Breaking Bad News - mcstmf
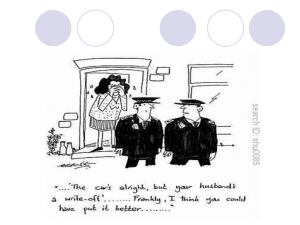
advertisement

Breaking Bad News Objectives: Students will: • Recognize essential principles of breaking bad news. • Identify pitfalls in delivering breaking bad news. • Apply skills of breaking bad news in a simulated situation. THE BAD NEWS ABOUT BREAKING BAD NEWS IS THAT BAD NEWS IS BAD NEWS DEFINITION OF BAD NEWS Bad News any news that drastically and negatively alters the patient’s view of their future Buckman R. BMJ1984 Bad News any news that drastically and negatively alters the patient’s view of their future Buckman R. BMJ 1984 Bad News any news that drastically and negatively alters the patient’s view of their future Buckman R. BMJ 1984 It alters one’s self-image : “I left my house as one person & came home another.” Professional cyclist Lance Armstrong’s recollection Examples of Conditions Requiring Breaking of Bad News ???!!!! Examples of Conditions Requiring Breaking of Bad News • Cancer related diagnoses • Intra uterine foetal demise • Life long illness: Diabetes, Epilepsy • Poor prognosis related to chronic diseases: loss of independence Examples of Conditions Requiring Breaking of Bad News(cont) • Informing parents about their child’s serious mental/physical handicap • Giving diagnosis of serious sexually transmitted disease …catastrophic psychosocial results • Non clinical situations like giving feedback to poorly performing trainees or colleagues The Good News! about Bad News!!! • Using a plan for determining the patient’s values, their wishes for participation in decision making, and a strategy for addressing their distress when the bad news is disclosed can increase our confidence in the task. The Good News! about Bad News!!!(cont) • It may also encourage patients to participate in difficult treatment decisions • Those who do so have a better quality of life • Clinicians who are comfortable with giving bad news are subject to less stress and burnout. عن أبي يحي صهيب بن سنان رضي هللا عنه قال: قال رسول هللا صلى هللا عليه وسلم: (( عجبا ألمر المؤمن إن أمره كله له خير وليس ذلك إال للمؤمن :إن أصابته سراء شكر فكان خيرا له ،وإن أصابته ضراء صبر فكان خيرا له)) رواه مسلم Do You Tell?? Do You Tell? Recent studies have shown that: • Patients generally (50-90%) desire full & frank disclosure, though a sizeable minority still may not want the full disclosure. (Ley p. Giving information to patients. New York: Wiley, 1982 ) So the issue is not “do you?” Issue is “how?” Do You Tell? In reality, patients who are dying, know they are dying They want confirmation of their status They want a time frame YOU would want a time frame when your time approaches Is this Difficult to break the bad news? WHY? Is this Difficult to break the bad news? • It is referred by some physicians like “dropping the bomb” Baile W F, oncologist 2000 Why is this Difficult? Social factors Our society values youth, health, wealth Elderly, sick and poor are marginalized Sick and dying have less social value Why is this Difficult? Physician factors Fear of causing pain Uncomfortable in uncomfortable situations Sympathetic pain due to patient’s distress Why is this Difficult? Fear of being blamed Physicians have authority, control, privilege and status When medical care fails patient it’s physician’s fault “blame the messenger” Why is this Difficult? Fear of therapeutic failure Medical system reinforces idea that poor outcome and death are failures of ‘system’ and by extension, our failure “all disease is fixable” “better living through chemistry” We are trained to feel this way; “if only……” Why is this Difficult? Fear of medico-legal system Everyone has “right” to be cured; If no cure happens, someone is to blame Why is this Difficult? Fear of not knowing “we don’t do what we don’t do well” Good communication is a skill that is not highly valued, therefore not taught Why is this Difficult? Fear of eliciting reaction “don’t do anything unless you know what to do if it goes wrong” Not trained to handle reactions Not trained to allow emotion to come out Why is this Difficult? Fear of saying “I don’t know” We are never rewarded for lack of knowledge Can’t know or control everything Why is this Difficult? Fear of