ANTIMICROBIAL THERAPY
CHAPTER 13
Copyright © 2012 John Wiley &
Sons, Inc. All rights reserved.
Mad cow disease is caused by an “infectious” protein
se
50%
Fa
l
50%
Tr
ue
A. True
B. False
Mad cow disease-related death confirmed in TexasCNN) -- Mad cow disease has caused a
fourth death in the United States, health officials say.
Lab tests have confirmed that a patient in Texas who recently died had Variant CreutzfeldtJakob Disease. Variant CJD is a fatal brain disorder linked to eating beef from cattle with mad
cow disease, the Centers for Disease Control and Prevention said in a press release.
Variant CJD was first identified in the United Kingdom in 1996, according to the CDC. Worldwide
more than 220 cases have been reported, the majority in Europe. CDC officials said this is only
the fourth case to be reported in the United States, and that each U.S. infection is believed to
have happened while the patient was traveling abroad.
The Texan patient traveled "extensively" to Europe and the Middle East, the CDC said. Variant
CJD is different than what the CDC calls classic CJD, which is not related to mad cow disease.
Classic CJD strikes less than 400 Americans each year. It is also fatal.
Case of CJD confirmed in New Hampshire
Mad cow disease is officially called bovine spongiform encephalopathy, or BSE. Animals with
BSE have infectious prions in their brain, spinal cord and some parts of the central nervous
system. These prions can be spread to humans who eat those specific parts of the cow, or who
eat meat that has come in contact with infected tissue or that has been processed in
contaminated machinery.
Eating meat contaminated with the disease is thought to be the cause of Variant CJD in humans.
The first case of mad cow disease was confirmed in a cow in the United States in December
2003.
Drug-resistant TB may be treatable with new small molecule drug In a new study, scientists
report how a new small molecule drug appears able to kill drug-resistant tuberculosis without toxic
side effects. According to the World Health Organization (WHO), 9 million people around the world
fell ill with TB in 2013 and 1.5 million died of it. Improper use of antibiotics has led to new strains of
TB that are resistant to the two most powerful drugs used to treat it: isoniazid and rifampicin. Now,
researchers at the University of Georgia (UGA) in Athens have developed a new small molecule drug
that may serve as a treatment against multidrug-resistant TB that cannot be cured with conventional
drugs. "Multidrug-resistant TB is spreading rapidly in many parts of the world. There is a
tremendous need for new therapies, and we think our laboratory has developed a strong candidate
that disrupts fundamental steps in the bacterium's reproduction process."Dr. Nair and colleagues
were interested in one particular molecule - an enzyme that helps to produce TB RNA called RNA
polymerase, or RNAP. Without this molecule, the TB bacterium cannot produce the proteins it needs
to survive. The team developed a compound that interrupts the process through which RNAP
produces TB RNA. The compound - which they refer to as "Compound 2" in their paper - is a small
molecule that binds to specific amino acids and magnesium in the bacterial cells. The team was also
surprised - when carrying out early tests on the new compound - that it shows strong anti-HIV
properties. This could open the door to dual-purpose therapies, where the drug tackles more than
one disease at the same time.
A dual-purpose drug that tackles TB and HIV at the same time is a very exciting prospect because
the risk of developing TB is 26-31 times higher in people infected with HIV, according to the WHO.
Here we report a series of compounds containing a nitroimidazopyran nucleus that possess
antitubercular activity. After activation by a mechanism dependent on M. tuberculosis F420
cofactor, nitroimidazopyrans inhibited the synthesis of protein and cell wall lipid. We
conclude that nitroimidazopyrans offer the practical qualities of a small molecule with the
potential for the treatment of tuberculosis.
Breastfeeding may influence immune system development in early life A series of studies set to
be presented at the American Academy of Allergy, Asthma & Immunology's Annual Meeting in
Houston, TX, claim an infant's immune system development and susceptibility to asthma and
allergies may be influenced by a number of factors that shape what bacteria is in their gut,
such as gestational age at birth, breastfeeding and delivery by Cesarean section. "The immune
system is designed to be exposed to bacteria on a grand scale," she adds. "If you minimize those
exposures, the immune system won't develop optimally."Other studies have supported this
claim. In June 2014, for example, Medical News Today reported on a study published in the
journal Allergy and Clinical Immunology, in which researchers found exposing babies to bacteria
and allergens in the first year of life may reduce the risk of allergies, wheezing and asthma
later in life. he results of their analysis revealed that a mother's race/ethnicity, an infant's
gestational age at birth, prenatal and postnatal tobacco smoke exposure, the presence of pets in
the home and whether a baby was born via Cesarean section or vaginal delivery influenced an
infant's gut microbiome composition.
