Rh Blood Group
advertisement

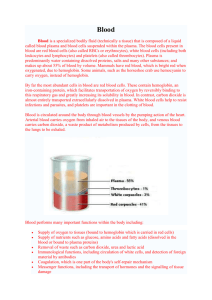
Blood!! Blood • The fluid portion of cardiovascular system • Connective Tissue • Serves the body’s 75 Trillion Cells!! WOW! Blood • Blood is a sticky opaque fluid with a characteristic metallic taste. • Blood has a pH of 7.3-7.4 • Oxygen rich blood is more scarlet in color while oxygen poor blood is a dark red color. • Average adult male has 5-6 liters of blood, while the female is slightly less with 4-5 L. Functions of Blood • Transports – – – – – Gases Nutrients Electrolytes Hormones Wastes ex: urea and uric acid Functions of Blood • Restricts blood loss – Clotting • Defends against pathogens and toxins. – White blood cells – Antibodies • Distributes heat produced by cells • Regulates interstitial fluid by exchange with capillaries. Blood and Blood Cells • Whole blood is slightly heavier 3 to 4 times more viscous than water. • Its cell form mostly in red bone marrow, include white and red blood cells. (Bone marrow transplants often take place in the ilium..your hip) • Blood also contains cellular fragments called blood platelets. Composition of Blood • Whole Blood = • Plasma + formed elements • a solution cells & platelets Composition of Blood • • • • • 45% Formed elements Platelets Red Blood Cells White Blood Cells Most of the formed elements is RBC..99% • • • • 55% Plasma Electrolytes Water Proteins- Albumins, Globulins, Fibrinogen • Wastes • Gases • Nutrients, Vitamins, Hormones. Blood • If a sample of blood is spun in a centrifuge, the heavier formed elements are packed down by the centrifugal force and the less dense plasma remains at the top. Blood • You have three distinct layers – Plasma –(55% of whole blood) – Buggy Coat(leukocytes and platelets < 1% of whole blood) – Erythrocytes (45% of whole blood) Blood Blood Plasma Plasma • (You may have to add this material to your notes…NOT in guided reading) • Function: • • • • • Maintaining osmotic balance, Buffering against pH changes Maintain blood viscosity Transporting materials through blood Blood clotting. Erythrocytes aka Red Blood Cells • Red Blood Cells (erythrocytes) are tiny flattened discs with depressed centers. • They have no nucleus and have basically no organelles. • Essentially they are little bags of hemoglobin (Hb) which is the protein that functions in gas transport. Erythrocytes aka Red Blood Cells • It is its special shape that is an adaptations that allows it to readily squeeze through the narrow passages of capillaries. Structure of Hemoglobin • Hemoglobin, the protein that makes red blood cells red, binds easily and reversibly with oxygen, and most oxygen carried in blood is bound to hemoglobin. Erythrocytes aka Red Blood Cells • The number or count varies from individual to individual. • Increase in number during strenuous exercise, increase in altitude • They live approx. 120 days and travel through the body about 75,000 times. • They age with time, they become more fragile and can be damaged simply by passing through capillaries. Erythrocytes aka Red Blood Cells • The production of RBC are controlled through Negative Feedback and a hormone called erythroprotein. • A deficiency of red blood cells or a reduction in the amount of the hemoglobin they contain results in a condition called anemia. Sickle Cell Anemia • Sickle cell anemia (uhNEE-me-uh) is a serious disease in which the body makes sickle-shaped red blood cells. “Sickleshaped” means that the red blood cells are shaped like a "C." Sickle Cell Anemia • Sickle cells contain abnormal hemoglobin that causes the cells to have a sickle shape. Sickleshaped cells don’t move easily through your blood vessels. They’re stiff and sticky and tend to form clumps and get stuck in the blood vessels. (Other cells also may play a role in this clumping process.) • The clumps of sickle cells block blood flow in the blood vessels that lead to the limbs and organs. Blocked blood vessels can cause pain, serious infections, and organ damage. Sickle Cell Anemia Leukocytes aka White Blood Cell • White Blood cells or leukocytes protect against disease. • Work outside the circulatory system. • They are transported in the blood to sites of infections. • Leukocytes can phagocytize bacterial cells in the body. • Other produce antibodies that destroy foreign particles. Leukocytes aka White Blood Cell • White Blood cell count should