the Y-axis, or the ordinate, while the horizontal axis is known as the X-axis, or the abscissa. Ministry of Health -Resource Centre April 2012 40 4. Keys or labels are necessary in graphs with more than one line or bar, i.e., when information on more than one case is presented. The labels identify the different groups being presented for comparison. 5. Footnotes may be given, where necessary, providing explanatory notes or additional information. 6. Keep it simple: no graph should attempt to present so much information that is difficult to comprehend. 7. The data must be presented according to size or importance, chronologically or geographically. 8. When the tables and charts are prepared, the head of the health facility or in-charge of OPD should do the checking and the interpretation, as elaborated in the next chapter. The report, tables and charts should be put on the notice board of the health facility. The tables and charts that monitor progress for the whole year should be updated every month and kept on the notice board. 9. Each months / quarter’s tables and charts should be replaced the following month/quarter and permanently kept in a file if the notice board cannot have all of them at ago. The notice board should have the most up-to date information for appropriate planning and decision-making. Ministry of Health -Resource Centre April 2012 41 SESSION 4: DATA MANAGEMENT AND ANALYSIS: Now that we have seen the methods of data analysis, which can be applied to the HMIS, let us now focus on how we will analyse the data which later link to interpretation of the findings: Service Delivery Data Management activities at each level are contained in Annex I: Needs for this session: • One field in HMIS form filled out • Catchment area population • Map of the district/ sub county / Catchment area map for the Health facility • List of villages for H.C II list of parishes for H.C III, lit of sub counties for H.C IV/HSD , and in case of district Tots, list of HSD). • Paper, ruler, pen and calculator for H.C.II & III training, computes for other levels Data for the HMIS 105 for the previous six months. 4.1 DATA ANALYSIS FOR VOLUME OF SERVICES: Source: HMIS form and registers; required for this exercise: the health facility monthly inpatients data of the last three months, the health facility outpatient data of the three six months (HMIS 105 and HMIS 108) Indictors: patient load (health facilities & health posts/out reaches), mix of services, major patients groups; top ten diseases Tabulation/presentation of data: line chart (trend analysis), pie chart Analysis purpose: monitoring improvement and seasonal changes Objective Ministry of Health -Resource Centre April 2012 42 - understand the meaning of performance indicators and select from a list those basic indicators that are key to monitor delivery of Basic package of health care service at the various levels - be able to describe the use of line, bar and pie charts - use line, bar and pie chart to monitor the basic performance indicators of a health facility / district (service delivery) Facilitator’s guide: Ask the participants the following question one at a time and go through, make sure you note their answers on the chart, write the indicators on the charts or Project the slide. Remember this is discussion session read out the answers written in the table i.e. how the data can be used as addition suggestion but probe for the health workers own thinking and initiatives’ on data use. Discussion questions Which of the following indicators do you think are most useful in monitoring the performance of your health facility? What other indicators (not listed here) do you think would be key in measuring your health facility performance? Relate this to the use of data to the health system in Module 1: List these indicators electively for applicability in trainings of HC II & H.C III trainees List all indicators if the training is for levels above H.C III. Examples used will focus on these indicators. More indicators in Annex III. Indicator/variable Source of data # of OPD served OPD registers / # of children less than 5 years summarised on served in the OPD HMIS 105 Ministry of Health -Resource Centre How can the data be used All levels: Show utilisation of the health centre in general. Identify trends; causes for the current trends; identify the need for change; design interventions for change. April 2012 43 Indicator/variable Source of data top ten diseases in the OPD HMIS 105, OPD register # of New ANC & 4th visits HMIS 105, ANC register How can the data be used Hospitals For the hospital OPD new attendance should be less than 10% of all attendances, as this level is referrals. OPD Morbidity, as the In-charge , there is need Identify top ten most prevalent diseases treated; plan for the necessary stock of key pharmaceuticals; design preventive interventions and communicate to the staff team how to approach the situation , reference the MOH guidelines necessary etc. Use of ANC, focus on MCH as per Reproductive health Division strategic plan Access to malaria preventive measures Immunisation coverage Number of LLINs given at HMIS 105, ANC ANC register # of children immunised for HMIS 105, DPT1, 3 and measles immunisation tally sheet, child register # new acceptors of family HMIS 105, Family Family planning coverage, strategies planning methods Planning register for improvements Method mix among new HMIS 105, Family Adaptive methods , stock refills acceptors Planning register Number of malaria test done # deliveries carried out at the health facility # lab confirmed TB cases who started treatment # of HIV tests done HMIS 105, Lab register HMIS 055A HMIS 105, maternity register Rates of presumptive treatments, laboratory utilisation and training needs in laboratory Need to identify the current trend in H.F deliveries and whether the trend should change; design interventions for change; monitor effectiveness of the interventions HMIS 106a, TB Access to TB care, diagnosis register HMIS 105, HCT Access to HIV care, laboratory register HMIS- utilisation and training needs in 055b laboratory Ministry of Health -Resource Centre April 2012 44 Indicator/variable Number of families visited by Health assistant or number of community out reaches done Source of data How can the data be used Health assistant activity reports., HMIS 105 Quick example: HMIS form 123 reported for the month of July2009 show data as below District Suspected Malaria cases Under five Soroti 3042 2452 Amuria 1045 982 Kaberamaido 800 685 Kumi 2096 1045 Present this data on a graph Group work: Put the class into groups and have the list of the HMIS forms data for the previous 6 months. If there is more than one person from a particular health facility, and the Health facilities are not more than 10, each health facility would work on their set of indicators and present it out to the class. Exercises Note: For doing these exercises you will need to have the HMIS105 and/or HMIS 108 of your health facility for the last six months. For the district, they require HMIS 123 and 124 for the last six months Use the provided templates and grids for constructing line, pie and bar charts to present the appropriate indicators if the trainees do not have computers (specifically for training at HC II & III Note to the facilitator move around to the team and ensure groups pick the appropriate presentation i.e. type of graph for the indicators. Since the indicators are many, you can Ministry of Health -Resource Centre April 2012 45 opt for each group to present work on other indicators. However ensure that at least two groups are working on the same set of indicators to compare the reasoning for under performance. For the HSD/Hospital they opt to use computers so it will not take a lot of time. 1- Using a chart, plot the trend of OPD patients served in your health facility over the past six month. In the same chart plot the trend of under five OPD patients served during the same period. The group should pick the appropriate chart, Facilitators note: Bar and line graph are the most appropriate to present the two indicators on one chart. (Probing questions) How do these trends look like? Decreasing, increasing, constant or fluctuating? Do you think this trend is acceptable or you need to do something to change it? What are the most likely causes of the current trend? If you need to change the trend, what interventions should be adopted? Which one of these interventions is within your control at the health facility level? How are you going to share this information with your staff? Which one of them is beyond your control at the health facility level and what needs to be done so that you can get the necessary support? 