They also found that babies who were breastfed at 1 and 6 months had specific gut
microbiome compositions, compared with babies who were not breastfed, which the
researchers say may affect immune system development. In addition, babies who were
breastfed at 1 month were at lower risk of pet-related allergies. "The research is telling us that
exposure to a higher and more diverse burden of environmental bacteria and specific patterns
of gut bacteria appear to boost the immune system's protection against allergies and asthma."
CHAPTER 13 ANTIMICROBIAL THERAPY
The term chemotherapy was coined by Paul
Ehrlich to describe the use of chemical substances to kill
pathogenic organisms without injuring the host. Ehrlich
also coined the phrase “magic bullet” to describe
chemotherapeutic agents.
E-mail I received from Consumers Report (I subscribe to CR):
Dear Sheldon
Did you know that an antibiotic resistant strain of staph infection now kills an estimated 17,000 people
each year—and most people contract this infection during a stay in a hospital?
Hospitals know how to prevent the spread of these dangerous infections—good hand washing, isolation of infected patients, and use of
masks, gowns and gloves—but they haven't taken the necessary steps to make us all safe.
Tell your governor to direct hospitals in Kentucky to reduce the spread of these dangerous infections
And tell you which hospitals do the best job.
If you contract MRSA during a hospital stay, you are four times as likely to die, you will stay in the
hospital far longer than you planned, and your charges will triple, according to a recent study.
Some people who contract MRSA during their hospital stay live with it for years, undergo multiple
surgeries and are permanently disabled. These dangerous infections were once rare, but are now
epidemic.
Your governor can help! Tell your governor to make MRSA prevention a top priority in Kentucky
When you finish, be sure and forward this email to people in your address book who might also want to
help us prevent the spread of dangerous hospital-acquired infections.
Sincerely,
Jim Guest
President, Consumers Union of the U.S.
101 Truman Avenue
Yonkers, NY 10703-1057
\
Antibiosis- against life
antibiotic- coined by Selman Waksman, “a chemical
substance produced by microorganisms which has the
capacity to inhibit the growth of bacteria and even destroy
bacteria and other microorganisms in dilute solution.”
Synthetic drugs are agents synthesized in the
laboratory
Semi-synthetic drugs are antimicrobial agents made
partly by laboratory and partly by microorganisms
Bacteriocidal- killing
Bacteriostatic- growth inhibiting
Paul Erhlich- 1910 used salvarsan (heavy metal-arsenic
salt) to treat syphilis. Although salvarsan did not withstand
the test of time the concept of using a systemic “magic
bullet” did.
Gerhard Domagk and Ernest Fourneau (1935)discovered “sulfa” drugs (sulfonamides)
Alexander Fleming (1928) reported on his
observation with penicillin- but did not realize the magic
bullet possibilities
Ernst Chain (stumbled across Flemings research
paper) and Howard Florey - brought penicillin to it
“magic bullet” status. There was a great deal of money
available for research because the findings were directed
towards soldiers during WWII.
The combination of sulfonamides and penicillin
began the modern drug era.
Selective Toxicity- must harm the microbes without causing significant
damage to the host.
Therapeutic index- maximal tolerable dose per Kg body
weight, divided by the minimum dose per Kg body weight.
If the max= 8 and the min= 2- the therapeutic index = 4
If the max=6 and the min= 3 - the therapeutic index = 2
The top drug would be more effective and less toxic to the patient
than the bottom drug.
The therapeutic dose (also known as thetherapeutic ratio =
LD50 (lethal dose for 50% of the population)
ED50 (effective dose for 50% of the population)
is a very important number in studies of new drugs. If the therapeutic index is too low
(such as, Phase II studies) development of the drug will be discontinued.
“the active ingredient in popular over-the-counter analgesic Tylenol, also has a narrow
therapeutic range.” the active drug is acetaminophen. What does that statement mean to you?
Paracetamol (acetominophen) toxicity is the foremost cause of acute liver failure in the Western
world, and accounts for most drug overdoses in the United States, the United Kingdom, Australia
and New Zealand. (from wikipidea- with the appropriate references).
Penicillins fairly broad
spectrum
fairly broad spectrum
very broad spectrum
Narrow spectr.
Broad spectrum drugs, such as tetracycline, affect a variety of different organisms.
