Cartilage
advertisement

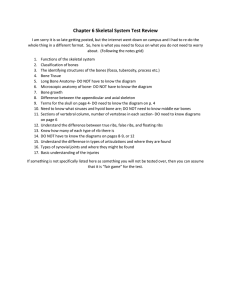
Chapter 11 Skeletal System Points to Ponder • • • • • • What are the 5 functions of the skeletal system? What are the parts of a long bone? How do bones grow, remodel and repair? How are hormones involved in bone growth? What is osteoporosis? How are age, gender and ethnicity determined through skeletal remains? • What are the components of the axial and appendicular skeletons? • What are synovial joints and what kind of angular movements to they allow? Functions of the Skeletal System 1. 2. 3. 4. Supports the body. Protects the soft body parts. Produces blood cells. Stores minerals (calcium and phosphate) and fat. 5. Allows for movement by attaching muscles. Anatomy of a Long Bone • Diaphysis: Shaft of the bone; made of compact bone. – Large shaft (medullary cavity) filled with yellow marrow. • Epiphysis: Ends of the bone made mostly of spongy bone. – Coated with thin layer of articular cartilage. • Articular cartilage: Hyaline cartilage found on the ends of long bones. Anatomy of a Long Bone • Yellow bone marrow: Stores fat. • Red bone marrow: Makes blood cells; found in spongy bone and flat bones. • Periosteum: Living, outer covering of the entire long bone composed of fibrous connective tissue. – Blood vessels, lymphatic vessels, nerves. • Ligaments: Fibrous connective tissue that connects bones. Compact Bone • Composed of osteons with a central canal containing blood vessels. – Lie in the lacunae (arranged in concentric circles around the central canal). • Contains living bone cells (osteocytes) that lie in the lacunae. Compact Bone • Canaliculi (tiny canals) run through the bone matrix. – Connect lacunae with each other and the central canal. • Osteocytes nearest center of the osteon exchange nutrients and wastes with the blood vessels at the central. Spongy Bone • Made of plates (trabeculae) separated by uneven spaces; filled with red bone marrow. • Lighter than compact bone, but still made for strength. – Trabeculae follow lines of stress. Cartilage • Cartilage: Flexible, gel-like connective tissue (collagenous and elastic fibers) made of cells called chondrocytes. • No nerves or blood vessels; slow to heal. • 3 main types: – Hyaline cartilage: Ends of long bones, nose, ends of ribs, larynx and trachea. – Fibrocartilage: Disks between vertebrae and in the knee; stronger than hyaline cartilage. – Elastic cartilage: Ear flaps and epiglottis; more flexible than hyaline cartilage. Bone Growth, Remodeling and Repair • Skeleton forms at 6 weeks in fetus development. • Most bones grow in width and length during adolescence; some continue until 25. • Remodeling: Bone changes of size, shape and strength due to stress on the bone. Important Cells in Bone Growth, Remodeling and Repair • Osteoblasts: Bone-forming cells; promote deposition of calcium and salts into bone matrix. • Osteocytes: Mature bone cells that maintain bone structure; Derived from osteoblasts. • Osteoclasts: Bone-absorbing cells; break down calcium and phosphate to return it to the blood. • Chondroytes: Cartilage-forming cells. Bone Development and Growth • Ossification: Formation of bone. • Occurs in two distinct ways: 1. Intramembranous Ossification: Bone development between sheets of fibrous connective tissue; flat bones. – These bones retain red bone marrow. – Ex. Skull bones 2. Endochondrial Ossification: Cartilage is replaced by bone; most bones formed this way. Intramembranous Ossification Endochondral Ossification • 1st Cartilage model: Chondrocytes lay down hyaline cartilage in the shape of the future bones; occurs in embryo. • 2nd Bone collar formation: Osteoblasts secrete bone matrix, resulting in a collar made of compact bone; thickens over time. • 3rd Primary ossification center: Osteoblasts are brought interiorly by blood to lay down spongy bone. • 4th Secondary ossification sites: Bone centers in the epiphyses are formed after birth. • 5th Epiphyseal plate: Growth plate (band of cartilage) between primary and secondary ossification center allows bones to