2- Repeat the above exercise for the new acceptors of family planning services. Using a pie chart, indicate the share of each family planning method among the new acceptors. (Probing questions) Which method is most commonly used? Which method is used the least? Which method is used less than you expected? Which method is used more than expected? Ministry of Health -Resource Centre April 2012 46 What is the most likely underlying cause for these conditions? Do you think you need to bring any changes to the share of any of the methods? If you need to change this pattern, what interventions should be adopted? Which one of these interventions is within your control at the health facility level? How are you going to share this information with your staff? Which one of them is beyond your control at the health facility level and what needs to be done so that you can get the necessary support? 4.2 DATA ANALYSIS FOR SERVICE UTILIZATION COVERAGE: - Use demographic and target group data, HMIS and baseline household survey data to monitor the utilization coverage for EPI, antenatal care, deliveries by skilled personnel and family planning services - Be able to identify trends and needs for change in the current status and analyze most likely causes - Design interventions to make changes happen Discussion questions The below charts demonstrate the performance of a health facility on DPT3 vaccination in its catchment areas. - On which HMIS form and where exactly can you collect the number of DPT3 doses administered to under 1 children? - In the first chart, explain what does each of the following mean? • The vertical axis and its values • the bar graph • the line graph • How do you think the line and bar graph are related? Ministry of Health -Resource Centre April 2012 47 Example 4.2.3: Use the data below to create a line graph of monthly DPT3 coverage and targets for Nakasongola district. # of # of # of month DPT3 month DPT3 month DPT3 Jan 401 May 514 Sep 507 Feb 520 Jun 602 Oct 312 Mar 315 Jul 410 Nov 456 Apr 415 Aug 510 Dec 304 Total number of children under 1 year of age: 7512 National DPT3 coverage target: 80%. 1. Use the national DPT3 coverage target, or the specific target for your facility if you have it. We assume the target is to completely immunize 80% of children under one year of age (or 80 children out of every 100 children). 2. Get your facility’s data. You need a denominator. In the case of DPT3 immunization, this will be the number of children under one year of age in your catchment area. There are several ways to obtain this denominator. For our example, If Nakasongola district the <1 population in 2012= 7512children. 3. Convert/calculate the local annual target for your facility as follows: Ministry of Health -Resource Centre April 2012 48 Number of children <1 multiplied by target = your facility’s annual target, using a target of 80%: (7512 X 80/100) = 6010 children to be vaccinated in a year (i.e. the health facility target 4. Calculate the local monthly target for your facility, using the annual target, as follows: Local ANNUAL target divided by / 12 months = your HMIS MONTHLY target. 6010 divided by 12 = approximately 501 children per month, to be vaccinated for DPT3. 5. Draw the X and Y-axis (see line graph example):X-axis = 12 months, labeled “Jan to Dec“(Bottom, horizontal line of graph). Y-axis = labeled Children Immunized (Left hand side, vertical line). 6. Place total number of children <1 (7512) at the top of the Y axis and complete the scale down to zero (the corner of the graph). 7. Mark the point for your annual local target (6010) up on the graph above the month of December. This is the number of children that you plan to have immunized with DPT3 by the end of the year. 8. Trace a broken line from 0 children at the beginning point in January, through to your local target point marked at the end of the year (December). This is your “Target Line”, which you need to achieve in order to reach your target. 9. In your frequency table in the left upper corner, ADD the number of newly immunized Children of each month to the previous month’s total number. The number of children vaccinated each month is taken from the HMIS 105, Section “child immunization”, which Ministry of Health -Resource Centre April 2012 49 is the total number of children 0 – 11 months vaccinated with DPT3. Adding the number to the previous month’s number gives you the “cumulative” total. 10. Plot the graph accordingly, labeling dots with the cumulative number of new + old children immunized. Connect the dots with an un-broken line. Starting from the end of January, plot the ACTUAL number of children immunized. Make the dot and label that point with the actual number of children immunized. 11. Each month monitor your facility’s performance against the target. If the target is NOT being met, decide on immediate actions to be taken by nurse in charge of immunization of health assistant staff. 12. Finally, put a Title on your graph that explains what the graph is showing (example: DPT3 Target Monitoring, Nakasongola district, 2011). Also include the Source: of the data (which HMIS form or register), the Author (s): and the Date the data was compiled. Computerised excel system for district, H.C IV and Hospital: Using excel after you have entered the data, click on insert tab on excel menu, click the line graph under the chart tab, click the line graph type of your choice, you can adjust insert titles, adjust the legend according) Facilitators note: Demonstrate this on the computer as appropriate for the trainees to get this done with a computer. DPT 3 immunisation coverage for Nakasonogla district: 2011: Ministry of Health -Resource Centre April 2012 50 DPT3 Immunization Coverage Nakasongola distrcit,2011 Population <1 7512 National DPT3 Target 80% Annual Local DPT3 Target 6010 Monthly Local Target 501 month target 80% # of DPT3 /123 reported from HMIS 105 Jan 501 401 401 Feb 1002 520 921 Mar 1503 315 1236 Apr 2004 415 1651 May 2505 514 2165 Jun 3006 602 2767 Jul 3507 410 3177 Aug 4008 510 3687 Sep 4509 507 4194 Oct 5010 312 4506 Nov 5511 456 4962 Dec 6012 304 5266 DPT 3 cumulative 7000 Repoted number of DPT3 6000 5000 target 80% DPT 3 cumulative 4000 3000 2000 1000 0 Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Month Figure Line Chart: Immunization Coverage Nakasongola district, data source health unit HMIS 105-2011 Ministry of Health -Resource Centre April 2012 51 4.3 DATA ANALYSIS FOR SERVICE UTILIZATION RATES: Objective o Be able to identify the high priority area and identify priorities for intervention o To be familiar with ten key indicators o Be able to create and describe the use of Bar chart Which of the following indicators are the most useful in monitoring the performance of your health facility? • % women of reproductive age (15-49 years) who are using (or partner is using) a contraceptive method • % women of reproductive age (15-49 years) who can identify at least two forms of modern contraception • % births attended by a skilled birth attendant • % children >= 1 year and < 2 years fully immunized (DPT3) • % children >= 1 year and < 2 years who received Vitamin A therapy • % children 0 to 6 months exclusively breastfed • % mothers receiving PNC after delivery • % mothers attending at least one ANC visit • % mother receiving TT injections • % mothers reporting appropriate behaviour for treating a sick child 4.4 DATA ANALYSIS FOR MONITORING WORK PLAN: The HMIS data can be used to monitor the achievements as per he set targets in the Work plan Below is the number of children immunised a DPT3 in Buginyanya H.C III in 2 in 2004 as reported on HMIS 105 Under CHILD IMMUNISATION section. The health facility had set a target as per column A and the number immunised in column B, column c obtains the cumulative DPT3 by adding the previous month results to the current month. Ministry of Health -Resource Centre April 2012 52 Year Cumulative DPT3 Targeted (A) Jan 12 13 13 Feb 24 17 30 Mar 36 25 42 Apr 48 35 60 May 60 33 68 Jun 72 55 88 Jul 84 45 100 Aug 96 91 136 Sep 108 59 150 Oct Nov Dec 120 132 144 120 225 200 175 No of children given DPT3 (B) Cumulative DPT3 Attained (C) 179 75 195 132 207 Cumulative DPT3 Targeted Cumulative DPT3 Attained 150 125 Cases 100 75 50 25 0 Months 4.5 .Using HMIS data in Epidemic Detection Epidemic detection requires well kept data and monition from the previous two years to have a trend. Below is and example of trend ongoing for Bukhalu H.C III as collected on Ministry of Health -Resource Centre April 2012 53 HMIS 105 OPD diagnosis – epidemic prone diseases section .Data was plotted was from Jan 2001 to November 2003. 