Narrow-spectrum drugs, such as isoniazid, affect only a few specific types of
organisms.
Fig. 13.1 the spectrum of antibiotic activity
You want to know the modes of action and examples
Fig. 13.2 The five major modes of action of antibacterial drugs
How penicillin inhibits cell wall synthesis
http://www.youtube.com/watch?v=4EJEr_lt5dM
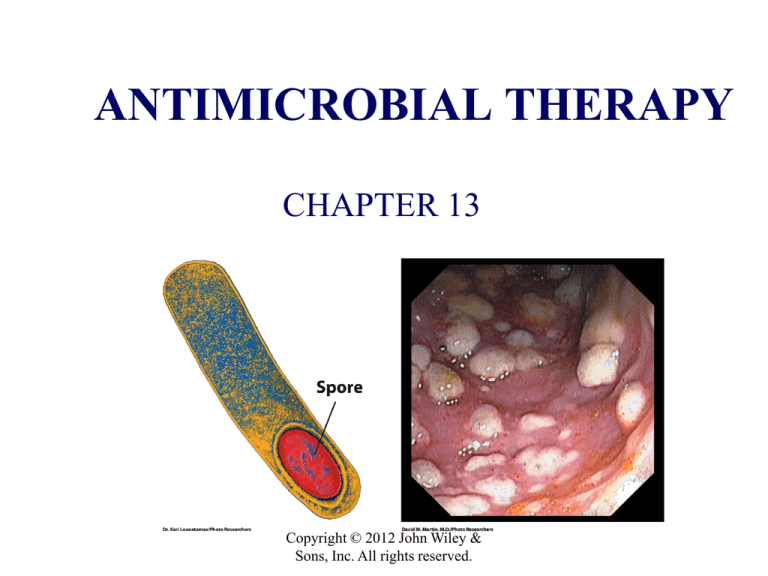
1. Inhibition of cell wall synthesis- Antibiotics such as
penicillin and cephalosporin contain a chemical
structure called a beta-lactam ring which interferes
with the cross-linking of the peptidoglycan (we will
see the structure when we discuss resistance- Figure
13-7.
Bacitracin is another antibiotic that blocks cell wall
synthesis- it block the basic synthesis of the cell wall
by blocking the movement of key wall components
from the cytoplasm through the membrane into the
wall.
Video below shows the mode of action of vancomycin
http://www.youtube.com/watch?v=UK7TaxmxOQ0
http://www.youtube.com/watch?v=Ov3G9GQo0fg&feature=relmfu
Spread of methicillin resistant Staphylococcus aureeus
2. Disruption of cell membrane function- certain
polypeptide antibiotics such as polymyxins act as
detergents and disorder bacterial membranes such that it
leaks and cannot carry out its function. Particularly active
against Gram negative organisms.
Polyene antibiotics, such as amphotericin B, bind to
particular sterols present in the membrane of fungi (and
animal cells) and do not act on bacteria (except
Mycoplasma) and polymyxins do not act on fungi.
http://www.youtube.com/watch?v=JzP2K60VDmc&feature=related
Amphotericin B liposome delivery system
3. Inhibition of protein synthesis. Differences between
bacterial (70S) and animal (80S) ribosomes allow
antimicrobial agents to attack bacterial cells without
significantly damaging animal cells-selective toxicity.
Aminoglycoside antibiotics, such as streptomycin, act on
the 30S portion of bacterial ribosomes by interfering with
the accurate reading (translation) of the mRNA message.
Chloramphenicol and erythromycin act on the 50S
portion of bacterial ribosomes, inhibiting the formation of
the growing polypeptide.
Antibiotics targeting ribosomes
http://www.youtube.com/watch?v=oC21vLFtsjo
http://www.youtube.com/watch?v=mM_HK3nSmsw&feature=relmfu
Streptococcus pneumoniae-Resistance to erythromycin
4. Inhibition of Nucleic acid synthesis- Differences
between the enzymes used by bacterial and animal cells
to synthesize nucleic acids provide a means for selective
action of antimicrobial agents. Antibiotics of the
rifamycin family bind to bacterial RNA polymerase
and inhibit RNA synthesis. This is due to the high
affinity of rifamycins to prokaryotic RNA polymerase.
5. Action as antimetabolites -Antimetabolites are
substances that affect the utilization of metabolites and
therefore prevent a cell from carrying out necessary
metabolic reactions.
Antimetabolites function in two ways:
1) by competitively inhibiting enzymes
2) by being erroneously incorporated
into important molecules such as nucleic acids.
