pathophysiology 3
advertisement

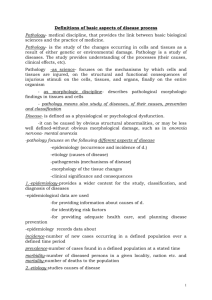
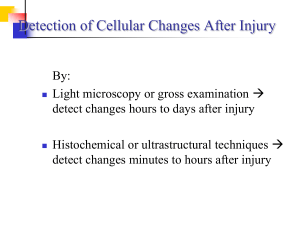
CELL INJURY & CELL DEATH Overview of Cellular Injury • Cells actively control the composition of their immediate environment and intracellular surrounding within a narrow range of physiological parameters (“homeostasis”) • Under physiological stresses or pathological stimuli (“injury”), cells can undergo adaptation to achieve a new steady state that would be compatible with their viability in the new environment. • Cellular injury may be a reversible process, in which case the cells can recover their normal function, or it may be irreversible and lead to cell death and necrosis • If the injury is too severe (“irreversible injury”), the affected cells die. Overview of Cellular Injury Reversible and Irreversible Cell Injury Outcomes from cell injury depend upon: 1. Type of injury 2. Severity of the injury 3. Duration of the injury 4. Type of cell being injured-Some cell types sustain injury better than others; some tissues (e.g. liver) have a capacity to regenerate. Causes of Cellular Injury ()أسباب اإلصابة الخلوية 1. Hypoxia (oxygen deficiency) and ischemia (blood flow deficiency) 2. Physical injury • Mechanical trauma • Temperature extremes (burn injury, frostbite ) • Electrical current 3. Chemical injury • Chemicals, toxins, heavy metals, solvents, smoke, • pollutants, drugs, gases 4. Radiation injury • Ionizing radiation — gamma rays, X rays • Non-ionizing radiation — microwaves, infrared, laser 5. Biologic agents • Bacteria, viruses, parasites 6. Nutritional injury • Malnutrition: Protein deficiency • Over nutrition: Obesity More Energy Ionizing Radiation Less Energy Non -ionizing Radiation Mechanisms of Cellular Injury the underlying mechanisms of cellular injury usually fall into one of two categories: 1. Uncontrolled free radical injury 2. hypoxic injury (impaired oxygen delivery or utilization) . Primary Site of Impact 1) Oxidative phosphorylation - ATP generation 2) Membrane integrity - osmotic pump 3) Protein synthesis - cell repair 4) Nuclear integrity - direction of cell functions Free Radical Injury • Free radicals are highly reactive chemical species that have one or more unpaired electrons in their outer shell. • Examples of free radicals include superoxide (O2−), hydroxyl radicals (OH−) and hydrogen peroxide (H2O2). • Free radicals are generated as by-products of normal cell metabolism and are inactivated by free radical–scavenging enzymes within the body such as catalase and glutathione peroxidase • When excess free radicals are formed from exogenous sources or the free radical protective mechanisms fail, injury to cells can occur. Free Radical Injury • Free radicals are highly reactive and can injure cells through: 1. Peroxidation of membrane lipids 2. Damage of cellular proteins 3. Mutation of cellular DNA • Exogenous sources of free radicals include tobacco smoke, organic solvents, pollutants, radiation and pesticides. • Free radical injury has been implicated as playing a key role in the normal aging process as well as in a number of disease states such as diabetes mellitus, cancer, atheroscelrosis, Alzheimer’s disease and rheumatoid arthritis. Effects of free radical cell injury Hypoxic Cell Injury • Hypoxia is a lack of oxygen in cells and tissues that generally results from ischemia. • During periods of hypoxia, aerobic metabolism of the cells begins to fail. • This loss of aerobic metabolism leads to dramatic decreases in energy production (ATP) within the cells. • The pH of the extracellular environment begins to decrease as waste products (such as lactic acid, a product of anaerobic metabolism) begin to accumulate. Hypoxic Cell Injury • The cellular injury process may be reversible, if oxygen is quickly restored, or irreversible and lead to cell death. • Certain tissues such as the brain are particularly sensitive to hypoxic injury. Death of brain tissues can occur only 4 to 6 minutes after hypoxia begins. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Unit 3 Objectives Define homeostasis of cells? Write the types of cell injury? Write the characteristics of reversible injury? Write the characteristics of irreversible injury? Write the factors on which the outcome of disease depends on? Define the different cause or etiology of disease? Name the 2 main mechanisms of cellular injury? What are free radicals? Name the free radicals found in the body? Name the free radical scavenging enzyme? How does the free radical bring about cell injury? Name the important disease caused as a result of free radical injury? Write the mechanism of hypoxic cell injury? What happens when there is loss of ionic balance in hypoxic cells? Cell Death Cell Death • Like disease, cell death may be caused by • internal (intrinsic) factors that limit the cell's life span or • external (extrinsic) factors that contribute to cell damage and aging. • When a stressor is severe or prolonged, the cell can no longer adapt and it dies. • Cell death, or necrosis, may