expressing emotions Viewed as unprofessional Suppressing emotions increases distance between ourselves and patients Rabow & Mcphee (West J. Med 1999) described: “Clinicians focus often on relieving patients’ bodily pain, less often on their emotional distress & seldom on their suffering.” Why is this Difficult? Ambiguity of “I’m sorry” Two meanings “I’m sorry for you” “I’m sorry I did this” Easily misinterpreted Why is this Difficult? Fear of one’s own illness and death Cannot be honest with the dying unless you accept you will die So How Do We Do This?? Never, never, never, ever… NEVER “assume” If you need to know something If you want to know something If you need to know something If you want to know something ASK!! THINGS GO WRONG WHEN: * WE TRY TO ESCAPE * WE REACT IN ANGER * WE DILUTE THE AGENDA THINGS GO WRONG WHEN: WE TRY TO ESCAPE: • • • • • • INAPPROPRIATE DELEGATION DISTRACTION FRONTAL ATTACK INTELLECTUALIZATION MINIMIZATION EMPTY REASSURANCE THINGS GO WRONG WHEN: WE REACT IN ANGER: • • • • • TO DENIAL TO IDEALIZATION TO REHEARSAL OF THE STORY TO ‘UNREASONABLE’ DEMANDS TO ANGER AND BLAME THINGS GO WRONG WHEN: WHEN WE DILUTE THE AGENDA: • BILLING • PRACTICAL ARRANGEMENTS • REQUEST FOR POST MORTEM The SPIKES Protocol • SETTING UP the interview • Assessing patient’s PERCEPTION • Obtaining the patient’s INVITATION • Giving KNOWLEDGE and information • Addressing the patient’s EMOTIONS • STRATEGY and SUMMARY SPIKES Step 1: S - SETTING UP the interview • Preparation Preparation- Preparation • Always in person, face to face NEVER on telephone • Plan, arrange for privacy, involve significant others • Sitting down, Non Verbal Behaviour • Manage time constraints and interruptions SPIKES • Step 2: P – Assessing The PATIENT’S PERCEPTION • Gather before you Give • Patient’s knowledge, expectations and hopes • What do they understand about the situation? Unrealistic expectations? • What is their state of mind? Hopes? • Opportunity to correct misinformation and tailor your information SPIKES • Step 3: I – Obtaining the patient’s INVITATION • Gather before you give • How much does the patient want to know? Coping strategy? • Answer questions, offer to speak to another SPIKES • Step 4: K – Giving KNOWLEDGE and information to the patient • • • • • • • • Warning shot Use simple language, no jargon, Vocabulary and comprehension of patient Small chunks, avoid detail unless requested Pause, allow information to sink in Wait for response before continuing Check understanding Check impact SPIKES • Step 5: E – Addressing the patient’s EMOTIONS with empathic responses • Shock, isolation, grief • Silence, disbelief, crying, denial, anger • Observe patient’s responses and identify emotions • Offer empathic responses Emotions of the patient • Respond to patients’ emotions with empathy • Often shock, isolation, disbelief, grief or anger Observe for emotion on patient’s part Identify the emotion. Identify the reason for the emotion Connect with the patient Emotions of the patient • Exploratory questions How do you mean? Tell me more about it You said it frightens you You said you were concerned about your children, tell me more Could you tell me what you are worried about? Emotions of the patient • Validating responses I can understand how you felt that way I guess anyone might have the same reaction You are perfectly correct to think that way Your understanding of the reason for the tests is very good Many other patients have had a similar experience Emotions of the patient • Doctor: “I’m sorry to say that the X-ray shows that the chemotherapy is not working [pause]. Unfortunately, the tumor has grown somewhat” • Patient: “I’ve been afraid of this!” [Cries] • Doctor: [Moves his chair closer, offers the patient a tissue and pauses,] “I know that this isn’t what you wanted to hear. I wish the news were better” What is Empathy? The capacity to recognise emotions that are being felt by another person. Empathic Responses • An indication to the patient that you recognise what they are feeling (and why) • Verbal and Non verbal • Often associated with the impact of the news rather than the understanding. • Wait for response • Clarify Emotions of the patient Empathic statements I can