Classic example of competitive inhibition is the
use of sulfanilamide which is structurally similar to paraaminobenzoic acid.
Developing resistance to sulfa drugs
http://www.youtube.com/watch?v=GpYMgwXoy7Y
Para-aminobenzoic acid (PABA)
PABA-is a metabolite in the synthesis of Folic Acid
para-aminosalicylic acid (PAS)
sulfanilamide
a) PABA (para-aminobenzoic acid) a metabolite required by many bacteria for the synthesis of folic acid among other
things b) sulfanilamide, a sulfa drug c) para-aminosalicylic acid (PAS) another competitive inhibitor or PABA. Animal
cells require folic acid (vitamin) and therefore their metabolism is not disturbed by these competitive inhibitors
Fig. 13.4 Competitive inhibition
Polyene antibiotics, e.g., amphotericin B, function by blocking
ergosterol synthesis in fungal membranes
se
50%
Fa
l
50%
Tr
ue
A. True
B. False
Parkinson's trial suggests growth factor has regenerative effects in brain The first trial to test
the effect of a growth-factor compound in humans with Parkinson's disease has shown
promising results. A report in the Journal of Clinical Investigation raises the hope that one day
we will see regenerative treatments for Parkinson's disease that use the brain's own protective
mechanisms to halt the loss of brain cells and restore dopamine levels. Research into the effects
of platelet-derived growth factor or PDGF started over 10 years ago with studies in animals.
These found that the growth factor reduces symptoms of Parkinson's, improves motor skills,
and restores levels of dopamine in the brain. They also suggest PDGF repairs neurons and nerve
fibers. he treatment - PDGF or placebo - was delivered via a pump surgically implanted in the
abdomen, with an internal catheter that went up into the brain. The pump delivered the drug
for 12 days, and patients were followed for another 73 days, during which the pump delivered
an infusion of saline. The results show that PDGF does not cause serious, unresolvable side
effects. The researchers were also encouraged by other results, which they discovered when
they examined PET scans of the patients' brains taken 4 months after treatment.
The PET scan images showed that in the patients who received the active treatment - as
opposed to placebo - levels of dopamine signaling were not only maintained, but even
increased. "Although we still have a long way to go our study suggests that it may be possible
to stimulate the brain's built-in protective mechanisms in order to slow or halt disease
progression."
Peptide developed that may slow Parkinson's disease New research suggests
it may be possible to slow the progression of Parkinson's disease using a manmade peptide that stops the formation of faulty protein fibrils that kill the
brain cells that produce dopamine. The main reason behind the death of
dopamine-producing cells in patients with Parkinson's disease is thought to
be a fault in a common cell protein called α-synuclein. When faulty, the
protein forms the wrong shape and clumps into long toxic fibrils that stop the
cells functioning properly. Now, a new study - funded by Parkinson's UK and
led by the University of Bath in the UK - shows how a peptide they designed
may offer a way to slow the progression of Parkinson's disease. In this study,
the researchers found that their peptide sticks to misshapen α- synuclein and
stops it stacking into the fibrils that kill off the dopamine cells. The peptide
matches a region of α-synuclein that is mutated in Parkinson's
To make their peptide - which comprises 10 amino acids - the team searched a
library of peptides for candidates that match the region of α-synuclein that is
mutated in patients with early-onset Parkinson's. In their paper, the team
notes that the technique may also apply to other neurodegenerative diseases
like Alzheimer's disease, which also arises as a result of misshapen proteins
clumping together in the brain.
Pyrimidine
Purine
Vidarabine
idoxuridine
Antimetabolites such as the purine analogue vidarabine and the pyrimidine analogue
idoxuridine are erroneously incorporated into nucleic acids. Vidarabine is an anti-viral drug which
is active against herpes simplex and varicella zoster viruses. Idoxuridine is an herpesvirus antiviral drug.
Fig. 13.5 Base analogues
Kinds of side effects
Side effects of antimicrobial agents on infected persons fall into
three general categories: 1) Toxicity, 2) allergy and 3) disruption of normal
microflora.
1) toxicity- some antibiotics exert toxic effects on the host (will discuss
as we deal with the individual antibiotics).
2) Allergy- An allergy is a condition in which the bodys’ immune
system responds to a foreign substance, usually a protein. Allergic reactions
can be limited to mild skin rashes or they can be life-threatening. Breakdown
products of penicillins can combine with proteins in the body to trigger an
anaphylactic type reaction which is life threatening.