20 18 16 14 Cases 12 10 8 6 4 2 0 Months The in-charge should use the information and prompt the following questions? What is the most likely underlying cause for this epidemic? If you need to change this pattern, what interventions should be adopted immediately? Which one of these interventions is within your control at the health facility level? How are you going to share this information with your staff? Which one of them is beyond your control at the health facility level and what needs to be done so that you can get the necessary support? 4.5 Analysis checklist: Facilitator’s notes: go through this checklist as a way of interesting the trainees that analysis is not business as usual but activity done for a purpose, and to make a positive Ministry of Health -Resource Centre April 2012 54 change in the way the health activities are done, and influence decisions at all levels. Several steps in the process of using data should be applied systematically when looking at data. Depending on the situation, some of these steps may be reduced in scope and time, particularly when action is urgent and timely interventions important. The main steps of data analysis are reflected in the following questions: 1. Are the data accurate? Do the data measure what they are supposed to measure? Were the calculations made correctly? 2. Are the data reliable? Are you confident that you could come up with the same numbers if you were to review the source registers and documents again? 3. Do any of the numbers cause you immediate concern or alarm even before doing any additional calculations? Sometimes you might find a figure that seems way out of line with all of the others! Did someone enter an extra 0 – a common mistake that inflates122 numbers? Are too many priority drugs out of stock? Does the number of emergency purchases seem too high? 4. How do the numbers compare to previous time periods? Is there a trend towards improvement even if the numbers are not as good as you had hoped? Drawing a simple graph on a wall chart can help you identify such trends. 4. How do the numbers compare between/among geographic areas? Are some areas more successful than others? Do some areas need extra help attracting new clients or reevaluating their procurement methods? Does more training or IEC work need to be done for BHC staff or community? 5. If the reports identify specific problem areas, what might be the causes? Are certain factors external to the program possibly responsible for some of the problems (e.g., economic problems of clients)? What are the internal causes? (e.g., poor estimation of drug requirements, delays in processing orders). Think also about changes in community characteristics, such as an aging population or decreasing pool of potential new patients. 4.5 MAPS Ministry of Health -Resource Centre April 2012 55 Maps provide the advantage of visual presentation of the geographical distribution of cases. Thus, it is easier to identify the location of cases to get an idea of how communicable diseases are spreading. For example, diarrhea cases may be seen as a cluster in one area. If there is a map of the catchment area of the health facility available, certain cases--especially EPI target diseases--can be marked by pins. Community mapping has been used successfully in several countries as a useful tool for non-literate health workers to monitor the health status of families in their catchment area. At region level and national levels, coverage rates by district quickly let planners distinguish between well-served and less well-served areas and populations. Exercise 4: Data analysis and use For HSD, hospitals and district level trainees Case study Activity 1: The DHT has come to supervise a HC III, the MFP checks the stores stock cards for the number of doses given out in the previous month. The stock cards were found filed in the box file placed in the in charge’s desk ; the stock cards show that 200 blue , 412 green; 200 red , 400 brown doses of ACT were released from the stores in that month , however the total number of doses available is noted as 30000 on the stock card. All Coartem different pack are available in stock as per the stock card records, on checking the HMIS register it show only 1200 malaria cases were seen in that month 1. Explain how you would use the data to advise the health unit stock management system. 2. As part of the H.C III management team, explain the procedures you would take to address these gap. Case study Activity 2: The VHT report show 183 VHTs reported out of the 220 in the Ntwetwe H.C IV catchment area, the VHT supervisor has complied data from these VHT and the total number of children treated were 540. Only 320 were followed up after 3 days and Ministry of Health -Resource Centre April 2012 56 only 120 had taken the medication given. The VHT report also shows that 104 of the caretakers own mosquito net but 24 had slept under a mosquito net the day before reporting for treatment. State clearly what useful information and malaria indicators can be computed from this data. Discuss within your group how this data can be effectively utilized to improve the health education and fill in the gaps of the VHT system. Key points to highlight during assessment: % of VHT reporting Follow up rate Estimate of proportion of children with a net Estimate of net use Health education of adherence , was the right information given during treatment seeking, are the CMDs still competent enough, refresher course of CMDs , when were they last supervised? Ministry of Health -Resource Centre April 2012 57 Group work /exercise Case study Activity 3: HSD, HOSPITALS and District This exercise is to highlight that Useful interests of data can be got from the initial stage of eye bowling and suspected error checks could be investigated.) Data on the malaria laboratory tests are done for six month in 2008 in a particular health facility were as follow: Jan Feb MARCH APRIL MAY JUNE 112 245 99 2886 145 185 What can you say about this data?? Cross Tabulation Age by laboratory results among malaria suspected cases Age group Malaria results +ve -ve total Under 5 year 120 25 145 Above five years 65 60 125 Total 185 85 270 What are the useful percentages in relation to malaria? Column percentages or row percentage? calculate test positivity rate among children calculate test positivity rate among adults Ministry of Health -Resource Centre April 2012 58 Trainers Guide: Direct the trainees to fast have a Data overview and feel by first thinking through what are the numerator and denominator, which percentage are more important? Example of for HC II & III data use: Consider 420 outpatients who have been recorded in the OPD register. Among these clinical diagnosis column shows 320 have been suspected to be having malaria .if the disease of interest is malaria then the proportion of malaria cases is It’s further found out that of the 420,210 were children under five and of the 320 malaria suspects 183 were children. Present this data in a table. Of age group by malaria case Age group Suspected malaria with Not suspected to be having malaria Under five 183 b 5 years and above a c Total 320 210 100 420 Find a, b, c Age group by malaria confirmed cases Calculate the proportion of malaria suspected cases per each age group: a) under five year and b) Those aged 5 years and above Ministry of Health -Resource Centre April 2012 59 Of the 320 suspected malaria cases, 200 were taken to the laboratory for confirmation. Calculate the malaria test ratio or lab test ratio. From the laboratory register, 83 were found to be positive. Obtain the test positivity ratio or Proportion of positives. What would be the excess malaria treatment doses used if the laboratory tests were not done i.e. only clinical diagnosis was used. Facilitators guide: The trainees can refer to Annex 2 for more information on each indicators and how they can be presented and analysed. Print it out for each person. Ministry of Health -Resource Centre April 2012 60 SESSION 5: DATA INTEPRETATION, SHARING INFORMATION AND PROVIDING FEEDBACK Objectives: Understand the importance of feedback in program improvement and management List potential barriers to providing feedback Identify priority decisions and programmatic questions Link decisions/questions with potential data sources Create a time-bound plan for using data in decision making Consider how to improve feedback mechanisms in participants’ each level. Facilitators guide: Asks for group participation. Before moving on to the next session, ask participants if everything was clear and if they would like to discuss any of the concepts or topics further. 