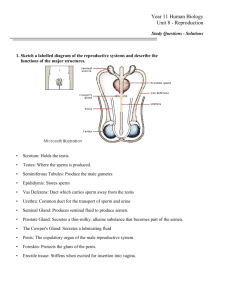
Male Reproductive $ystem
advertisement

The reproductive system produces, stores, nourishes, and transports functional gametes. By: Erin Whatley, Chontel Childress, Jevin Clinkscales and Kendel Shanks • • • • The decent of the testes through the inguinal canals occur during fetal development. The testes remain connected to the internal structures via the spermatic cords. The raphe marks the boundary between the two chambers in the scrotum. The dartos muscle tightens the scrotum, giving it a wrinkled apperance as it elevates the testes; the cremaster muscles are ore substantial muscles that pull the testes close to the body. The tunica albuginea surrounds each testis. Septa extends from the tunics albuginea to the region of the testis closet to the entrance to the epididymis, creating a series of lobules. Seminiferous tubules within each lobule are the sites of sperm production. From there, spermatozoa pass through the rete testis. Efferent ductules connect the rete testis to the epipdidymis. Between the seminferous tubules are interstitial cells, which secrete sex hormones. • Seminiferous tubules contains spermatogonia, stem cells involved in spermatogenesis (the production of spermatogonia) , and sustentacular cells, which sustain and promote the development of spermatozoa. • Each spermatazoon has a head tipped by an acrosomal cap, middle piece, and a tail. • • • From the testis, the spermatozoa enter the epididymis, an elongate tubules with head, body, and tail regions. The epididymis monitors and adjusts the composition of the fluid in the seminiferous tubules. Serves as a recycling center for damaged spermatozoa, stores and protects spermatozoa, and facilitates their functional maturation. The ductus deferens, or vas deferens, begins at the epididymis and passes through the inguinal canal as part of the spermatic cord. Near the prostate gland the ductus deferens enlarges to ampulla. The junction of the base of the seminal vesicle and the ampulla creates the ejaculatory duct, which empties into the urethra. The urethra extends from the urinary bladder to tip of the penis. The urethra can be divided into prostatic , membranous, and spongy regions. • Each seminal vesicle is an active secretory gland that contributes about 60 percent of the volume of semen; its secetions contain fructose (which is easily metabolized by spermatozoa), bicarbonate ions, prostaglandins, and fibrinogen. The prostate gland secretes slightly acidic prostatic fluid. Alkaline mucus secreted by bulbourthral glands has lubricating properties. • A typical ejaculation releases 2-5 ml of semen (ejaculate), which contains 20-100 million spermatozoa per milliliter. The fluid component of semen is seminal fluid. • The skin overlying the penis resembles that of the scrotum. Most of the body of the penis consists of three masses of erectile tissue. Beneath the superficial fascia are two corpora cavernosa and a single corpus sponglosum, which surrounds the urethra. Dilation of the blood vessels within the erectile tissue produces an erection. • The Male Climacteric: During the male climacteric, at age 50-60, circulating testosterone levels fall, and levels of FSH and LH rise. A female’s reproductive system is vital for the existence of life. The uterus must be able to support and nourish a developing embryo and continue to nourish the infant after it is born. The major parts of the Female reproductive system include: the ovaries, the uterine tubes, the uterus, the vagina and the components of the external genitalia. The Ovaries are located on the lateral walls of the pelvic cavity Their three functions include: 1. Production of immature female gametes or oocytes 2. Secretion of female sex hormones (estrogens and progestins) 3. Secretion of inbulin and feedback control of FSH Oogenisis- Ovum production; Begins at the woman’s birth and accelerates during puberty and ends at menopause. Ovarian cycle: Divided in to two phases. The Follicular Phase and the Luteal Phase Step 1: the formation of primary follicles Step 2: the Formation of secondary follicles Step 3: Formation of tetiary follicles Step 4: ovulation Step 5: Formation and degeneration of the corpus Step 6: Unless fertilization occurs, the Corpus luteum degenerates after 12 days of ovulation (menstruation) Hollow muscular tubes divided in to three segments: 1. the Infundibulum: the end closest to the ovaries with finger-like projections called fimbriae. 