3) Disruption of normal microflora- long term use of penicillins or
aminoglycosides can abolish natural microbiota and allow colonization of
the gut with resistant Gram negative bacteria, Clostridium difficile (very
common and nasty Inflammatory bowel disease) and fungi such as Candida.
Oral and vaginal superinfections with species of Candida yeasts are common
after prolonged use of antimicrobial agents such as cephalosporins, tetracyclines,
and chloramphenicol.
The Resistance of Microorganisms-resistance of a
microorganism to an antibiotic means that a microorganism
formerly susceptible to the action of the antibiotic is no
longer affected by it.
How resistance is acquired
Microorganisms generally acquire antibiotic resistance by genetic
changes, but sometimes they arise by nongenetic means.
Resistance of the latter sort occurs when organisms evade antibiotics by remaining out
of reach. TB in the lungs and sometimes E. coli in the urinary tract.
.
Another type of resistance is the shift to L forms that lack most of their cell walls (Lforms are typically derived from Gram negative bacteria and similar to
spheroplasts)
Genetic resistance to antimicrobial agents develops from genetic changes
followed by natural selection. In most bacterial populations mutations occur
spontaneously at a rate of approx. 1 in 107 to 1 in 1010.
Because bacteria multiple so rapidly it is easy to have 1010 cells and so there
will typically be a number of resistant cells in a population of bacteria.. If the resistant
organism is in an environment in which the antibiotic is present its progeny will have a
selective advantage such that after a number of generations it will be the predominant
organisms. Antibiotics do not induce mutations but they create an environment in which
resistant organisms predominate (such as seen in the fluctuation test (repeated on the
next slide).
Genetic resistance can be due to changes in the bacterial chromosome or
to extrachromosomal material.
There are basically five mechanisms associated with bacterial resistance to
antibiotics:
1. Alteration of targets- the target protein is changed due to
mutation. Resistance to erythromycin, rifamycin and antimetabolites has
developed by this mechanism.
2. Alteration of membrane permeability- antibiotic can no
longer cross the membrane or is transported out of the cell- In bacteria,
resistance to tetracyclines, quinolones and some aminoglycosides has
occurred by this mechanism.
3. Development of enzymes that destroy or inactivate the
antibiotic. One enzyme of this type is beta-lactamase which breaks the betalactam ring of penicillin and some cephalosporins. Similarly, enzymes can
destroy various aminoglycosides and chloramphenicol.
4. Alteration of an enzyme- that works better with the
substrate than the antibiotic. Example is with sulfonamide-resistant
bacteria. These organisms have developed an enzyme that has a very high
affinity for PABA and a very low affinity for sulfonamide.
5. Alteration of a metabolic pathway- This mechanism bypasses a reaction inhibited by an antimicrobial agent. A good example is 4.
Cross-resistance- is resistance to two or more similar
antimicrobial agents via a common mechanism. The
action of beta-lactamase against penicillin and
cephalosporin is an example.
How penicillin and vancomycin inhibits cell wall synthesis- already seen
Above already seen
Fig. 13.7 The effect of b lactamase on penicillin
How to Limit drug resistance1) high levels of an antibiotic can
be maintained in the bodies of patients long
enough to kill all pathogens, including
resistant mutants, or to inhibit them
sufficiently such that the host defenses can
get rid of them
Fig. 13.8 Effects of premature termination of antibiotic treatment
2) Two antibiotics can be administered simultaneously
so that they can exert an additive effect termed synergism.
For example, when streptomycin and penicillin are
combined in therapy, the damage to the cell wall caused
by the penicillin allows better penetration by
streptomycin.
When clavulanic acid and a penicillin called
amoxicillin are given together the clavulanic acid binds
tightly to beta-lactamase and prevents the enzyme from
inactivating the amoxicillin, i.e., clavulanic acid inhibits
penicillinase (beta-lactamase).
3) limiting antibiotics to essential uses only. Restrict the
use of antibiotics to cases with bacterial infections. Restrict
the use of antibiotics in hospitals. In addition, ban the use
of antibiotics in animal feeds.
Why are there so few clinically useful antibiotics?
Several hundreds of compounds with antibiotic activity have been
isolated from microorganisms over the years, but only a few of them
are clinically useful. The reason for this is that only compounds with
selective toxicity can be used clinically - they must be highly effective
against a microorganism but have minimal toxicity to humans. In
practice, this is expressed in terms of the therapeutic index - the ratio
of the toxic dose to the therapeutic dose. The larger the index, the better
is its therapeutic value.
