1-Kakkis-Workshop-5 - EveryLife Foundation for Rare Diseases
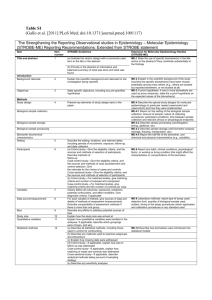
advertisement

Welcome to Workshop #5: Accelerated Approval (AA) in Rare Diseases: Review of a White Paper Proposal Emil D. Kakkis, M.D., Ph.D. President and Founder EveryLife Foundation for Rare Diseases May 15, 2013 Sofitel Hotel Washington, D.C. Lafayette Square The EveryLife Foundation For Rare Diseases • Formed to focus on improving the development of treatments of rare diseases in February 2009 • Conducting workshops and participating in conferences to help promote scientifically sound change • Supporter of ULTRA/FAST legislation in FDASIA • Working toward scientifically sound change to improve the accessibility of the Accelerated Approval pathway • 181 Partners+ Workshop Series Topics • Workshop #1 • Workshop #2 • Workshop #3 • Workshop #4 • Workshop #5 Statistical analyses of rare disease studies Clinical evaluation of rare disease treatments Surrogate endpoints & accelerated approval Developing Policy Recommendations for Accelerated Approval Accelerated Approval in Rare Disease: Review of a White Paper Proposal Find slides from prior workshops at www.everylifefoundation.org Morning Session 8:30 - 9:00 AM REGISTRATION AND BREAKFAST Introduction 9:00 AM Welcome, Brief Review of FDASIA, Draft White Paper & Overall Workshop Goals Emil Kakkis, MD, PhD President, EveryLife Foundation for Rare Diseases Session A: Challenges in Utilizing the Accelerated Approval Pathway 9:30 AM Factors that Should Enhance Rare Disease Treatment Access to Accelerated Approval Mark Thornton, MD, PhD, President, Sarcoma Foundation of America (SFA) 9:50 AM Assessing Benefit/Risk of Potential Treatments by Patients and Patient Groups Pat Furlong, President & CEO, Parent Project Muscular Dystrophy 10:10 AM Challenges in Qualifying Surrogates: FDA Perspective Marc Walton, MD, PhD Office of Translational Sciences, CDER, FDA 10:40 AM 11:00 AM DISCUSSION: Maximizing Reasonable Access to Accelerated Approval BREAK Can we do better developing treatments? Sly Disease has been successfully treated in animals but no children have ever been treated 5 The challenges for AA in Rare Diseases • Challenges in qualifying a surrogate to be “reasonably likely to predict clinical benefit” • Lack of prior clinical outcome & treatment data • Limited prior clinical studies or natural history • Difficult clinical biology not easily studied • Yet science and medicine may be solid and clear Key question: How do we practically qualify biomarkers for use with little prior clinical experience? In FDASIA (PDUFA V) US Congress Legislation: H.R. 4132: FAST Introduced By Rep. Stearns and Townes Better access to Accelerated Approval Pathway “Considerations. – In developing the guidance . . . . the Secretary shall consider . . . . for drugs designated for a rare disease or condition under section 526 of the Federal, Food, Drug, and Cosmetic Act; and (2) how to incorporate novel approaches to the review of surrogate endpoints based on pathophysiologic and pharmacologic evidence in such guidance, especially in instances where the low prevalence of a disease renders the existence or collection of other types of data unlikely or impractical.” 7 Workshop #5: Accel Approval in Rare Diseases Review of a White Paper Proposal At Workshop #4, created the plan • Draft set of criteria were considered • A working group was formed • White paper to consolidate recommendations for AA under FDASIA Work Shop #5 Key Goal • Review a proposed White Paper on recommendations for access and qualification considertions for AA RARE DISEASE WORKSHOP SERIES Improving the Clinical Development Process EVERYLIFE PROPOSED CRITERIA FOR QUALIFICATION OF A DISEASE/DRUG/BIOMARKER SET FOR ACCELERATED APPROVAL IN RARE DISEASES A) Disease Considerations Cause of disease clearly understood based on a measurable entity or single gene disorder Pathophysiology mechanisms relating to clinical disease/outcome reasonably understood Rare diseases with critical need for AA as plausible pathway: extremely high unmet medical need (lacking any current effective treatments with high morbidity and mortality), extreme rarity of the disorder or lack of any prior clinical studies, long time horizons for progression, disconnects between time of pathophysiologic damage and clinical expression, late diagnosis relative to the irreversible progression of disease, substantial clinical heterogeneity in a small population B) Drug Considerations Drug mechanism of action is direct and known Drug pharmacokinetics, pharmacodynamics and metabolism are relevant to the disease process being treated and can be accurately and readily measured Drug can be made reproducibly with appropriate quality to provide consistent effect C) Biomarker Considerations Biomarker has direct relationship to important disease cause and process Sampling compartment for biomarker predicts the important disease compartment/tissue Biomarker assay is a valid and reproducible: Sensitive, accurate, precise and specific with a sufficient dynamic range to calibrate change in biomarker with change in pathology Biomarker is a clinical physiologic assessment used in regular clinical practice for diagnosis and management D) Preclinical Considerations Magnitude/type of treatment effect is relevant and substantial relative to the human disease state Preclinical treatment studies show an appropriate dynamic dose-response relationship of the biomarker on pathophysiology and or clinical effect Preclinical studies show a meaningful clinical or physiologic effect on the disease if the models reflect human disease reasonably accurately Evaluation of alternative adverse effect pathways that are independent of efficacy that may mitigate or eliminate a determination of positive risk-benefit E) Clinical Considerations A cross sectional clinical study or retrospective medical chart survey of affected patients shows a relationship between severity/progression/disease level to a biomarker measure Comparable disease states based on similar biology or pathophysiology, if they exist, have supportive associations between a similar