The Intra Partum Period
advertisement

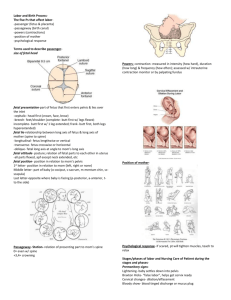
THE INTRA PARTUM PERIOD MATERNITY NURSING Study of the Childbearing process that has taken place throughout history. Involves RiskProvides rewards. They don’t call it labor for nothing!!! It is the hardest work and most intense physical work a woman will do. Pains with a purpose- just don’t say “pain”. PSYCHOPROPHYLACTIC Lamaze methods are based on classic behavioral conditioning- breathing Trained to respond to a specific event Controlled breathing is used to take attention away from the discomfort of the contraction Goal: Inhibits pain impulses to the brain and keep Mom alert and active participant BREATHING Inhale slowly through the nose and exhale through mouth Cleansing breath in and out as contraction starts and when over- exhalation should take longer In beginning, take 8-10 breaths As labor intensifies take 16-20 breaths Effleurage- significant other sits behind the Mom and massages the stomach Shallow chest breathing as progress alternating with puffs or huffs Puffs and pants through an open mouth to control the urge to push prematurely During delivery prevent sustained breath holding while bearing down- Valsalva- is not recommend say “push” or “ugh”.- Anything that interferes with Mom’s blood flow, impedes the baby’s heart flow. PYSCHOSOCIAL Dick-Read or Bradley Focuses on the natural methods of delivery Focused body relaxation Positive mental imaging NURSING MEASURES Monitor FHR not uterine soufflé (the mother’s own pulse as it perfuses the arteries) Monitor Vital signs of Mom How to take a B/P Between contractions left side lying position PREMONITORY SIGNS OF LABOR Lightening Occurs 2-3 weeks before labor “Baby drops” Baby descends into the pelvis in preparation for labor and delivery Mom breathes better Urinary frequency is increased Braxton-Hicks Mild to moderate irregular uterine tightening/contractions Do not result in cervical dilation Bloody Show Mucous plug that has sealed the uterus breaks free. Thick, stringy mucus that is streaked or tinged with blood Very little blood, must distinguish from true bleeding If bleeding, call doctor stat Spontaneous Rupture of Membranes Bag of waters which enclose, protect, and cushion the fetus May need amniotomy if not spontaneous Sudden, unexpected gush of fluid from the vagina or in a slow steady trickle of fluid ??? Urine Nitrazine test: turns blue when exposed to amniotic fluid Once membranes rupture: 24 hour deadline to deliver Increased chance of infection If membranes rupture before the presenting part of fetus is engaged may have prolapsed cord Check vaginal area Any gray bulging structure with pulsation is a prolapsed umbilical cord- 911! Head down and elevate feet May have to hold baby’s head during contraction until 911 C-section is done Based on FHR Note color, amount, odor, consistency of amniotic fluid- clear with flecks of vernix Green or brown amniotic fluid is a sign of fetal distress- called meconium stained amniotic fluid Baby will have been hypoxic- brain damage or pneumonia Weight Loss 1-3 pounds noted a few days before labor begins Hormonal changes affecting fluid and electrolytes Burst of Energy: To clean, cook or prepare home or nest- “Nesting Instinct” Caution not to overexert themselves! TRUE LABOR- CONTRACTIONS Follow regular pattern Come closer together, get stronger, and last longer Stronger with ambulation Start in lower back and move to abdomen Relaxation does not stop the contraction Cervix softens, dilates, and effaces TRUE LABOR Fetus continues descent into pelvis “5 minutes apart” rule with Primigravidas FALSE LABOR- CONTRACTIONS Do not follow predictable pattern Vary in duration and intensity Stop with ambulation Felt in abdomen or lower back Relaxation may slow or stop Cervix may soften but does not dilate or efface No fetal descent CONTRACTIONS Increment- when the uterus starts to tighten up Acme- the peak or strongest effect Decrement- the contraction starts to relax Timing contractions: From the beginning of one contraction to the beginning of the next contraction Always monitor FHR FETAL MONITORING Tocotransducer- Tocodynometer- TOCO Top of the fundus- Monitors contractions Doppler transducer over the baby’s back- FHR Continuous record of baby’s heart rate and contractions Internal monitors- 2cm dilation- more reliable but invasive Normal fetal heart rate= 