DETERMINING MICROBIAL SENSITIVITES TO
ANTMICROBIAL AGENTS.
The disk diffusion method.
Disc contains a set amount
of antibiotic.
Circumference of the zone
of clearing is compared to
standards to determine the
effectiveness of the
antibiotic against the test
organisms. Size of zone of
clearance not necessarily
indicative of one
antibiotic being more
effective than another
(because the diffusion
rates of the antibiotics
vary).
Minimal inhibitory concentration (MIC) microbial
susceptibility testing. Organism is sensitive to all
but Penicillin R. Most sensitive to methicillin and
cefotaxime.
Fig. 13.9 The disk diffusion method of
determining microbial sensitivities to various
antibiotics
Each lollipop is
saturated with a
different
antibiotic or it
can be different
concentrations of
an antibiotic
Organism showing resistan
This test determines antibiotic
sensitivity and estimates minimal
inhibitor concentration (MIC). A
plastic strip containing an
increasing gradient of a given
antibiotic is placed on the surface of a
Petri dish which has been swabbed with
the bacterial organism of interest. A
zone of inhibition of growth around the
strip indicates sensitivity of the
organism to that specific antibiotic.
The point a which inhibition begins
indicates the MIC (minimal
inhibitory concentration) for that
antibiotic, and can be read off the
printed scale.
Fig. 13.10 An E (epsilometer) test.
Antibacterial agents
Penicillin and cephalosporin
block cross-linking of
pentaglycine bridge
pentaglycine cross-link bridge
tetrapeptide starts
Basic structural unit of the
as a pentapeptide
as shown in the
figure to the right
View the videos
In previous slides
For the action of the
Beta-lactam antibiotics
peptidoglycan
D-ala
This D-ala is cleaved during cross-linking
Basic building block of peptidoglycan
How Vancomycin inhibits cell wall synthesis
http://www.youtube.com/watch?v=UK7TaxmxOQ0
Cephalosporin works essentially the same way as penicillin
a) A comparison of the penicillin and cephalosporin molecules with beta-lactam rings
b)Cephalosporins differs slightly in the attached ring and has two sites for side -chain
attachments rather than one, as on the penicillin molecule
Fig. 13.11 Basic structure of penicillin and cephalosporin
Need not memorize the
different R groups of
penicillin just wanted to give
you some idea of the
structural differences among
the different types of
penicillin and Cephalosporins
You do not have to know
the varous types of
penicillins.
Figure 13 bottom
Additional Beta-lactam antibiotics:
Carbapenems represent a relatively new group of bactericidal antibiotics with a two-part
structure.
Example- Primaxin:
Imipenem/cilastatin is a broad spectrum beta-lactam antibiotic containing equal quantities
of imipenem and cilastatin.
Imipenem, the active antibacterial agent, is rapidly degraded by the renal enzyme
dehydropeptidase if administered alone (making it less effective). It is a cell wall antibiotic
Cilastatin is a dehydropeptidase inhibitor, with no intrinsic antibacterial activity,
and must be co-administered with imipenem to ensure its efficacy. Cilastatin blocks the
effects of the renal enzyme. Cilastatin has no antibacterial effects and does not affect the
antibacterial activity of the imipenim. This drug is given by injection or infusion and is
generally used to treat severe infections. It may be less likely to cause an allergic reaction in
people who have had an allergic reaction to a penicillin in the past.
Other antibacterial agents that act on cell walls
Bacitracin a small bactericidal polypeptide derived from Bacillus
licheniformis, is used only on lesions and wounds of the skin or mucous
membranes because it is poorly absorbed and toxic to the kidneys. This
antibiotic prevents the transfer of the peptidoglycan building block
synthesized within the cell from going through the plasma membrane
to the outside of the cell.
Vancomycin- Can be used to treat infections caused by methicillinresistant staphylococci and enterococci. Because it is poorly absorbed
through the GI tract, it must be administered intravenously.
Vancomycin prevents incorporation of N-acetylmuramic acid (NAM)- and Nacetylglucosamine (NAG)-peptide subunits into the peptidoglycan matrix;
which forms the major structural component of Gram-positive cell walls.
Vancomycin binds to the D-alanyl-D-alanine moieties of NAM/NAG peptides and
blocks cross-linking.