range between 5-10,000 per cubic millimeter. • Too many is called leukocytosis- could indicate acute infections such as appendicitis • Too few is called leukopenia…such a deficiency may accompany typhoid fever, influenza, measles, mumps… Leukocytes aka White Blood Cell • There are five different types of white blood cells. – – – – – Neutrophilis Lymphocytes Monocytes Eosiniphils Bbasophils Blood Platelets • Blood platelets are not complete cells, less than half the size of a RBC. • Help repair damaged blood vessels by sticking to broken surfaces. • They release serotonin, which contracts smooth muscles in the vessel walls, reducing blood flow. Composition of Blood Types of Blood Cells Hemostasis • Refers to the stoppage of bleeding. • Is vitally important when smaller blood vessels are damaged. • Larger vessels may result in a severe hemorrhage that requires treatment. • Following injury, these 3 actions may prevent blood loss: • Blood Vessel Spasm • Platelet Plug Formation • Blood Coagulation Extrinsic and Intrinsic Clotting Mechanisms. • Extrinsic – Triggered when blood contacts damaged blood vessel walls or tissues outside blood vessels. • Intrinsic – Stimulated when blood contacts with foreign surfaces in the absence of tissue damage. • All components necessary are in blood. Blood Vessel Spasm • Cutting or breaking a smaller blood vessel stimulates the smooth muscles in its wall to contract, an event called vasospasm. • Blood loss lessens immediately and severed vessel may close. • This effect results from stimulation of vessel as well as reflexes elicited by receptors. • Blockage called platelet plug has formed and blood is coagulating. Platelet Plug Formation • Platelets stick to exposed ends of injured blood vessels. • They adhere to any rough surfaces. • When in contact with collagen, shapes change drastically. • Platelets stick to each other forming a platelet plug in the vascular break. Platelet Plug Cont. • A plug may control blood loss from a small break, but a larger one may require a blood clot to halt bleeding. Blood Coagulation • The most effective hemostatic mechanism. • Causes formation of a blood clot by a series of reactions, each one activating the next in a chain reaction. • May occur in extrinsic or intrinsic clotting mechanism. • Utilizes many biochemicals called clotting factors. • Vitamin K is necessary. Blood Coagulation Cont. • The major event in blood clot formation is conversion of the soluble plasma protein fibrinogen into insoluble threads of the protein fibrin. • Activation of certain plasma proteins triggers the conversion. Blood Types • In 1910, Physician Karl Landsteiner identified the ABO blood antigen gene. • Today 20 different genes are know to contribute to the surface features of red blood cells, which determine compatibility between blood type. • Agglutination – Clumping of red blood cells when testing blood compatibility or resulting from a transfusion reaction. Antigens and Antibodies • Although there are many different antigenes in humans only a few of them trigger serious transfusion complications. • Antigens – Red blood cell surface molecules. • Antibodies – Proteins carried in plasma. • Avoiding the mixture of certain kinds of antigens and anitbodies prevents adverse transfusion reactions. ABO • ABO blood group is based on the presence ( or absence) of 2 major antigens, A and B. • A persons antigen combination can be only A, only B, both A and B, or neither A nor B. • If persons antigen is – • • • • Only A = A blood type. Only B = B blood type. Both A and B = AB blood type. Neither A nor B = Type O blood. Permissible Transfusion!! • You must keep in mind that you cannot except a blood type that has anitbodies against your own. • O is often called the universal donor because it lacks antigen A and B, however it does contain BOTH anti A and anti B antibodies so it can only except blood from another type O. Blood Types Blood Type Antigen Antibody A A Anti-B B B Anti-A AB A and B Neither anti-A nor anti-B O Neither A nor B Both anti-A and anti-B Preferred and Permissible Blood Types Blood Type of Recipient Preferred Blood Type of Donor A A Permissible Blood Type of Donor A, O B B B, O AB AB AB, A, B, O O O O The Rh Blood Type System • When we are told our blood type, it is usually expressed as a letter followed by either a positive (+) or negative (-). • This