5.1 INTERPRETING DATA Data is usually interpreted in relation to a specific indicator: Indicators An indicator is an indirect measure of an event or change in a situation; it is a structured way to recognize patterns of data. When studying complex situations or events, it is often impossible or impractical to study each of the many factors that contribute to it. Measurement of carefully selected indicators (see also Annex 1 – Indicators will allow getting a good idea about the event or situation. If the indicator changes, we conclude Ministry of Health -Resource Centre April 2012 61 that the event of the situation has changed accordingly. Indicators could be discussed under data processing as well: the indicators we chose tell us how to rearrange data to present them in a more understandable way. Did you recognize any data patterns? The following patterns should immediately be looked for. Spikes are unusual or sharp increases in the number of cases. Spikes can indicate an outbreak of a disease. At clinic level you may notice spikes even during your work while you are examining and tallying the patients. In such cases, you should not wait for the end of the month. You should inform the authorities and start investigation and action immediately. Line graphs and frequency tables are useful for identifying and recording spikes. Clusters are groupings of cases by time period, area, age and sex groups, etc. This can indicate an epidemic or endemic that is limited to a certain place, group of people and period of time. Comparison of frequency and relative frequency of cases in different age and/or sex groups in a clinic and between/among different clinics can be helpful in this regard. Comparison of the top 10 cases in different health facilities is also helpful as well as pie, line and vertical bar charts. Trends are gradual increases or decreases in cases over time. Look carefully for trends, since they may occur so gradually that change is not observed. Identify trends by looking at the number of cases that have occurred and comparing them to the number reported in previous months and previous years (data of several years are needed for studying and learning trends as they are different in different areas). Trends are very useful to assess service coverage, making sure that the necessary stocks in required amounts are available to be used and timing of the leave schedules appropriately Ministry of Health -Resource Centre April 2012 62 in the year. The number of services delivered should increase over time until the target is reached. The line charts are extremely useful for this purpose. Seasonal variations. Regular changes occurring according to the time of year. The incidence of measles, diarrhea, ARI and malaria, for example, varies seasonally. Increased accessibility of facilities due to seasonal weather changes can explain a suddenly increased number of patient visits. A sudden spike or drop may be due to seasonal variation. Line charts are particularly helpful for displaying and identifying seasonal variations. Refer to Annex III on details of indicators and how they can be used /interpretation. 5.2 DATA PRESENTATION, SHARING AND FEEDBACKS: 1. Discuss reports with colleagues when they are first prepared. Include discussions of reports and structure of presentation (even preliminary findings) in regular staff meetings. Others can offer useful insights into why specific conditions are getting better or worse and have helpful suggestions about changes which could be made. The two main ways of summarizing data are by using tables and charts or graphs. A table is the simplest way of summarizing a set of observations. A table has rows and columns containing data, which can be in the form of absolute numbers or percentages, or both. Charts and graphs are visual representations of numerical data and, if well designed, will convey the general patterns of the data. The presenter should mind the audience the data is to be presented as this will determine whether the visual presentation will convey the message more at the tables or the combination. Ministry of Health -Resource Centre April 2012 63 If no structures report formats are provided, the presenter should pick the data to be presented relating to the priorities of the data sharing meeting. This can involve consultation with other National level officers, DHT members or health unit staff. Facilitators guide: It should be noted that HMIS data or health data is not only for the records people, and the HMIs focal person /biostatisticians in or national data bank but for all stakeholders in the health system. The more we get all members involved in data, the more they will be interested in the information from it and the more utilization of the data generated once it is shared. 2. Provide feedback to those who have sent reports or data from other units. Doing this can be as simple as acknowledging the receipt of the report, and responding to any issues that require your action. Better still, you can develop a routine mechanism to feedback some analysis of key indicators on reports you receive from all facilities. This should help them compare their performance with that of other reporting facilities. 5.3: LINKING DATA TO ACTION There is need to understand how to link the data we have with our programmatic questions and the decisions we need to make. Once the analysis is made, there is need to o Identify priority decisions and programmatic questions , o Link decisions/questions with potential data sources o Create a time-bound plan for using data in decision making. In the previous sessions, we discussed many of the concepts and tools, anaylsis methods that can facilitate data use in your setting. Ministry of Health -Resource Centre April 2012 64 Facilitators Note : Now let’s discuss the practical aspect of data use. How can you manage to build data use into your work? How do you ensure that data use becomes part and parcel of your day-to-day duties? The answer is to PLAN for it. These may be decisions and questions around: Program monitoring, planning, and improvement advocacy needs.( e.g increase the doses of malaria treatment in a Health center II medicine kit, number of staff required for immunization outreach etc may require advocacy with evidence based data at Health center II level to be sent to the upper levels ) Program management or operations issues based on the information obtained from the data. One needs to link the decisions and questions with data and then creates a timebound plan for decision making. It is also critical to involve others in your work because the best decisions are made with stakeholder involvement. For the data use to be effective , one needs to identify the ddecision makers and stakeholders with potential interest in your data and the information you have obtained from the interpretation, decisions / actions that the stakeholder makes, Questions to which the stakeholder requires answers and When the decision will be made One needs to know “What Are Decisions?” The following should be notes : Choices that can lead to action All decisions are informed by questions Ministry of Health -Resource Centre April 2012 65 All questions should be based on data For example: Some decisions may require Allocation of resources across districts / facilities,Revising VHT program approaches to emphasize testing every fever case, develop and institute PMTC policies on ANC clinics , Hire and allocate staff to facilities In some contexts, a decision cannot be identified before a key programmatic or policy question is answered. Or decision makers may have a question about their program for which they need an answer. It is the answer to this question that may provide the evidence that some kind of action needs to be taken to either improve or realign services. In these cases, we focus on identifying ‘programmatic questions,’ as opposed to decisions. Examples of programmatic questions: What percentage of HIV+ pregnant women in care actually are delivering in health facilities? What percentage of clients starting ART are lost to follow-up? Are the number of family planning clients decreasing? What percentage of pregnant patients who are HIV+ actually are receiving ART? Facilitator notes: In some cases, it may be helpful to have participants brainstorm a list of programmatic questions and not use the list above. As participants identify questions (or as you go through the list above), talk about what data could answer the questions, as well as what decisions might result from the data. Ministry of Health -Resource Centre April 2012 66 For example, if the monthly report data reveal that only 20% of women are delivering in health facilities, ask the participants to brainstorm solutions. Identify at least one decision that would need to be made. Lets use the PMTC T example to clearly see how we can derive actions: 1. Are we reaching testing targets in PMTCT? 