Polymyxin mode of action:
1.Alters cytoplasmic membrane permeability by binding to
a negatively charged site in the lipopolysaccharide layer
which has an electrostatic attraction for the positively
charged amino groups in the cyclic peptide portion
2.Fatty acid portion dissolves in hydrophobic region of
membrane and disrupts membrane integrity
3.Leakage of cellular molecules, inhibition of cellular
respiration
4.Binds and inactivates endotoxin (LPS)
5.Relative absence of selective toxicity: nonspecific for cell
membranes of any type, highly toxic
Active ttuberculosis will kill about two of every three people
affected if left untreated. Treated tuberculosis has a mortality rate
of less than 5%.
The standard "short" course treatment for tuberculosis (TB), is
isoniazid (inhibits mycolic acid-major cell wall component), rifampicin
(inhibits RNA polymerase), pyrazinamide (thought to disrupt membrane
structure and interfere with energy metabolism), and ethambutol (blocks
the formation of the cell wall of the tuberculosis organism), for two
months, then isoniazid and rifampicin alone for a further four months.
The patient is considered cured at six months (although there is still a
relapse rate of 2 to 3%). For latent tuberculosis, , the standard treatment
is six to nine months of iisoniazidalone.
If the organism is known to be fully sensitive, then treatment is with
isoniazid, rifampicin, and pyrazinamide for two months, followed by
isoniazid and rifampicin for four months. Ethambutol need not be used.
Acyl lipids
lipoarabinomannan (LAM)
Mycolic acid
arabinogalactan
peptidoglycan
Lipid bilayer
The complex structure of the acid fast
cell wall makes it a good barrier against
many physical agents, such as phagocytic
cell digestion, penetration by
antibacterial agents. However, the
treatment in the slide above, combination
of drugs described in the previous slide,
seems to be very effective against TB.
Mycobacterium tuberculosis (TB organism is an acid fast organism )
Fig. 4.6c-Acid fast cell wall
Inhibitors of protein synthesis
You do not need to memorize any of the
antibiotic producing organisms.
Aminoglycosides (irreversibly binds to the 16S subunit of
the 30S ribosome)- An important property of this class of
antibiotics is its ability to act synergistically with other
antibiotics.
binds here
30s sub-un
For example, gentamicin (an aminoglycoside) and penicillin
or ampicillin are effective against penicillin-resistant
streptococci.
Some examples: gentamicin, kanamycin, neomycin, and
streptomycin.
Tetracyclines (Also binds to the 16S subunit of the 30S ribosome)
Some examples: i) tetracycline ii) chlortetracycline (aureomycin) and
oxytetracycline (terramycin)
Newer semisynthetic teteracyclines include minocycline and
deoxycycline.
All are bacterostatic (reversibly bind to the 30S ribosome) at
normal doses, are readily absorbed from the digestive tract, and
become widely distributed in tissues and body fluids. The fact that
tetracyclines have the widest spectrum of activity of any antibiotics
30S subunit
(Gram positives, Gram negative, rickettsia, mycoplasma and some fungal
infections) both beneficial and a problem:
i) produce severe gastrointestinal disorders because they destroy so
much of the normal flora
ii) recalcitrant superinfections of tetracycline-resistant Proteus,
Pseudomonas and Staphylococcus as well as yeast infections, also can
result. Also Clostridium difficile infection of the GI tract
Chloramphenicol- Chloramphenicol binds to the 50Sribosomal subunit and blocks translation. Chloramphenicol is now
fully synthesized in the laboratory. Like
tetracyclines it is
bacteriostatic, is rapidly absorbed from the digestive tract, is
widely distributed in tissues, and has a broad spectrum of activity.
It is used to treat typhoid fever, infections due to penicillin-resistant
strains of meningococci and Haemophilus influenzae, brain
abscesses and severe rickettsial infections.
However, it is used sparingly because it can cause aplastic anemia
(body stops producing red and white blood cells in sufficient quantity)in a dose-dependent manner- which is often a fatal disease. Aplastic
anemia appears days to months after treatment is discontinued and
is most common in newborns.
Other antibacterial agents that affect protein synthesis
macrolides- Erythromycin Binds to the 50S ribosomal
subunit and blocks translation.
A commonly used macrolide (large ring compound) is
produced by several strains of Streptomyces erythreus and
exerts a bacteriostatic effect.
It is recommended for infections caused by streptococci,
pneumococci, and corynebacteria but is also effective
against Mycoplasma, Chlamydia, and Campylobacter.
Several antibiotics are effective against pneumonias,
however, erythromycin
is the only common
antibiotic that will combat Legionnaires’
disease.
