Tissue and Cellular Injury
advertisement

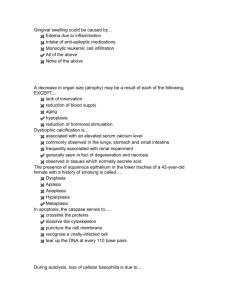
2. Necrosis Severe damage Metabolism stop Structure destroy Function lose Classification: necrosis & apoptosis (1) Definition: Localized death of cell or tissue occurring in the living body. (2) Cell death is recognized by: ① Ultrastructural changes Margination or progressive nuclear chromatin loss of Focal rupture of the nuclear membrane Breakdown of the plasmalemma. Development of flocculent densities in mitochondria. ② Changes in the nucleus. Pyknosis: condensation of chromatin of chromatin and shrinkage of the nucleus. Karyorrhexis: nucleus. fragmentation of the Karyolysis: dissolution of the nucleus. Normal Pyknosis Karyorrhexis (参照武忠弼 病理学规划教材第一版 人民卫生出版社1979,修改) Karyolysis ③ Changes in cytoplasm staining Positive staining with vital dyes such as Trepan blue which reflects abnormal membrane permeability. Opacification: denaturation of proteins lead to aggregation with resultant opacification of the cytoplasm. Eosino0.philia: exposure of basic amino groups results in increased affinity for acidic dyes such as eosin. ④ Biochemical changes Release of K+ by dead cells. Release of enzymes into the blood. e. g. increased plasma levels of creatine kinases, lactic dehydrogenase and aspartate aminotransferase. Release of protein or protein breakdown products into the blood. ⑤ Postmortem change: General of normal tissues occurring dead body, generally distinguished from necrosis by being diffuse and not associated with inflammatory response. ⑥Autolysis: Digestion of cell by enzymes released from lysosome; occurs after cell dies. (3) Types: ① Coagulative necrosis: Gross features: The necrosis area is swollen, firm and pale. LM: cell detail is lost, but architecture preserved. The dead cells retain their outline but only indistinctly. This type of necrosis is frequently caused by lack of blood supply and is exemplified well in infarcts of solid organs, e. g. heart, spleen, kidney. Coagulative necrosis of kidney Coagulative necrosis of the left ventricular wall (From ROBBINS BASIC PATHOLOGY,2003) Special types of coagulative necrosis A. Caseous necrosis: Gross features: soft, granular, and friable a cream-cheesy appearance. granular, eosinophilic. LM: architecture completely destroyed. i. e. Tuberculosis, syphilis, some sarcoma. A tuberculous lung with a large area of caseous necrosis From ROBBINS BASIC PATHOLOGY,2003) Caseous necrosis Special types of coagulative necrosis B. Gangrene Definition: necrosis of big tissue with superadded putrefaction, black, fou-smelling appearance. Necrosis of big tissue putrefactive black, green Or organ or limb organisms infection appearance (black or green due to breakdown of haemoglobin) Types of gangrene : a. Dry gangrene: Conditions: only occurs on the skin surface following arterial obstruction. It is particularly liable to affect the limbs, especially the toes. Character: mummification Dry gangrene Offered by Prof.Orr Types of gangrene : b. Wet gangrene: Conditions: Both arterial and venous obstruction; wet in environment; Character: wet swollen, foul-smelling, black or green. Commonly in small intestine, appendix, lung, and uterus, also in limbs. Moist gangrene Types of gangrene : c. Gas gangrene: Conditions: deep contaminated wounds in which there is considerable muscle damaged by gas formation bacteria. Character: swollen obviously, gas bubbles formation. The infection rapidly spreads and there is associated severe toxaemia. Only occasionally in civilian practice but is a serious complication of war wounds. ② Liquefactive necrosis: Soft and liquid grossly. Enzymes digest the cell and convert it to a formless proteinaceous mass. Ultimately, discharge of the contents forms a cystic space. i. e. central nervous system after ischemic injury; abscesses. Special type: Fat necrosis: Grossly: Opaque and chalky LM: outline of necrotic fat cells filled with amorphous basophilic material (calcium soaps). i. e. Digestion of peritoneal fat by pancreatic enzymes in pancreatic inflammation. Fibrinoid necrosis: Definition: This is not a true degeneration but a strongly eosinophilic stain like fibrin. Location: interstitial collagen and blood vessels (small artery and arteriole) Nature: one kind of necrosis. e. g. in allergic reactive diseases: active rheumatism, polyarteritis nodose. in non-allergic reactive diseases: malignant hypertension. Fibrinoid change in blood vessel (4) Consequences of necrosis ① Acute or chronic inflammation ② Immunological reactions to sub cellular components released by dead tissue or self-antigens altered by denaturation. ③ lysis and absorption ④ Isolation and discharge: ulceration and cavity formation ⑤ organization ⑥ encapsulation, calcification.