biomarker and relevant clinical benefit Absence of reliable or consistent clinical endpoints or extreme heterogeneity of important clinical evaluations provide few or no alternatives to AA 9 White Paper on AA in Rare Diseases Working Group Industry and Foundations Marc Boutin National Health Council Susan Boynton Shire HGT Mladen Bozic Shire HGT Gerald Cox Genzyme, A Sanofi Company Pat Furlong Parent Project MD Mark Hayes Synageva Emil Kakkis EveryLife Foundation for Rare Diseases Cori Leonard Ultragenyx Pharmaceutical Rachel Mack Vertex Pharmaceuticals Inc. Mary O'Donovan BioMarin May Orfali Pfizer Mark Thornton Sarcoma Foundation of America Jack Weet Seaside Therapeutics 10 Surrogate endpoint considerations • Prentice criteria: A set of mathematical criteria on how one variable represents another: not biological • Fleming (2005) reworked to focus on biological pathway issues – Direct measures versus parallel measures – Alternative unmeasured adverse pathways – Tiers of surrogates proposed Fleming concepts valid but not experimentally defined Need a practical implementation of concepts 11 Developing a scientific framework for for qualification of a biomarker for AA • Breakdown the surrogate endpoint analysis into individual specific scientific considerations – Disease, Drug, Biomarker • Better understanding of science at each level provides greater support for predictive value • Support the underlying science – Preclinical data and clinical supportive information • Find the balance of data that meets the standard “Reasonably likely to predict clinical benefit” 12 White Paper: Improving Scientifically Sound Access to the AA Pathway • Reviews the criteria for rare disease access – What factors should be considered in flexibility for AA as a pathway? • Defines Disease, Drug, BioMarker characteristics that enhance predictability • Defines preclinical and clinical data to support the qualification • Discusses Clinical Trial Design and Confirmatory studies 13 White Paper Table of Contents I. Introduction II. Background II. Considerations regarding the benefit-risk assessment IV. Scientific considerations for the qualification of biomarkers V. Summary considerations for qualification of a disease/drug/biomarker VI. Clinical trial design considerations VII. Conclusions VIII. References 14 Accelerated approval standard: Finding the balance in Benefit/risk • “A surrogate endpoint or clinical endpoint earlier than irreversible morbidity and mortality” that is “reasonably likely to predict clinical benefit” • What should set the standard for benefit-risk in rare diseases? – The disease matters: – Rarity, severity, biology, unmet need – Science behind the disease, endpoint and drug mechanism 15 1) Benefit-Risk Considerations Assessment should be evaluate the specific context of the disease, its rarity and other factors. • • • • • Extremely high unmet medical need Extreme rarity Absence of any prior clinical study or clinical data Slow or irreversible disease Significant delay between the onset of irreversible disease and clinical diagnosis • Lack of readily measurable clinical endpoints due to unusual clinical disease manifestations 16 2) Scientific Basis Considerations for a Disease/Drug/Biomarker Group Data in hand before extensive preclinical/clinical research • Disease considerations • Drug considerations • Biomarkers considerations 17 Scientific Context of Use for a Disease/Drug/Biomarker Set • A biomarker must be viewed in its context: – A disease mechanism connected to a certain drug action, leading to a biomarker result • The scientific relationship is critical to value as a surrogate • The group must be considered linked • Changing the drug mechanism or biomarker might not provide the same predictive value 18 DRUG BIOMARKER DISEASE MPS Disease/Endpoint/Drug Considerations 19 Scientific Data Considerations for a Disease/Drug/Biomarker Group Data developed from preclinical & clinical research • Preclinical research – Specific research data to support the relationships/validity of insights • Clinical data to support qualification – Cross-sectional survey – Natural history data – Other data 20 3) Clinical Study Data for Approval and for Post-marketing Confirmation • Adequate well-controlled studies • Pivotal study designs – Efficacy/biomarker – Safety • Placebo control – Alternative use of blinded evaluation – Natural history comparison 21 4) Post-marketing Confirmation • Requirements and challenges • Confirmatory study designs – Complexities – Alternative designs • Placebo and natural history controls • Withdrawal 22 Making AA practically assessable when it is the best choice for development • Predictable set of issues to collect and present at a pre-IND meeting – Need the opportunity early in development • Patient benefit-risk input via a sophisticated quality survey at the start – Provides the data on right benefit-risk choice • Early AA accessibility means more investment in more treatments Goals of today’s workshop • Discuss the elements of the guidance – Benefit/risk, Scientific qualification, Studies for approval, Confirmatory studies – Identify major omissions or issues that need to be resolved – Collect the major unresolved challenges for qualification • Provide examples for inclusion in the white paper • Build consensus of an improved document 24 Morning Session 8:30 - 9:00 AM REGISTRATION AND BREAKFAST Introduction 9:00 AM Welcome, Brief Review of FDASIA, Draft White Paper & Overall Workshop Goals Emil Kakkis, MD, PhD President, EveryLife Foundation for Rare Diseases Session A: Challenges in Utilizing the Accelerated Approval Pathway 9:30 AM Factors that Should Enhance Rare Disease Treatment Access to Accelerated Approval Mark Thornton, MD, PhD, President, Sarcoma Foundation of America (SFA) 9:50 AM Assessing Benefit/Risk of Potential Treatments by Patients and Patient Groups Pat Furlong, President & CEO, Parent Project Muscular Dystrophy 10:10 AM Challenges in Qualifying Surrogates: FDA Perspective Marc Walton, MD, PhD Office of Translational Sciences, CDER, FDA 10:40 AM 11:00 AM DISCUSSION: Maximizing Reasonable Access to Accelerated Approval BREAK