Inhibitors of Nucleic Acid Synthesis
Rifampin- produced by Streptomyces mediterranei, only the
semisynthetic rifampin is currently used. Easily absorbed from the
digestive tract except when taken directly after a meal, it reaches all
tissues and body fluids. Although it is bactericidal and has a wide
spectrum of activity, it is approved in the US only for treating
tuberculosis and eliminating meningococci from the nasopharynx
of carriers. Rifampin blocks RNA transcription.
Quinolones- inhibit bacterial DNA synthesis by blocking DNA
gyrase a new group of synthetic bactericidal analogues of nalidixic
acid, are effective against many Gram-positive and Gram-negative
bacteria. Quinolones’ mode of action is to inhibit the enzyme
that unwinds the DNA double helix preparatory to its
replication. Norfloxacin, ciporofloxacin and enoxacin are
examples of this group of antibiotics.
Antifungal Agents are being used with greater frequency because of the emergence of
resistant strains and an increase in the number of immunosuppressed patients, especially those with AIDS.
Imidazoles and Traizoles They appear to affect fungal plasma membranes by
disrupting membrane sterols.
Several agents in this family of drugs are currently in use: clotrimazole, ketoconazole, miconazole, and
fluconazole. All these agents are used topically.
Polyenes the polyene family of antibiotics consists of antifungal agents that contain at least two
double bonds. Amphotericin B (and Ampho E) and nystatin are two of the most
common polyene antibiotics. Amphotericin B increases membrane permeability such that
glucose, potassium and other substances leak from the cell. This drug binds to membrane
ergosterol found in fungi and some algae and protozoa but not in humans The drug is poorly absorbed
by the GI tract and is given intravenously.
Amphotericin B (and E) is the drug of choice in treating most systemic fungal
infections, especially cryptococcosis, coccidioidomnycosis, and aspergillosis.
Nystatin has the same mode of action as amphotericin B but is also effective topically in the treatment of
Candida yeast infections.
Griseofulvin-originally from Penicillium griseofulvum, is used primary for superficial fugal infections.
The drug binds to tubulin, interfering with microtubule function, thus inhibiting mitosis.
General mechanism of action of amphotericin B
Do not have to know these structures. Only that that Amphotericin B and
Nystatin are polyene antiobiotics
superficial fungal infections
e.g., athletes foot
Polyene antibiotics (ene= double bonds)
Amphotericin B and Nyastatin are membrane disrupters but unlike what your
book shows they have different structures (as shown above).
Antifungal antibiotics
Antiviral Agents:
Purine and pyrimidine analoguesIdoxuridine and trifluridine, both analogues of thymine, are administered in eye drops to treat
inflammation of the cornea caused by a herpesvirus. They block DNA replication.
Vidarabine (ARA-A)- an analogue of adenine, has been used effectively to treat viral encephalitis, an
inflammation of the brain caused by herpesviruses and cytomegaloviruses. Also blocks DNA
synthesis.
Ribavirin (Virazole), a synthetic nucleotide analogue of guanine, blocks replication of certain
RNA and DNA viruses. Ribavirin blocks RNA replication in RNA viruses, how it blocks
DNA virus replication is less clear. In an aerosol spray, it can combat influenza viruses; in an
ointment, it can help to heal herpes lesions. In the U.S. the oral (capsule or tablet) form of
ribavirin is used in the treatment of hepatitis C, in combination with interferon drugs
Acyclovir- (Zovirax) analogue of guanine (Blocks HSV DNA synthesis by competing
with HSV thymidine kinase), is much more repeatedly incorporated into virus infected cells
than into normal cells. Thus, it is less toxic than other analogues. It can be applied topically or
given orally or intravenously. It is especially effective in reducing pain and promoting
healing of primary lesions n a new case of genital herpes.
Ganiciclovir is an analogue of guanine similar to acycovir. The drug is active against several
kinds of herpesvirus infections and in particular cytomegalovirus eye infections.
Amantadine- The tricyclic amine amantadine prevents influenza A viruses from penetrating
cells.. In terms of the mechanism of its antiviral properties, amantadine interferes with a
viral ion channel which is required for the viral particle to become "uncoated" once it is
taken inside the cell by endocytosis.
Chloramphenicol can cause aplastic anemia, a deadly form of
cancer
se
50%
Fa
l
50%
Tr
ue
A. True
B. False
Neuraminidase required for release of influenza virus from the cell surface
Mode of Action of Tamiflu- neuraminidase inhibitor
Fig. 13.17 the use of double antibiotic therapy to eradicate resistant-strain
infections