2) Do we have sufficient test kits? 3) What is the nurse-to-client ratio in the clinic? let’s assume that the analysis informed us that the PMTCT program was no where close to meeting its targets for the year, the nurse-to-client ratio was far below acceptable, and there were sufficient test kits to reach programmatic targets. After this information was discussed with key stakeholders and interpreted in the context of the PMTCT program, the in-charge or DHT decided that additional PMTCT counsellors would improve program performance. What steps would be taken. For Linking Data with Action to be effective one needs to: 1) Creates a time-bound plan for data-informed decision making by setting dates by which data should be reviewed in relation to key programmatic questions and upcoming decisions. 2) Encourages greater use of existing information by identifying existing data resources and linking that information with the programmatic questions that need answers to support evidence-based decision making. Last, it provides you with a data-informed decision-making ‘record’ so that you can— Ministry of Health -Resource Centre April 2012 67 3) Monitor the use of information in decision making — Provides a timeline for conducting analyses and making decisions. Facilitator’ notes It should be noted that Building data use into your work takes planning and dedicated time Data should be linked to specific decisions so as to facilitate use Relevant stakeholders should be involved in each step of the process so that they appreciate its relevancy. For District Level training Examples: The health worker was complaining of heavy workload. The health unit has 2 midwives, 2 clinician (1 in charge, 1 laboratory assistant, 4 nurses) who claim they cannot handle the workload. The health facility has no records officer and the in charge rarely sends monthly report to the HSD. The last report sent to the HSD three months ago shows the OPD attendance of 1004 patients in the month of May approximating to 82 patients per day with no report on impatient data at all .(no HMIS 108). The unit has piles of ANC register in the stores and OPD counter books as stationery in the In-charge’s office but are not filled. You have headed a team to supervise this health facility describe how you can help this in-charge be able to manage this health unit and be able to convince the DHT that he needs more staff. State both immediate and long-term actions. Ministry of Health -Resource Centre April 2012 68 ANNEX 1: DATA MANGEMENT AND USE ACTIVITIES AT VAROUS LEVELS Service Delivery Data Management activities at various levels [1] At National Level The Biostatistician at the Resource Centre is responsible for: • Receiving all district data (including those from the national referral hospitals. • Ensuring entry of all district data (including those from the national referral hospitals) onto the District Health Information System (DHIS) software package. • Analyzing the quality of all reports received and ensuring follow-up in case of incompleteness, problems with validity, as well as delays. • Compiling all reports from the districts & NRHs into a single national report using the DHIS software. • Preparing an analysis of the data for discussion during the SMER TWG meetings and sector performance review meetings for decision-making. • Providing quarterly feed-back to the districts / NRHs. • Disseminating weekly IDSR reports to all stakeholders and community. • Disseminating quarterly district performance reports at sector review meetings. At District Level The District Biostatistician, or, where this position in not filled, the HMIS focal person, is responsible for: • Receiving all health unit data (including those from the general and referral hospitals). Ministry of Health -Resource Centre April 2012 69 • Entering all health unit data (including those from the general and referral hospitals) onto the District Health Information System (DHIS) 2 software package. • Analyzing the quality of all HMIS reports received and ensuring follow-up in case of incompleteness, problems with validity, as well as delays. • Compiling all reports from the units into a single district report using the DHIS 2 software. • Preparing an analysis of the data for discussion by the DHT for decision-making and participating in the DHT discussion. • Forwarding the DHIS 2 report electronically to the RC. If not possible, deliver the physical report by the 28th day of the following month. • Providing quarterly feed-back on data management to the health units. • Disseminating quarterly district assessment reports to DHMT. • Disseminating annual district performance report to District stakeholders’ forum. At Health Sub District Level The HSD Health Information Assistant is responsible for: • Receiving all health unit data (including those from the private providers) in the HSD. • Entering all health unit data (including those from the private providers) into the HSD databank. • Analyzing the quality of all HMIS reports received and ensuring follow-up in case of incompleteness, problems with validity, as well as delays. • Compiling all reports from the units into a single HSD report. Ministry of Health -Resource Centre April 2012 70 • Preparing an analysis of the data for discussion by the HSD Team for decisionmaking and participating in the discussion; • Forwarding the HSD report to the DHO by the 14th day of the following month; • Providing quarterly feed-back on data management to the health units. • Disseminating quarterly HSD assessment reports to HSD Team. • Disseminating annual district performance report to HSD stakeholders’ forum. At Health Facility Level All Health Providers including those from the private and community (VHT) are responsible for: • Collecting patient data using relevant patient forms. • Compiling relevant patient data from patient forms and entering it into the patient registers on a daily basis. The Health Information Assistant (HIA) or Medical Records Officer, or, where there is no HIA or MRO, the Health Unit In Charge or a designated person is responsible for: • Regularly compiling relevant patient data from patient registers and community (VHT) into the health facility HMIS database. • Analyzing the quality of all patient registers and community reports received and ensuring follow-up in case of incompleteness, problems with validity, as well as delays. • Compiling all reports from the sections/units / departments into a single health facility report using the health facility HMIS database. Ministry of Health -Resource Centre April 2012 71 • Plotting monthly performance on the displayed monitoring graphs. • Preparing an analysis of the data for discussion within the health facility for decisionmaking methods and participating in the discussions. • Forwarding or delivering the health facility report to the HSD/DHO by the 7 th day of the following month; In case of IDSR data weekly reports should be forwarded every Monday. • Providing quarterly feed-back on data management to the sections / units/ departments and community (VHTs). • Disseminating of monthly performance during monthly facility meetings. • Dissemination of quarterly facility assessment reports to the HUMC / Hospital Board. • Dissemination of annual facility performance reports to the Sub County forum. At Community Level All Community Health Providers (VHT) are responsible for: • Collecting patient/client, or activity data using relevant forms. • Compiling data from the relevant forms and entering it into the VHT Register on a regular basis. • Compiling relevant data from the VHT register into the VHT Report. • Preparing an analysis of the data for discussion within the VHT for decision-making methods and participating in the discussions. • Forwarding or delivering the VHT report to the nearest health Centre by the 5th day of the following month; Ministry of Health -Resource Centre April 2012 72 • Disseminating quarterly performance report data to Parish Committee. ANNEX II: LIST OF INDICATORS RELATED TO HEALTH SERVICES PROVIDED