RRTC on Secondary Conditions in the Rehabilitation of Individuals
advertisement

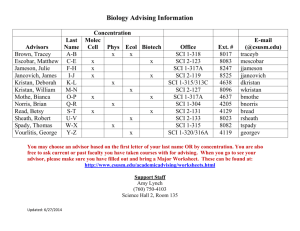
RRTC on Secondary Conditions in the Rehabilitation of Individuals with SCI Suzanne Groah, MD, MSPH Mark Nash, PhD Alexander Libin, PhD Jessica Ramella-Roman, PhD Manon Lauderdale, ABD NSCIA and ILRU RRTC Staff Center Director Suzanne Groah, MD,MSPH Emily Ward, MS Alexander Libin, PhD Miriam Spungen, BS Manon Inger Schladen Ljungberg, MPH (Lauderdale), MSE Eric Larson Jessica Romella-Roman, PhD, MSEE Alison Lichy, DPT Mark Nash, PhD Brenda Triyono, BS Cynthia Pineda, MD, FAAPMR Allen Taylor, MD Kurt Johnson, PhD Brenda Gilmore, BFA Mark Loeffler, MA Other Staff (Picture not available) Nawar Shara, PhD Patricia Burns, MS Eleutevio Ballwis, BSN Jasmine Martinez, DO Armando Mendez, PhD Tom Burnett, MS Sydney Jacobs, MA Robert Marsteller Katherine Westie, PhD Shannon Minnick Ms. Wheelchair Maryland ILRU Staff Laurie Gerken Redd Marj Elhardt Summary of Proposed RRTC • Research focus – Cardiometabolic risk and cardiovascular disease – Obesity – Pressure ulcers Summary of Proposed RRTC • Training focus – Consumers - focus on the underserved and nonEnglish speaking – Health care professionals - including nonrehabilitationists – State of the Science Importance of the Problem • Cardiovascular disease is a leading cause of death in long-term SCI – Overweight and obesity (especially around the abdomen) – Diabetes and pre-diabetes – High blood pressure – Abnormal cholesterol levels – Other – inflammation Importance of the Problem • Pressure ulcers (PU) are the most common medical complication in people surviving at least 1-year post injury • Frequency may be on the increase • Turning and repositioning recommendations are NOT supported by evidence • When PU’s occur in the hospital, they are now considered a “Never Event” Project R1: Cardiometabolic Risk, Obesity and Cardiovascular Disease in People with Spinal Cord Injury Principal Investigator (PI): Suzanne Groah, MD, MSPH Co-Principal Investigator (Co-PI) Mark Nash, PhD Project Coordinators: Emily Ward, MS (NRH) and Patricia Burns, MS (Miami) Background • Cardiometabolic syndrome is characterized by risk clusters • Risk clustering present in > 33% young, healthy paraplegics Background, con’t. • All of our knowledge of cardiovascular disease is from risk factors (cholesterol, etc) • But we don’t know whether obesity, abnormal cholesterol levels, diabetes or pre-diabetes actually leads to cardiovascular disease and “hard” endpoints • “Hard” endpoints for CVD include MI, cardiac death and stroke Objectives 1. Understand to what extent obesity, high blood pressure, diabetes, pre-diabetes, cholesterol, and inflammation lead to cardiovascular disease in people with SCI 2. Understand if there are certain risk factors that have greater importance in people with SCI 3. Develop an online cardiometabolic risk assessment tool (RISK) 4. Develop an adjusted BMI table for people with SCI R1 Methods R1 Testing - Carotid IMT • Shows atherosclerosis in the blood vessels leading to the brain • Related to future heart disease • Associated with high cholesterol levels R1 Testing - Carotid IMT • Associated with low good cholesterol (HDL-C) • Associated with diabetes and pre-diabetes • One study in people with SCI showed more atherosclerosis • Risk is underestimated by measurement of cholesterol levels R1 Testing - Coronary Artery Calcium (CAC) Scores • Atherosclerosis often has calcium deposits • Any calcium in coronaries = atherosclerosis • CAC scores directly correlate with – Atherosclerosis – Heart disease CAC and CT Angiography • But, CAC score alone may not fully reflect heart disease risk • Women and certain ethnic groups tend to not have calcium in heart • 1/10 with CAC score of 0 have noncalcified plaques CAC and CT Angiography • Non-calcified plaque most likely lead to heart disease • Calcified and noncalcified plaques • 1/5 radiation exposure SOME EARLY RESULTS Frequency of Risk Factors Risk Clustering Risk by BMI Category Subject 1 • Single 39yo African American Woman • Spinal Cord Injury: C6/C7 AIS B – Sense of touch maintained below neck – Loss of movement below neck – Due to car accident (9/1991) – Wheel Chair: Power Subject 1 cont. • Health History: – Non-Smoker – Family Hx: Pre-diabetes (father) • • • • Ht/Wt: 5 feet 10 inches, 171.3 pounds Resting Heart Rate: 70bpm Blood Pressure: 98/52 Framingham Risk Score: <1% 10-year risk of heart attack or death Subject 1 Body Fat • Body Fat Scan: – Total Body Fat: 50.4%; obese – Stomach Fat: 55.2% – Hip, Thigh, and Buttock Fat: 54.0% • BMI – 24.6 – “Normal” by general population tables – “Overweight” by SCI adjustment Subject 2 • Married 48yo Caucasian Woman • Spinal Cord Injury: C2 Sensory, C6 Motor AIS A – Loss of feeling below upper neck – Loss of movement below lower neck – Due car accident (7/1999) – Wheel Chair: Power Subject 2 cont. • Health History: – Non-Smoker – Muscle