2. The Ampulla: Located in the middle of the uterine tube, has smooth muscle layers 3. The Isthmus: A short segment connected to the uterine wall The Uterine tubes provide a nutrient-rich environment that contains lipids and glycogen which is essential for a developing embryo. The uterus provides mechanical protection, nutritional support and waste removal for the developing embryo. The Cervix: the inferior portion of the uterus that extends to the vagina. The cervix contains the cervical canal that opens in to the uterine cavity. Uterine wall: Contains thick outer muscular myometrium and an inner thin glandular endometrium. The Myometrium provides the force needed to move the fetus from the uterus to the vagina. The Endometrium provides supports the growing fetus, this layer also changes with the uterine cycle monthly. Uterine Cycle (Menstrual Cycle) Step 1: Mensus Mensus is when degeneration of the endometrium occurs. The functional zone is lost and this lasts for normally about seven days. About 30 to 50mL of blood is lost. Step2: Proliferative phase In the days after mensus, the epithelial cells of the uterine glands multiply across the endometrium and restore the uterus. Estrogens are secreted by the growing ovarian follicles. Step 3: Secretary Phase In the last stage, the endometrium glands enlarge, accelerating their rate of secretion. Also arteries in the uterine wall elongate and spiral in to the tissues of the functional zone. During this phase, ovulation occurs. If the egg is not fertilized, hormone functions stop and the mensus phase begins once again. The Vagina is an elastic muscular tube extending between the cervix and the vestibule The vagina has three major functions: 1. Serves as a passageway for eliminating menstrual fluids 2. Receives the penis during sexual intercourse, and holds sperm cells prior to their passing in to the uterus 3. Forms the inferior birth canal, in which the fetus passes. The vaginal lumen is lined with non-keratinized stratified squamous epithelium and when relaxed, forms rugae. The vagina contains healthy bacteria that keep it acidic to eliminates the growth of pathogens. Vaginitis: Inflammation of the vaginal canal caused by fungi, bacteria, or parasites The area containing the female genitalia is called the vulva The vagina opens up in to the vestibule bounded by small flaps called labia minora and labia majora The Urethra is located above the vagina An infant gains nourishment from milk secreted by the mammary glands. Mammary glands are controlled by hormones of the reproductive system, the mammary glands lie within surrounding fat pads Each breast has a nipple in which the mammary gland ducts open to the surface, the reddish-brown area around the opening is called an areola The female reproductive tract includes interplay between secretions of the pituitary gland and the gonads The hormones control the uterine and ovarian cycles Three estrogens circulate the blood stream: Estradiol, estrone, and estriol. Estradiol is the most prominent to ovulation FSH is the dominant hormone released by the pituitary gland Key facts: sexual intercourse involves the reproductive system of the male and the female Fertilization of a females egg can take place Presents tract semen into the female reproductive The male and female sexual functions cycle consists of excitement, plateau, orgasm, and resolution. the body responds with an increase in heart rate, blood pressure and respiration First is penile erection, it is produced by arteriolar dilatation and increased blood flow to the erectile tissue of the penis. Erection is a reflex response initiated by visual, or imaginative stimuli impinging upon supraspinal centers or by genital stimulation that in turn activates spinal reflex mechanisms, or an erection Sacral parasympathetic and thoracolumbar sympathetic nerves provide the efferent vasodilator input to the penis. Parasympathetic nerves also stimulate secretion from the seminal vesicles and prostate and Cowper's glands during the plateau phase. The orgasmic phase is characterized by seminal emission and ejaculation and the associated sensations. The release of semen into the urethra depends on sympathetic nerves that elicit contractions of smooth muscles in the vas