AT FACILITY LEVEL AND HOW THEY CAN BE PRESENTED: Summary of the list of indicators related to health services provided at facility level and how they can be analyzed: Reporting % of reports received (received reports table) Health problems Number of new cases in all age and sex groups (frequency table) % of new cases in all age and sex groups (percentage table) % of positive slides for malaria (percentage table) Health problems in children < 5 years Number of new cases in children < 5 years (frequency table for children < 5 years) % of new cases in children < 5 years (frequency table for children < 5 years) Number of neonates delivered < 2500 g (frequency table) % of neonates delivered < 2500 g (percentage table) Health problems in different age and sex groups Number of new cases in all age and sex groups (frequency table) % of new cases in different age and sex groups (percentage table) Quality of practices % of re-attendance (percentage table for re-attendance) % of pneumonia among all ARI cases (percentage tables) % of acute bloody diarrhea among all diarrheal cases (percentage tables) Ministry of Health -Resource Centre April 2012 73 % of blood tests in malarial cases (percentage tables) Reproductive health services Number of deliveries (frequency table) % of assisted deliveries among all deliveries (percentage table) Number of new antenatal visits (frequency table) Number of repeat antenatal visits (frequency table) % of 2nd antenatal visits out of new antenatal visits (percentage table) Number of other antenatal visits (frequency table) % of other antenatal visits out of new antenatal visits (percentage table) Number of women who came for at least one postpartum visit (frequency table) % of women that delivered who came for postpartum visit (percentage table) % of postpartum visits out of new antenatal visits (percentage table) Number of maternal deaths (frequency table) Number of neonatal deaths (frequency table) Number of stillbirths (frequency table) Utilization of health services Total number of OPD visits (frequency table) Percentage of different age and sex groups (pie chart) Ministry of Health -Resource Centre April 2012 74 ANNEX III: INDICATORS WITH SOURCES OF DATA AT THE HEALTH FACILITY AND HOW THE INFORMATION CAN BE USED: INDICATOR DEFINITION HOW TO USE IT Numerator: Number of total OPD attendance attendance OPD RATES (i.e. and new re- UTILIZATION attendance). Information on the service delivery system and the use of the Denominator: Catchment service by the community. population for the year in question or catchment population/4 for the quarter. Numerator: Number of patient bed days in a given BED RATE OCCUPANCY period (e.g. quarter or year) x 100 Denominator: Number of beds in institution x Number The bed occupancy rate gives the average percentage of occupied beds during the period under review(usually one year). The bed occupancy rate should ideally be 80% or more. Two sets of parameters determine the occupancy rate: the need for service, and the service delivery factors. Ministry of Health -Resource Centre April 2012 75 INDICATOR DEFINITION HOW TO USE IT of days in time period under review It is estimated that in areas of high malaria transmission, 23% of deaths among children under 5 years are attributable to malaria Numerator: Number of deaths in children under 5 due to malaria in health unit(s) MALARIA - CASE (x100) FATALITY RATE IN Denominator: CHILDREN UNDER 5 Number of cases of diagnosed malaria among children admitted to health unit(s). under 5 and 11% in areas with medium transmission intensity based on findings from verbal autopsy study in western Uganda. The under 5 mortality of 159/1000 live births (DHS 1995) in Uganda translates into a malaria specific mortality of 37/1000 in high malaria endemic areas and 18/1000 in low endemic areas, to a total of 70,000-110,000 child deaths annually. The case fatality rate is probably more closely related to quality of service than the incidence rate. Even if the number of deaths is too small for the CFR to have statistical significance, each death should prompt an investigation regarding case management, referral, treatment failure and other related factors. Ministry of Health -Resource Centre April 2012 76 INDICATOR DEFINITION Numerator: HOW TO USE IT Number of deaths due to pneumonia in health unit(s) ( x 100) ARI-PNEUMONIA CASE FATALITY RATE Denominator: cases Number of of Same as malaria above diagnosed pneumonia admitted to health units(s) Numerator: Number of deaths due to diarrhea in DIARRHOEA FATALITY RATE CASE health units (x 100) Denominator: Number of cases of diagnosed diarrhea cases admitted to health units CUMULATIVE INCIDENCE SEXUALLY An increasing case fatality rate should lead to an analysis that includes review of the availability of drugs and supplies and of the rational use of pharmaceuticals. The possibility of missed outbreak of cholera or dysentery should not be dismissed Numerator: Number of new The Sexually Transmitted Infections that are captured using HMIS OF cases of STIs in health units (x 105 are categorized as; 1000) Urethral Discharges, Transmitted Infection due to Gender Based Ministry of Health -Resource Centre April 2012 77 INDICATOR DEFINITION HOW TO USE IT TRANSMITTED Denominator: INFECTIONS aged above fifteen years old in STI incidence should be monitored by comparing its value with Population Violence, and the catchment area. Other Sexually Transmitted Infections that of the same time period in the previous year. Investigation and action should follow an increase of 15% from the earlier time period. To follow time trends in a single area, counts of STD cases may be monitored instead of incidence. Ranking the village incidence rates can identify priority areas for STD interventions, particularly prevention. Interventions include IEC campaigns, as well as promotion of the use of condoms. Numerator: Number of cases of TB notified annually x 100%. TB RATE NOTIFICATION Denominator: Expected number of TB cases for the catchment population in the same period. CASE NOTIFICATION Numerator (N): Total number NTLP Quarterly treatment outcome report forms. Ministry of Health -Resource Centre April 2012 78 INDICATOR DEFINITION RATE (CNR) of all new TB cases and relapse smear HOW TO USE IT positive TB cases (D): Total notified per year Denominator population in the catchment area. Case notification rate = N/D X 100,000 Numerator: reported NUMBER CASES OF OF NEW Flaccid Number cases of Paralysis of Acute AFP is a notifiable disease and a single case should be among investigated with follow-up at all levels of the ACUTE people less than 15 years of FLACCID PARALYSIS age x 100000. Denominator: service delivery system. AFP may only be confirmed as poliomyelitis after investigation and Population confirmation following the WHO criteria. aged less than 15 years. Ministry of Health -Resource Centre April 2012 79 INDICATOR DEFINITION HOW TO USE IT Progress is monitored monthly at the health unit graphically. At Numerator: Number of new health Health Sub-Districts, Districts and MOH clients at antenatal clinic (x headquarters, the proportion of new pregnancies attended ANTENATAL ATTENDANCE COVERAGE units, 100) Denominator: should be analyzed quarterly and annually. Number of When the attendance is lower than targeted, reconsider the estimated pregnancies in the strategies. catchment population Identify the districts/parishes/villages with low attendance. Contact the community and find a solution with them: e.g. intensified information or organize an outreach. At health units, health sub-districts, districts and MOH Numerator: Number of TT2, headquarters, the proportion of new pregnancies attended TT3, TT4 and TT5 doses given should be analyzed quarterly and annually. TETANUS COVERAGE TOXOID to pregnant Women (x 100) Denominator: Number The coverage of pregnant women attending Antenatal Clinic with of TT vaccine is an indicator of quality expected pregnancies in the of care. Ideally, we would also want to know the percentage of same period women in the entire country whose pregnancies (and therefore newborns) are protected. Overall coverage of the population of is Ministry of Health -Resource Centre April 2012 80 INDICATOR DEFINITION HOW TO USE IT estimated at around 90% of pregnant women COVERAGE OF PREGNANT WOMEN WITH PRESUMPTIVE TREATMENT FOR (IPT) MALARIA USING S-P Numerator: Number pregnant women receiving 2 doses of S-P in a given period (x 100) Denominator: Number of new ANC attendances in a given period Numerator: PERCENTAGE of Number of OF deliveries in health facilities (x DELIVERIES TAKING 