spasms/weakness, bed sores, under-active thyroid – Family Hx: heart disease, high blood pressure, high cholesterol, cancer – Surgical Hx: uterus removed (2006) • Ht/Wt: 5 feet 7 inches, 121.0 pounds • Resting Heart Rate: 62bpm • Blood Pressure: 78/51 • Framingham Risk Score: 1% 10-year risk of heart attack or death Subject 2 Body Fat • Body Fat Scan: – Total Body Fat: 37.3%; obese – Stomach Fat : 43.0% – Hip, Thigh, and Buttock Fat: 42.1% • BMI – 19.0 – “Normal” by general population guidelines – “Normal” by SCI adjustment Results – Blood Work Subject 1 Total Cholesterol (mg/dL) LDL (mg/dL) 118 64 Subject 2 206 136 Average Tetra* Recommended Value 171.67 Less than 200 Good 200-239 Not Good More than 240 Bad 108.71 Less than 100 Very Good 100-129 Good 130-159 Not Good 160-189 Bad More or equal to 190 Very Bad 42.10 Less than 40 Bad 40-60 Ok More than 60 Good HDL (mg/dL) 46 49 Total Cholesterol: HDL 2.57 4.2 Less than 4.5 Good More than 4.5 Bad 106 Less than 150 Good 150-199 Ok 200-499 Bad More or equal to 500 Very Bad TG (mg/dL) 38 94.92 * Groah SL, et al. Cardiometabolic risk in community-dwelling persons with chronic spinal cord injury. JCRP. (in press). Results – Blood Work Cont. Subject 1 Fasting Blood Sugar (mIU/mL) 78 Subject 2 80 Mean Tetra* Recommended Value 87.29 <100 Normal 100-125 Impaired ≥126 Diabetic 2 hour Blood Sugar (mIU/mL) 92 135 137.93 <140 Normal 140-199 Impaired ≥200 Diabetic Fasting Insulin (mIU/mL) 7.75 2.51 8.663 <20 Normal 2 hour Insulin (mIU/mL) 45.07 23.94 94.36 HbA1C (%) 4.8 5.3 5.13 hsCRP (mg/L) 4.2 5.1 IL-6 (pg/mL) 4.4 4.3 * Groah SL, et al. Cardiometabolic risk in community-dwelling persons with chronic spinal cord injury. JCRP. (in press). 4.4-6.4 Good <1 Good 1-3 Normal >3 Bad Summary Subject 1 BMI Body Fat % Blood lipids (fat) Inflammatory Markers 24.6 50.4% High Normal HsCRP: 4.2 High 37.3% High High Total Cholesterol and High LDLs HsCRP: 5.1 High Over weight Subject 2 19 Normal weight -Subjects have high body fat% regardless of body weight -Both Normal and High blood lipids (fat) found -Subjects have high levels of inflammatory markers Results - Imaging NRHR101 Right common carotid arteryanterior projection 13 Mean 0.627 mm Max 0.738 mm NRHR102 Right common carotid arteryanterior projection Normal CIMT Focal plaque seen in carotid artery CAC score 0 NRHR101 Cardiac CT: Coronary calcium and CT angiography Plaque quantitation: Curved MPR Thin cross sections RCA, thick MIP Oblique MPR- No plaque NRHR102 Incidental finding of thickened pericardium (noncalcified) History of pneumonia Project R2: Effect of an Omega-3 Supplement Intervention Program (OSIP) on Cardiometabolic Health in People with Spinal Cord Injury Principal Investigator (PI): Mark S Nash, PhD FACSM Co-Principal Investigator (Co-PI) Suzanne Groah, MD, MSPH Project Coordinators: Emily Ward, MS (NRH) and Patricia Burns, MS (Miami) Benefits of ω-3 Poly-Unsaturated Fatty Acids • Reduced death due to heart disease • Improved cholesterol levels – Triglycerides – Low density lipoprotein cholesterol • Reduced irregular heartbeats • Reduced inflammation • Reduced body fat Objectives • To determine whether ω-3 omega fatty acid supplementation can improve lipid (cholesterol) levels, inflammation, and body fat in people with chronic spinal cord injury (SCI) who have 2 or more cardiometabolic risk (CMR) factors. Methods • Multi-center double-blind RCT • Participants: 34 individuals, 18-65, from Project R1 • Participants must have multiple (i.e., 2+) of the CMRs – – – – Fasting TG> 150 mg/dL HDL-C < 40 mg/dL for males or < 50 for females hs-CRP > 3.0 Body fat (by DXA) >25% for males and 33% for females Methods • Procedures – Dietary Supplement and Placebo: • Ω-3 PUFA, 3.2 g EPA+DHA (EPA/DHA 3:1) vs. 4g Safflower seed oil – Blood Testing: • Administered at baseline (pre) and 3 months (post). • Testing for OGTT, lipid profile and inflammatory mediators as in R1 – Post-prandial Assessments (after a high fat meal) (0, 1,2,4,6 hrs): • Triglycerides • Inflammation • Whole body fat – Body Composition: DXA Training* Overview • • Overarching Objective: Translate findings of RRTC research to practice for both consumers and health care providers Supporting Objectives: 1. Define and present the state of knowledge about cardiovascular risk in people with SCI (systematic reviews) 2. Explore what knowledge and information formats and delivery mechanisms are most useful and acceptable to our consumer and clinician audiences 3. Build capacity to support the health and well-being of persons with SCI (consumer living, clinical practice, research discovery) * What we mean by “training” – Activities that promote understanding and application of the knowledge our RRTC will produce “Tight” Relationship Between Our Research and Training •Components of web-based tools •For both consumers and providers Systematic Review • Definition: a systematic study of existing research in an area of focus • Goal: to produce a