lengthen. Visualizing Endochondral Ossification How do bones lengthen? Final Size of the Bones • When epiphyseal plates close, bone growth no longer occurs. – Women: Arm and leg plates close at 16-18 – Men: Arm and leg plates close at 20. – Other bones may grow to age 25. • Plate closure is controlled by hormones. Hormones and Bone Growth • Growth hormone (GH): Stimulates general bone growth and growth of the epiphyseal plates. – Requires adequate cellular metabolism. • Diet and thyroid hormone. • Sex hormones: Increases osteoblast activity causing “growth spurt” during adolescence. • Vitamin D: Converted to a hormone to allow calcium absorption in the intestine. Bone Remodeling and its Role in Homeostasis • Bone remodeling: Bone renewal to keep bones strong; allows them to respond to stress. – Rate of up to 18% per year. • Allows body to regulates the calcium in the blood through hormones: ** Calcium in blood allows blood to clot! – Parathyroid hormone (PTH): Stimulates osteoclasts to dissolve calcium matrix of bone; Increases blood calcium by accelerating bone recycling. – Calcitonin: Decreases blood calcium. Steps in Bone Repair • Hematoma (6-8 hrs.): Blood clot formed between broken bones. • Fibrocartilaginous callus (~ 3 weeks): Cartilaginous callus filling the space between broken bones. • Bony callus (3-4 months): Cartilaginous callus is turned to bone to join bones together. • Remodeling: Osteoblasts build new compact bone at the periphery; Old bone tissue is replaced by new bone tissue. Bone Repair Health focus: Osteoporosis • Osteoporosis: Bones are weakened due to a decreased bone mass. • Bone reabsorption exceeds absorption usually by age 40. • Risk factors: Women, white or Asian, thin, family history, early menopause, smoking, diet low in calcium, excessive caffeine or alcohol consumption and a sedentary lifestyle. • Can lead to fractures and other complications. • Can be treated with drugs, hormones and lifestyle change. The 206 Bones of the Skeleton Science focus: Skeletal remains Characteristics to be determined: 1. Age: approximated through dentition, studying areas of bone ossification and joint condition 2. Gender: pelvic bone is best used, thickness of long bones, skull characteristics 3. Ethnicity: difficult to tell but skull characteristics are most useful The Axial Skeleton • Skull: Made of cranium and facial bones. • Hyoid bone • Vertebral column: Vertebrae and intervertebral disks. • Rib cage: Ribs and sternum. The Skull: The Cranium • Cranium: – Protects the brain. – Composed of 8 bones. – Some contain sinuses. Bones of the Face and the Hyoid Bone • Facial bones: – Mandible – Maxillae – Zygomatic bones – Nasal bones • Hyoid: – Only bone that does not articulate with another bone. The Vertebral Column • Types of vertebrae: – 33 vertebrae • Cervical (7) • Thoracic (12) • Lumbar (5) • Sacrum (5 fused) • Coccyx (4 fused into tailbone) • Intervertebral disks – Fibrocartilage between vertebrae. The Rib Cage • Ribs: Protects heart and lungs. – Flattened bone originating from the thoracic vertebrae. – 12 pairs: • 7 pr. true ribs • 3 pr. false ribs • 2 pr. floating ribs • Sternum (Breastbone) The Appendicular Skeleton • Pectoral girdle and upper limb • Pelvic girdle and lower limb The Appendicular Skeleton • Pectoral girdle: – Scapula and clavicle. • Upper limb: – Arm and hand bones. The Appendicular Skeleton • Pelvic girdle: – Coxal bone • Lower limb: – Leg and foot bones Types of Joints (Where Bones Meet Bones) • Fibrous: Usually immovable. – Ex. Sutures between cranial bones. • Cartilaginous: Tend to be slightly movable. – Ex. Intervertebral disks • Synovial: Freely movable joints. – Ex. Ball-and-socket hip and shoulder joints; knee joint. Anatomy of a Synovial Joint Summary of Synovial Joints Movements • • • • • • Flexion: Decrease in joint angle. Extension: Increase in joint angle. Adduction: Body part moves toward midline. Abduction: Body part moves away from midline. Inversion: Sole of foot turns inward. Eversion: Sole of foot turns outward. Visualizing Synovial Joints Movements