see how upsetting this is to you I can tell you were not expecting to hear this I know this is not good news for you I’m sorry to have to tell you this This is very difficult for me also I was also hoping for a better result SPIKES • Step 6: S – STRATEGY and SUMMARY • Are they ready? • Involve the patient in the decision making • Check understanding • Clarify patient’s goals • Summarise • Contract for future REVISION OF THE 6 STEPS Six Step Protocol -arrange physical context -find out what patient knows -find out what patient wants to know -share information -respond to patient’s feelings -plan follow-through Arrange physical context Always in person, face to face NEVER on telephone Assure privacy Verify who is present Verify who should be present ASK Arrange physical context Remove physical barriers Sit down patient-physician eyes at same level appear relaxed, not casual (avoid ‘open 4’) Touch patient (appropriately) above the waist, handshake, shoulder Find out what patient knows Not just knows, but understands Use open questions closed questions excellent for historytaking prevent discussion Find out what patient knows Listen effectively to response: tells understanding, ability to understand Repeat back what patient says Do not interrupt Make encouraging cues Maintain eye contact Find out what patient knows Tolerate silences Listen for “buried question” question asked while you are speaking Find out what patient wants to know Ask!! Do not allow families to run interference If patient chooses not to know now, may ask later Share the information Plan agenda know beforehand what information has to get across eg diagnosis, treatment, prognosis, support Start by aligning with what patient knows Share the information Allow patients to ‘get ready’ Impart information in small packets best case retention = 50% Speak English, not “Doctor” Verify message is received Respond to feelings Acknowledge emotions strong emotions prevent communication identify and acknowledge them Learn to be comfortable with silence and with emotion Respond to feelings Range of normal reaction is wide give latitude as much as possible stay calm, speak softly be gentle, yet firm stick to basic rules of interview: question-listen-hear-respond Respond to feelings Distinguish between adaptive and maladaptive behaviors Adaptive anger crying bargaining fulfilling an ambition fear hope Maladaptive rage collapse manipulation impossible “quest” anxiety/panic unrealistic hope Respond to feelings Respond with empathic responses “it must be very hard to…” “you sound angry (afraid, depressed)…” Respond to feelings In the face of true conflict: act, don’t react If you cannot change behavior, get help Planning follow-through Have plan of action Make certain patient’s understand what is fixable and what is not Always be honest Patient leaves with contract: what will happen, who to call, how to call, when to return You have one chance to get this conversation right Patient/family will remember this always How do you want to be remembered? How to Break Bad News: A Guide for Health Care Professionals Robert Buckman, M.D. Johns Hopkins University Press, 1992 ISBN: 0-8018-4491-6 • Scenario 1 Tariq, a 55-year-old chain smoker taxi driver with persistent cough for 3 months, attends your clinic to find out the biopsy report of a lesion shown on a chest x-ray and CT scan. He is rather anxious, that he has a serious condition. His biopsy report confirms that he has a Bronchogenic Carcinoma of right lung. You are required to proceed with this consultation. Scenario 2 • A 54-year-old lady attends your clinic to find out the result of an MRI of her spine. She has had constant pain all over her spine for the last 2 months. She also has a history of Breast cancer, which was treated 5 years ago. • Her report shows that she has secondaries all over her spine Proceed with this consultation. (Examination not required) SAQs (1) One of the famous strategy for breaking bad news is the SPIKES Model: Explain briefly any 3 of the 6 areas mentioned in this model? (2) What is a warning shot? What you say and what skills you use after and before breaking bad news? (3) Breaking bad news is difficult: Give 3 reasons for that?