deferens, seminal vesicles, and prostate. Rhythmic contractions of striated muscle (bulbocavernosus and ischiocavernosus) generated by efferent pathways in the pudendal nerve eject semen from the urethra. Any physical or psychological factor that effects a single component of the system can result in the male sexual dysfunction Depression Nervousness anxiety Viagra Prescription drugs, that enhances and prolongs the effects of nitric oxide on the erectile tissue Rhythmic contact of the penis with the clitoris and vaginal walls Touch sensation from breast and other stimuli Erotic thoughts (visual,olfactory) Blood flow to the genitals increases, resulting in swelling of the woman's clitoris, vaginal walls and labia minora (inner lips) Vaginal lubrication begins, moistening the walls of the vagina The woman's breasts become fuller, parasympathetic stimulation causes them to become more sensitive to touch and pressure Sexual intercourse along with oral sexual activity carries the risk of infection and diseases, Stds are transferred by contact and can effect any part of the body Chlamydia Gonorrhea Herpes Genital warts Syphilis Decline in infertility Decline in sexual abilities Changes to reproductive organs and accessory organs Preimenopause – the ovarian and uterine cycles become irregular Occurs around 40 Oocytes drop dramatically Estrogen levels decrease, not triggering ovulation Ovulation and menstruation cease Occurs around 45-55 Circulation concentration of estrogens and progesterone decreases Increase production of GnRH, FSH and LH Physical effects are reduction in breast and uterus size Thinning of urethral and vaginal epithelia Bone composition proceeds at slower rate Hot flashes Mental effects- depression, anxiety The male climacteric of andropause Age 50 and 60 FSH and LH increase Sperm production continues Sexual activity decreases because male dysfunction Since women's reproductive organ are more internal and house fetus, they require more medical care. Gynecologists -study and treat problems with the female genital, rectal and urinary organs. Additionally, many gynecologists consult on pregnancies, reproductive therapy and other areas of the patient's reproductive system. Urologist-A physician who deals with the study and treatment of disorders of the urinary tract in women and the urogenital system in men. Endometriosis is a problem with the lining of the uterus (womb). Normally, when you have your menstrual period every month, the lining (endometrial tissue) of the uterus will come out in the menstrual flow. Infertility affects over 6 million people in the United States, which represents about 10% of the reproductive-age population. Most infertility cases are treated with medication or surgery. Assisted reproductive technologies, for example, in vitro fertilization and similar treatments, account for less than 5% of infertility services. Infertility, which is often a reversible or treatable condition, should be distinguished from sterility, which implies an irreversible inability to conceive. Ovarian Cancer Prostate cancer Testicular cancer Ovulation Game Menstrual Cycles The average menstrual cycle is 28 to 32 days. Some women have longer or shorter cycles, so the exact timing of ovulation can vary. Here's an overview of a typical 28-day menstrual cycle. Day 1 Your cycle begins on the first day of blood flow. Days 2-14 Follicular Phase The follicles on your ovary become active, and your cervical mucus starts to thin. Day 14 Ovulation occurs mid-cycle, but can vary from between Day 11 and Day 21 of a woman's cycle. Rising estrogen levels trigger the LH surge, which causes the follicle to ovulate and release an egg. It's important to chart your basal body temperature and LH surge so you know when you ovulate. Days 15-22 Luteal Phase After releasing the egg, the follicle produces progesterone, which thickens the lining of the uterus for implantation. Days 23 to 24 Implantation of a fertilized egg can take place. At this point, hormones produced by pregnancy may be detected by a pregnancy test. Days 25 to 28 If pregnancy does not occur, your hormone levels begin to fall. The uterine lining sheds, resulting in your period. Martini, Frederic. Fundamentals of Anatomy and Physiology. Upper Saddle River, NJ: Prentice Hall, 1998. Print. "Ovulation Calculator from WebMD." WebMD. WebMD, 7 Mar. 2012. Web. 09 May 2013.