110-160 Baseline Accelerations- movement 15 beats for 15 seconds= movement or hypoxia Decelerations- 15 beats for 15 seconds to be true deceleration Early-contraction- no risk to fetus occurs at the onset of contraction Late decels- mean fetal hypoxia and acidosis occurs after the contraction has already started Variable decels- can lead to fetal hypoxia-911- has no relation to the contraction Variability: fluctuations in the beat to beat FHR as a result of the autonomic nervous system activity Short term variability is more reliable but internal monitor is needed Long term variability- either external or internal can monitor but just shows large periodic changes. Duration: from the beginning of a contraction to the end of the same contraction- feel for the tightening of the uterus Relaxation: the interval between contractions- important so Mom can breathe in oxygen and get enough oxygen to the baby FACTORS AFFECTING LABOR Attitude- body position or posture- flexed or extended- head to chest- arms to chestposition that takes up less space Lie- relationship of long axis of baby to long axis of Mom- longitudinal or horizontal Presentation- part of fetal body that enters the pelvic cavity first and therefore is the first part to exit from the mother’s body- head is most common called cephalic If the fetus is in the flexed position- back portion of the skull or vertex is in contact with the cervix also called occiput If slightly extended- brow presentation- B When fetus is fully extended- the face or mentum is presenting part Cephalic is desirable with vertex presentation most desirable for dilation and effacement of cervix Single footling Complete and frank breech- s for sacrum Scapula- Sc or A Position- refers to the relationship of the presenting part of the fetus with the Mom’s pelvis Side of maternal pelvis: R or L anatomically Presenting part: O for occiput- M for mentum- S for sacrum- Sc or A for scapula or acromion process. Relative position of landmark to pelvis A- anterior- aligned with anterior portion of maternal pelvis P- posterior- aligned with posterior portion of maternal pelvis T- transverse- aligned with either side or horizontal Shape of maternal pelvis “passage” Uterine contractions- the “push power” Ability to bear down Psychological readiness “psyche” Full bladder impedes labor Epidural Anesthesia slows down labor TERMS Station- refers to the relationship between the presenting part of the fetus and an imaginary line drawn between the ischial spines of the maternal pelvis -5 to +5 False pelvis/true pelvis- linea terminalis 2 innominate bones: ischium, ileum and symphis pubis Effacement- 100%- progressive shortening and thinning of the vaginal portion of the cervixlong and thick- 0% Dilation- 10 cm- progressive expansion or enlargement of the cervical opening- 1in=2.5 cm CARDINAL MOVEMENTS Descent Engagement- head at the level of spines Flexion Internal Rotation Extension External Rotation Expulsion FIRST STAGE OF LABOR- DILATION AND EFFACEMENT Onset of true labor until complete dilation and effacement of the cervix (6-18 hours) 1. Latent- Onset of labor until 3 cm dilation and 50% effaced (station -5 to 0) Contractions 5-10 minutes apart Lasts 8-9 hours Do not give pain relief during this stage as it will stop contractions 2. Active- 4-7 cm dilation and 75% effaced 0 station Contractions 3-4 minutes apart and around 45-60 seconds best for dilation and effacement Last 4-6 hours Can give pain relief now 3. Transition- 8 cm to full dilation at 10 cm. 100% effaced Station +1-+2 Contractions occur every 1-2 minutes (should not go beyond 60 seconds) Shortest phase lasting less than 3 hours Restless, vomiting, rectal pressure Mom may want to push but cannot!! Pushing can cause cervical swelling and lifelong cervical complications including hemorrhage May hyperventilate and develop respiratory alkalosis-numbness/tingling Paper bag or cup hands around mouth and nose to re-breathe CO2 Direct eye contact and simple commands CONTRACTIONS Contractions that occur at 2-3 minute intervals and last approximately 60 seconds are best at dilating the cervix and allows for re-oxygenation of the fetus and uterine muscles Report contractions that occur 2 minutes apart and last more than 90 seconds- would most likely be in the transition stage and can indicate fetal hypoxia and death 2 N D STAGE- DELIVERY Starts with 10 cm. fully effaced