100) PLACE IN A HEALTH Denominator: FACILITY expected Number births catchment population in of the Coverage of pregnant women with malaria prevention is a national preventive target. At heath Units, Health Sub-Districts, Districts and MOH headquarters, the proportion of women attending for Antenatal Clinic who receive two doses of Fansidar should be analyzed quarterly and annually. National Target is 80% and each heath unit should strive for that target. The number of deliveries in maternity is monitored monthly as a national preventive target. Progress is monitored monthly at health Unit and reported. If deliveries decline while ANC new clients do not, it is necessary to find out why and correct the situation. This may include decreasing or eliminating user fees for delivery. Ministry of Health -Resource Centre April 2012 81 INDICATOR DEFINITION HOW TO USE IT CAESAREAN SECTION RATE Numerator: (NUMBER Number of OF Caesarian section in Hospitals CAESAREAN and Level IV Health Centres x SECTIONS PER 100 100 DELIVERIES WITHIN Denominator: THE CATCHMENT AREA OF deliveries Number within of the THE catchment population This indicator is intended to measure whether or not Hospitals and Level IV Health Centers are fulfilling their role in providing a service, namely caesarian section, which cannot be provided at lower levels of the health system. At level IV Health Units, HSD, District and National Level, analysis is recommended on an annual basis. HEALTH FACILITIES) Numerator: Number of children under one year of age BCG VACCINATION COVERAGE who have received BCG immunization (x delivery and providers’ delivery procedures should be investigated. Activities to increase accessibility to BCG at birth include increasing facility based deliveries, vaccinating the baby 100) Denominator: If the coverage is falling, the availability of vaccine, health service Number of children under one year in the before discharge of the mother and assuring availability of the vaccines. Ministry of Health -Resource Centre April 2012 82 INDICATOR DEFINITION HOW TO USE IT catchment area. Numerator: Number of children under 1 year of age DPT-HepB+Hib VACCINATION COVERAGE 3 who have received 3 doses of At health unit, DPT-HepB+Hib coverage should be calculated, DPT-HepB+Hib analyzed and graphed monthly and quarterly. At health sub- vaccination ( x 100) districts, Denominator: Number districts, and national MOH headquarters, DPT- of HepB+Hib coverage should be calculated quarterly and annually. children under 1 year in the catchment area. Numerator: Number of At the health unit, measles immunization coverage should be children under 1 year of age calculated, analyzed and graphed monthly, and quarterly. At MEASLES who have received the 1st health sub-districts, districts, and national MOH headquarters, VACCINATION dose of measles COVERAGE Vaccine before age 1 (at 9 and annually. Measles vaccination coverage should be compared measles coverage should be calculated and graphed quarterly months of age) (x 100) Denominator: Number to the measles incidence rate (use case based measles of surveillance data) to confirm that the vaccine is conveying Ministry of Health -Resource Centre April 2012 83 INDICATOR DEFINITION HOW TO USE IT children under 1 year immunity. If the number of cases is increasing (or indeed not declining over previous years), this may indicate a diminished effectiveness of the vaccine. An investigation into possible breakdowns in the cold chain should be investigated. This indicator is for nutritional surveillance of young children in Numerator: children UNDERWEIGHT PREVALENCE Number at of measles immunization with weight for AT age below the bottom line MEASLES (x 100) IMMUNISATION Denominator: Total number of children weighed at measles vaccination the service area. Each month the estimate is for a different group of children (those receiving measles vaccinations). There could easily be some seasonal variations since this age group of children is extremely vulnerable to food shortages. It is most important during times of disaster (floods, droughts) but it is an indication of general economic well being in the area, and therefore trends over years will also be important to document. Comparison of locations: Priority areas for nutrition interventions, particularly prevention and modification in treatment protocols, Ministry of Health -Resource Centre April 2012 84 INDICATOR DEFINITION HOW TO USE IT can be identified by ranking the areas’ prevalence rates. This can be done through a register review, which identifies the villages or parishes with the highest prevalence. At health units, health subdistricts, districts, and MOH headquarters, the proportion of children below two standard deviations from the bottom line is analyzed quarterly and annually. Children who are identified in this category should be followed up through outreach programs. PERCENTAGE VILLAGES VILLAGE OF WITH HEALTH TEAMS PERCENTAGE VILLAGES Numerator: Number of villages with Village Health Teams x 100 Denominator: Number villages in catchment area OF Numerator: Number of The indicator should be analyzed quarterly at health unit, HSD level, District and National levels. Special effort should be made to help form VHT in villages where active community participation in health does not exist. Community Health Workers can assist in formation and functioning of these committees. of Emphasis should be placed on raising the awareness in the WITH villages with known access to population of the relationships between their health and ACCESS TO WATER safe water x 100 surroundings. Collaboration with relevant agencies for the Ministry of Health -Resource Centre April 2012 85 INDICATOR DEFINITION Denominator: HOW TO USE IT Number of promotion of safe water should be made at all levels. This villages in catchment area indicator is monitored quarterly and annually at health unit, Health sub-district and District levels. PERCENTAGE PLANNED OF Numerator: Number of outreach activities conducted OUTREACH Denominator: ACTIVITIES CONDUCTED Number of outreach activities planned This indicator monitored monthly at health units, HSD and Districts levels. It will monitor the availability of staff and implementation of Outreach activities t from the health unit staff to a community to conduct preventive promotion activities such as immunization, growth monitoring, family planning, The HSD team and Health Unit staff should make efforts to avoid NUMBER TRAINED OF Numerator: of drop outs from those who have been trained for these voluntary VILLAGE trained Village health Teams HEALTH TEAMS PER Denominator: VILLAGE Number Number positions; regular meetings with CHWs/VHTs and public of recognition of their importance can help reduce drop outs. villages in the catchment area This indicator is monitored quarterly at health units, Health subdistricts, district and National levels. It is important to work with Community-Based Health Care programmers so that the support Ministry of Health -Resource Centre April 2012 86 INDICATOR DEFINITION HOW TO USE IT is optimized to the benefit of all. CHWs can be very useful to create an effective patient/client follow-up system. The In-charge can prepare a list of outpatients who do not return for continuing treatment (e.g. TB), or children who late for immunizations, or women who need to come for the next Tetanus booster. The CHW can visit those persons to remind them of their appointment. At health units, health sub-districts, districts and National level, Numerator: Number of health stock-outs of drugs is monitored monthly : Essential drugs for PERCENTAGE OF units reporting no stock outs monitoring the Health Sector Strategic and Investment Plan FACILITIES WITHOUT of any of the six essential (HSSIP) are First Line ANY drugs in a STOCK-OUTS FOR given time period ESSENTIAL DRUGS Denominator: health units Drug for Malaria, Cotrimoxazole tablets, Measles vaccines, Fansidar,Depo-provera and ORS sachets. Number of Monthly monitoring of the stock conditions is done through the HMIS reports received at the MOH Resource Centre. An adequate stock level is a level between the maximum and the Ministry of Health -Resource Centre April 2012 87 INDICATOR DEFINITION HOW TO USE IT minimum. A stock out of any of the essential medicines should not happen at any one time in any health facility as it is an indication of inadequate stock management, or of an unplanned extremely large increase in use, or routine misuse of the commodity. In normal circumstances, the Balance on Hand should not fall below the minimum. If this happens, then if an order has already