document that can be used by clinicians and consumers to change practice • Focus of our systematic review: What is the cardiovascular risk profile of people with SCI? • Collaboration with University of Washington, Knowledge Translation Center Consumer-focused Objectives • To translate the knowledge generated by Research Projects R1, R2 in such a way as to help all persons with SCI practically integrate that knowledge in to their self-management practices – Goal is application not passive understanding • To exercise particular sensitivity to the learning circumstances, in terms of language, literacy and culture, of the underserved. – Making information understandable by people with low literacy satisfies people with high literacy as well (Nielsen, 2005) Clinician-focused Objectives • Increase awareness and knowledge of the key SCI secondary conditions of cardiometabolic syndrome and obesity • Promote – primary (before disease occurs), – secondary (screening to detect disease before it becomes symptomatic) and – tertiary (reducing disability and restoring function due to disease) prevention Current Activities: Exploring How People Engage With Information about SCI • Specifically for Consumers: – How do people find information about SCI? – What contexts (interests, circumstances, concerns) motivate people to look for information? – How do people like to get their information? In what formats? Through what mechanisms? – How do people appraise the quality of the information they receive? Consumers and SCI Information • Connecting through social media – YouTube, Facebook, Twitter • Website SCI-Health.org – Plain language, both English and Spanish – Interactive • Polls, information subscriptions, Help Desk “Follow Me” • First stop: http://sci-health.org • Second stop: http://www.youtube.com/user/HealthyTomorrow Current Activities: Exploring How People Engage With Information about SCI • Specifically for Clinicians: – What are the best approaches to teaching clinicians how to serve people with SCI (both in terms of applying best medical practice and in terms of interpersonal communication)? – What can we do to provide just-in-time information about SCI best practice at the point of care? Standardized Patients • Standardized patients (SPs): 3 flavors 1. Real people, simulate clinical symptoms, help clinicians train for real practice 2. SCI SPs also real people, with real SCIs, provide clinicians with more authentic training experiences 3. Virtual standardized patients (VPs), online, interactive • Currently exploring uses and limitations of SCI SPs – – – – • • Resource intensive Excellent for interpersonal learning Good (not excellent) for clinical skills learning – promising for teaching CVD risk assessment Limitations (e.g. can’t really simulate clinical emergencies) Experimentation with VPs to begin in fall 2010 Also exploring mannequin simulators Efforts Involving Both Consumers and From RRTC Clinicians in Use of Knowledge March 2010 Advisory Board Meeting Key point: The centrality of the person with SCI What can we do to promote the application of knowledge about CVD in SCI at the point of care? • Under exploration: Use of Personally Controlled Health Records (PCHRs) to bridge knowledge between people with SCI and their health care providers • What is a PCHR? – An electronic medical record that is managed by the consumer – Can include BOTH patient-specific and medical knowledge/information – May be “tethered” to a providers’ EMR or independent – Has the potential to import information from a variety of health sources • Providers’ records, pharmacy, data from devices such as home BP monitors – Consumers can edit or annotate the record to assure information is complete and correct PHCRs • Utility and Advantages – Can promote continuity of care • Persons with chronic conditions, who see multiple providers may benefit the most – Can be imported to a “smart card”, copied to a thumb drive or printed for sharing – Can be accessed by health care providers if patient is unconscious – Unlike EHRs, format is standardized and readable by browsers • Barriers – Privacy • Need to assure personal information remains confidential – Credibility • When is it appropriate for a provider to accept the assessment of another? • How does a provider know that the knowledge (best practices) presented are reliable? • To what degree is it good practice to allow consumers to control the information in their health records? • Can consumers actually be harmed by knowing certain information in their health records? – Accessibility • What technology is required of both consumers and providers to access and annotate the stored electronic records? RRTC Training Project Contacts • Director, consumer-focused projects – Alex Libin, PhD • Director, clinician-focused projects – Cindi Pineda, MD FAARM • Co-Director, both projects – Manon Schladen, MSE PMP EdS • Project Coordinator, both projects – Inger Ljungberg, MPH