manifest in different ways, depending on the tissues or organs involved. Cell Death Apoptosis :Individual Cell Death • Apoptosis is genetically programmed cell death. • common event in some regenerating tissues: such as skin and gut epithelium and during embryogenesis • Not a typical event in developed tissues such as brain • Becomes a serious occurrence when many cells are involved in such organs as the liver Examples of Physiologic Apoptosis (A) separation of webbed fingers and toes in embryo, (B) development of neural connections, (C) removal of cells from intestinal villa, and (D) removal of senescent (old) blood cells. Examples of Pathologic Apoptosis 1. Irradiated tissues 2. Viral infections e.g. Viral Hepatitis 3. Hormone-dependent atrophy of tissue (e.g., endometrial cell breakdown after withdrawal of estrogen and progesterone in the menstrual cycle) 4. Death of tumor cells by cytotoxic T cells Types of Necrosis 1) Liquefactive necrosis: in brain, 2) Caseous necrosis: Infection with Mycobacterium tuberculosis 3) Fat necrosis: Liver and pancreas 4) Coagulative necrosis: Necrosis of kidney, liver, or heart muscle 5) Gangrene: Necrosis of an appendage, usually limbs Necrosis 1. Liquefactive necrosis occurs when a lytic (dissolving) enzyme liquefies necrotic cells. • It is generally associated with abscess formation • Typically, liquefaction necrosis occurs in brain infarcts and pancreatic necrosis. • Liquefaction by leukocytic enzymes is called suppuration, and the resultant fluid is called pus. E.g. brain abscess 2. In caseous necrosis, the necrotic cells disintegrate but the cellular pieces remain undigested for months or years. *This type of necrotic tissue gets its name from its crumbly, cheese- like (caseous) appearance. It commonly occurs in lung tuberculosis. Necrosis 3. In fat necrosis, *enzymes called lipases break down intracellular triglycerides into free fatty acids. These free fatty acids combine with sodium, magnesium, or calcium ions to form soaps. The tissue becomes opaque and chalky white. It is characteristic of tissues adjacent to pancreatic necrosis. 4. Coagulative necrosis *is the most common form of necrosis in cells without large numbers of lysosomes. *Commonly occurs when the blood supply to any organ (except the brain) is interrupted (ischemia). *It typically affects the kidneys, heart, and adrenal glands. Lytic (lysosomal) enzyme activity in the cells is inhibited, so that the necrotic cells maintain their shape, at least temporarily. Necrosis • 5- Gangrenous necrosis, • a form of coagulative necrosis, typically results from a lack of blood flow and is complicated by an overgrowth and invasion of bacteria. • It commonly occurs in the lower legs as a result of arteriosclerosis or in the gastrointestinal tract( GIT). Necrosis Gangrene can occur in one of three forms: dry, moist (or wet), or gas. 1. Dry gangrene occurs when bacterial invasion is minimal. It's marked by dry, wrinkled, dark brown or blackened tissue on an extremity. 2. Moist (or wet) gangrene develops with liquifactive necrosis that includes extensive lytic activity from bacteria and white blood cells to produce a liquid center in an area of tissue. It can occur in the internal organs as well as the extremities. 3. Gas gangrene develops when anaerobic bacteria of the genus Clostridium infect tissue. It's more likely to occur with severe trauma and may be fatal. The bacteria release toxins that kill nearby cells and the gas gangrene rapidly spreads. Release of gas bubbles from affected muscle cells indicates that gas gangrene is present. Difference between Apoptosis & Necrosis Apoptosis Regulation Genetic programmed Control Cell shape Plasma membrane integrity Cellular process Controlled Skrinkage, condensed Necrosis Ischemia, trauma or ATP depletion Uncontrolled Swelling Maintained Collasped Budding Packaged in apoptoic bodies Fragmentation, chromatin condensation ATP required Absent Caspase Blebbing Leakage to extracellular fluid Cellular content DNA Energy Inflammatory response Mediator No fragmentation Not required Present Caspase-independent Unit 3 Objectives 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Define apoptosis? Give examples of physiological apoptosis? Give examples of pathological apoptosis? Name the types of Necrosis and the organs affected by them? What is liquefactive necrosis? Which type of necrosis is associated with abscess formation? Where would you find liquefactive necrosis? What is caseous necrosis? Which type of necrosis there cheese like appearance? Define fat necrosis? In which type of necrosis the tissue becomes chalky white? Which is the most common form of necrosis? Unit 3 Objectives 13. 14. 15. 16. 17. 18. 19. 20. In which type of cells would you find fat necrosis? Define coagulative necrosis? What is gangrenous necrosis? Define the 3 forms of gangrene? Write the difference between apoptosis and necrosis? Write about the necrotic changes in the nucleus? What is pyknosis, karyolysis, and karyorrhexis Name the Enzyme Markers of Cell Death?