and ends with delivery of the baby 2 hours for a primagravida or a few minutes with a Multigravida varies according to person and if late medication or with epidural Bearing down reflex- urge to push Episiotomy/Lacerations Check nuccal cord around neck If delivery is imminent within 2 hours---no pain meds ASSISTANCE- NEEDS HELP!! Forceps Low forceps delivery rather than high or mid forceps deliver Low forceps- when baby’s head is visible on perineum Complications: brain trauma, facial paralysis Vacuum assistance Caput succedaneum Complications: edema or cephalhematoma and bleeding 3 R D STAGE- DELIVERY OF THE PLACENTA Begins with delivery of the neonate and ends with the delivery of the placenta Duration: 20 minutes Signs: lifting, rounding, and firm shape of the uterussudden small gush of blood Lengthening of the cord that extends from the vagina PLACENTA Shiny Schultze: leaves the vagina with smooth shiny fetal side Dirty Duncan: Leaves with rough raw bloody maternal side (more likely to leave fragments) Inspected closely: looking for retained placental fragments 4 T H STAGE- RECOVERY 1-4 hours following delivery Exhilaration Exhaustion Watch for hemorrhage- suspect problem when saturates 1 pad in hour/massage fundus Lochia rubrae- 1-4 days- red, bloody, drainage Lochia serosa- 4-7 days- pink drainage Lochia alba- 7th day to 3 weeks white drainage AT DELIVERY Uterus firmly contracted to compress the internal blood vessels Fundus should be midline and at the level of the umbilicus will descend 1 cm./day Soft, boggy uterus indicates inadequate contractions After pains/oxytocin from Posterior Pituitary stimulates contractions (LPN can administer this Pitocin) LACERATIONS 1st degree- skin and mucous membranes of the posterior connection of the labia minora and outer vagina 2nd degree- same and plus muscles and fascia up to the anal sphincter 3rd degree- same but extends through the anal sphincter 4th degree- same but extends through the anterior rectal wall- ice vs. heat/sprays/surgery INDUCTION Amniotomy Prostaglandin gel on cervix or vaginal suppository ONLY GIVEN BY RN to soften the cervix Pitocin or oxytocin drip-DONE ONLY BY RN Watch I&O (will get ADH also), contractions, and fetal distress LABOR INDUCTION OR AUGMENTATION Oxytocin (Pitocin) stimulates uterine contractions Nursing observations during induction/augmentation Fetal heart rate Character of contractions If abnormality occurs, nurse stops oxytocin and begins measures to reduce contractions and increase placental blood flow CESAREAN SECTION- 25% Fetal Distress Failure to make progress Abnormal Presentation CPD- cephalopelvic disproportion Genital Herpes Abruptio Placentae Previous C-Section C-SECTION NPO except antacid- preop teaching Catheterization IV Midline Incision for emergency Pfannestiel incision or low transverse or low horizontal incision along the pubic hairlinebikini incision Massage fundus from the side toward the middle of the incision ANESTHESIA RECOVERY General Anesthesia can cause uterine atony- watch for hemorrhage as VS, Pad count, signs of shock Regional anesthesia-Epidural anesthesiaWatch for maternal hypotension Numbness and paralysis Reaches T6-7 Still during insertion Position- sit up Slows down contractions Time contractions for mom Safety- Give 2000 mL IV’s before delivery- Biggest complication is maternal hypotension PHARMOCOLOGICAL PAIN MANAGEMENT Analgesics and adjunctive drugs Regional analgesic and anesthetics Local Infiltration Pudendal Block- through the vagina and numbs the cervix Epidural block Subarachnoid block (spinal block)/Saddle block- 3-5 minutes/paralysis of lower extremities/ headache 24-72 hours Caudal block General Anesthesia- get out in 7 minutes or the anesthesia will go to the baby C-SECTION Mom is always at risk post C-section of uterine rupture during next delivery VBAC debate Even more of a risk after a classic incision for emergency C-section. RH ISOIMMUNIZATION Blood typing and cross matching A, B, AB, O Rh + If blood type differs between Mom and Baby then antibodies will be built up Recessive gene- Both parents have to contribute (–) in order for baby to remain negative If (-) mother and (+) baby, the first baby will be fine but then subsequent babies will be destroyed by the mother Rhogam must be given with 72 hours after the first birth to prevent antibodies, or if Rhmom will be given Rhogam at 28 weeks to prevent.