been placed, ensure that it will arrive before a stock out occurs. If an order has not been placed, then an emergency order should be made. Minimum and maximum values may need to be adjusted. The stock control system may be one cause of the problem, but health unit in-charges should also consider the possibility of, pilferage, prescription habits of staff, and changes in disease patterns. Measures should be taken to correct the problem found. In the eyes of the general public the availability of drugs in health Ministry of Health -Resource Centre April 2012 88 INDICATOR DEFINITION HOW TO USE IT institutions is key for the confidence in the health system. At Health Units and Health Sub districts, staff workload by type of service provided is analyzed quarterly and annually. At District Numerator: contacts Total client (disaggregated by OPD, antenatal/postnatal care, DAILY STAFF WORK immunizations LOAD and family planning) Denominator: Number of clinic days (disaggregated by type of service as above) and MOH headquarters total staff daily workload (not disaggregated by services) is analyzed quarterly and annually. The number of attendance per staff member per clinic day is a measure of the workload. From this you can also calculate how much time a clinician spends with each patient/client (by dividing the hours in usual clinic day by the number of attendance per staff member per clinic day). If the available time is too short, the quality of care declines. Since a Health worker who has a low work load will never complain, this will not be noticed unless calculations are done. An unfair distribution of workload will undermine staff relations. ON-TIME HEALTH Numerator: Number of Routinely, the In-charge should be observing the recording of Ministry of Health -Resource Centre April 2012 89 INDICATOR DEFINITION MANAGEMENT monthly reports received on information for all the services the health unit provides and INFORMATION or before the due date during making corrections as needed. In addition, at the end of a SYSTEMS the time period reporting period, the aggregation of the totals for reporting must (HMIS) REPORTING (x 100) be done correctly. If late reporting is a general problem, the Denominator: HOW TO USE IT Number of health sub district should take measures to speed up reporting. reports expected during the Support supervision may provide an opportunity to encourage time period on-time reporting and to collect reports. Ministry of Health -Resource Centre April 2012 90 a) PMTCT 1. Number of pregnant women tested for HIV 2. Number of pregnant women tested HIV positive 3. Number of HIV positive pregnant women given ARVs by regimen 4. Proportion of babies born to HIV positive mothers who tested HIV positive 5. Proportion of HIV positive mothers who accessed family planning services b) ART 1. Number of new patients enrolled in HIV care at Facility during the quarter 2. Number of pregnant women enrolled into care during the quarter. 3. Cumulative Number of individuals on ART ever enrolled in HIV care at facility 4. Number of HIV positive patients active on pre-ART Care 5. Number of HIV positive cases who received CPT at last visit in the quarter 6. Number eligible patients not started on ART 7. Number of new patients started on ART at facility during the quarter 8. Number of pregnant women started on ART at facility during the quarter 9. Cumulative Number of individuals on ART 10. Number of HIV positive patients assessed for TB at last visit in the quarter 11. Number of HIV positive patients started on TB treatment during the quarter 12. Number of people accessing ARVs for PEP c) VCT 1. Number of clients received Pre test counseling 2. Number of clients Tested 3. Number received their HIV results Ministry of Health -Resource Centre April 2012 91 4. Number of clients Received HIV results for the first time in this financial year 5. Number of clients Counseled and tested as a couple 6. Number Received results as a couple 7. Number of Discordant results 8. Number of TB Suspect 9. Number of clients Started on CPT 10. Number of clients who received HCT for PEP 11. Number of clients Linked to Care Ministry of Health -Resource Centre April 2012 92 ANNEX IV: Section 2 – Generating Demand for Data Activity 1 – Case Study Review Instructions: Select a reporter. Read the case study assigned to your group (either the first or the second case study) and answer the following questions (45 minutes): o What prompted the data use undertaking? o What was the decision made? o What types of data were used to make the decision? o What was the outcome of the decision? o What can you comment on such kind of data collection arrangements of partners I the district. Report back. (10 minutes per group) Case study #1 MUJAP The MUJAP in wakiso from January 2009 and by September 2011 was assisting 12 service sites (Local Partner Treatment Facilities, or LPTF) to provide antiretroviral therapy (ART). As of the end of September 20011, the program had tested 103,685 individuals for HIV, enrolled more than 7,840 people in care, and started 3,852 clients on ART. Each LPTF provides services at a health facility (either a hospital or health center IV) and supports community outreach. MUJAP utilizes a system known as IQ Chart to collect patient data necessary for its ART programs. IQ Chart is an electronic patient management and monitoring system that allows service sites to collect, store, and analyze patient-level data. In May 2011, an IQ Chart report showed that a large number of clients were missing their scheduled appointments for antiretroviral (ARV) drug pick-up. The central office discussed the findings with each site’s clinical team. The initial reaction from the clinical teams was that the number of patients who allegedly missed appointments was inflated; they did not believe that so many patients had missed their ARV appointments. To determine the true cause, the clinical teams requested an investigation to determine if this was a data quality issue, or if many patients were in fact missing appointments. MUJAP had a multifaceted problem to solve. If the quality of data was poor, the Ministry of Health -Resource Centre April 2012 93 organization needed to reinvest in training service site staff in data collection techniques; if the data quality was sufficient, it needed to address the fact that many people were missing their appointments. Using patient data already collected and stored, the office generated a list of names and addresses of every patient marked as more than 20 days overdue for an ARV pick-up. The lists were given to clinicians and community coordinators for individual follow-up and verification at both the facility and the patient’s home. It was determined that patient records were indeed correct. This resolved the issue of data quality of existing medical records. As a result, MUJAP instituted new procedures to strengthen support services to ARV patients. Each community volunteer was assigned eight ART clients whom he/she was expected to visit weekly. New forms were designed for the volunteers to report on their clients, and monthly meetings were scheduled with the community coordinators to share and discuss the information collected and their experiences in supporting clients. With improved increased availability of data on ARV client progress, it was possible to provide a higher standard of care. Every site now monitors weekly ARV pick-up, CD4 testing, and care support. With improved data available at the service sites, clinicians now use the reports to identify problematic patients. Community volunteers then follow up with these patients to ensure that they continue with the drug regimen. As a result of these program improvements, the quality of life of program beneficiaries has improved. The number of patients lost to follow-up has dropped significantly. Anecdotal reports suggest that community volunteers have become more visible in their communities, which has encouraged other PLHIV to join the program and seek HIV-related services. Ministry of Health -Resource Centre April 2012 94 6.0. REFERENCES 1. Health Sector Strategic and Investment Plan, 2010/11 – 2014/15. 2. HMIS Health facility manual 2010 3. HMIS District Manual 2010 4. MOH- indicator for monitoring indices and the Health Sector Strategic and Investment Plan In Uganda , The User indicator Manual 5. Standard Operating Procedures for health information 6. MEASURE evaluation data use training materials. 7. Designing and Conducting Health systems Research projects Volume 2, Part 2, WHO 2005 Ministry of Health -Resource Centre April 2012 95