positive and negative indicates the Rh factor. The Rh factor determines the presence or absence of a protein on the surface of the RBC. If you carry this protein, you are Rh positive. If you don't carry the protein, you are Rh negative • 85% of the population is Rh +. The Rh Blood Type System • The Rh system is actually much more complicated than the ABO system because there are more than 30 combinations possible when inherited, however for general usage, the Rh proteins are grouped into two families - either positive or negative. The Rh Blood Type System • As with the ABO system, there is a dominant allele which happens to be the positive family. This means that the genetic pairs that can exist in humans are as follows: • Genetic makeup Blood type ++ Rh positive +Rh positive -Rh negative The Rh Blood Type System • Rh+ blood can never be given to someone with Rh - blood, but the other way around works. For example, 0 Rh+ blood can not be given to someone with the blood type AB Rh -. • People with blood group 0 Rh - are called "universal donors" and people with blood group AB Rh+ are called "universal receivers." Agglutination • For a blood transfusion to be successful, AB0 and Rh blood groups must be compatible between the donor blood and the patient blood. • If they are not, the red blood cells from the donated blood will clump or agglutinate. The agglutinated red cells can clog blood vessels and stop the circulation of the blood to various parts of the body. • The agglutinated red blood cells also crack and its contents leak out in the body. The red blood cells contain hemoglobin which becomes toxic when outside the cell. This can have fatal consequences for the patient. Can blood type effect pregnancy? • Rh Compatibility? • When you find out you are pregnant one of the first things you will have is your blood type tested…why?? • Any issue regarding this primarily focuses on the Rh protein(+,-) more than the “typing”…like A, or AB. Rh Compatibility • If you and your baby are Rh-negative, there's no problem, since you both have the same Rh type. • If the father's genes are + Rh positive, and the mother's are + - Rh positive, the baby can be: + + Rh positive • + - Rh positive • - - Rh negative Rh Compatibility • If a father's Rh factor genes are + +, and the mother's are - -, the baby will have one + from the father and one - gene from the mother. The baby will be + - Rh positive. Can blood type effect pregnancy? • If you're Rh-negative and your baby is Rh-positive (thanks to your husband's genes), that's fine…. until your blood mixes with your baby's blood a bit during placental separation at birth. • At that critical point, fetal blood cells can accidentally combine with your system, and you make antibodies to fight them. Can blood type effect pregnancy? • Your immune system is successful in vanquishing these stray fetal blood cells in your circulation. • This is of no consequence, because once they've gotten rid of the baby's blood cells in your system, they have no other job. And they can't filter back through to your baby's blood, because delivery has already taken place. • The antibodies you made just remain in your circulation waiting. For what? For your next pregnancy. Herein lies the problem!!! Can blood type effect pregnancy? • In the modern world of obstetrics; they now monitor blood typing closely…shortly before or after delivery the Rh- mother is given a RhoGAM shot. • This LIMITS moms body from producing those antibodies that would actually cross through the placenta in a second baby and attack the babies RBC. Hemolytic Disease • • • • This means you have become sensitized and your antibodies can cross the placenta and attack your baby’s blood. They break down the fetus’s red blood cells and produce anemia (the blood has a low number of red blood cells). This condition is called hemolytic disease or hemolytic anemia. It can become severe enough to cause serious illness, brain damage, or even death in the fetus or newborn. Hemolytic Disease • • • • • • Sensitization can occur any time the fetus’s blood mixes with the mother’s blood. It can occur if an Rh-negative woman has had: A miscarriage An induced abortion or menstrual extraction An ectopic pregnancy Chorionic villus sampling A blood transfusion • http://www.youtube.com/watch?v=t0pyd_uJvg • http://www.youtube.com/watch?v=CRh_dA zXuoU