Blood
advertisement

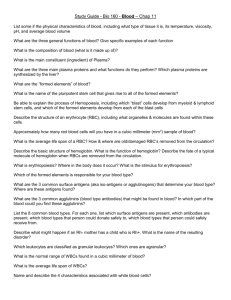
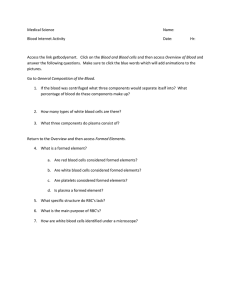
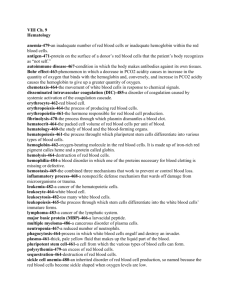
Blood Blood Functions • Transport Gases Nutrients metabolic wastes hormones • Regulate pH temperature fluid • Defense blood loss infectious agents • • • • O2 and CO2 Carbs, proteins, fats urea and uric acid Estrogen, testosterone, ADH, insulin • Between 7.45 to 7.48 • Acts as a heat resevoir to distribute it • tissues get fluid from blood • Has ability to stop blood loss • Defend against foreign invaders Blood Composition Cells = Formed Elements (not all are technically cells) Erythrocytes aka RED blood cells count ~ 5.0 million/drop Leukocytes aka White blood cells count ~ 4,000 – 11,000/drop Platelets aka Thrombocytes count 250,000 – 500,000/drp Blood Composition Matrix = Plasma 90% Water 8% Proteins albumin globulins fibrinogen 2% Other gases nitrogenous wastes nutrients electrolytes ERYTHROCYTES • Biconcave discs • Lack nucleus • Lack mitochondria • Contain hemoglobin • Carry oxygen and some carbon dioxide HEMOGLOBIN • HEME PORTION Has central Fe atom that carries one oxygen molecule Each Hemoglobin is like a 4 passenger TAXI HEMOGLOBIN • GLOBIN PORTION 4 protein chains *each chain has one heme *each RBC carries 250 million hemoglobin molecule *Therefore each RBC carries ONE BILLION O2 HEMOGLOBIN • When oxygen is bound to hemoglobin it is called oxyhemoglobin. • When oxygen is NOT bound to hemoglobin it is called deoxyhemoglobin • 20% of CO2 is transported in hemoglobin, but does not compete with oxygen site of heme CO So how can we get rid of CO? Skiing the Rockies Hematopoiesis Formation of blood Erythropoiesis: formation of erythrocytes •Starts with hemocytoblasts •Occurs in red bone marrow Hemocytoblast Stem cell Proerythroblast Committed cell Early erythroblast Ribosome production Late erythroblast Hemoglobin production Normoblast Reticulocyte Erythrocyte When hemoglobin content reaches ~35%, organelles get ejected. Eventually nucleus gets ejected. Gets released into blood stream Mature cell Time it takes for erythropoiesis Hemocytoblasts 3 to 5 days Reticulocytes 2 days more Erythrocytes Total time to replace RBCs is about ONE week Erythropoietin (EPO) • Regulates RBC production –Normal rates 2 million/sec • Kidneys control production of EPO mechanism for regulating erythropoiesis Homeostasis: Normal blood oxygen levels 1 Stimulus: Hypoxia (low blood O2- carrying ability) due to • Decreased RBC count • Decreased amount of hemoglobin • Decreased availability of O2 Homeostasis: Normal blood oxygen levels 1 Stimulus: Hypoxia (low blood O2- carrying ability) due to • Decreased RBC count • Decreased amount of hemoglobin • Decreased availability of O2 2 Kidney (and liver to a smaller extent) releases erythropoietin. Homeostasis: Normal blood oxygen levels 1 Stimulus: Hypoxia (low blood O2- carrying ability) due to • Decreased RBC count • Decreased amount of hemoglobin • Decreased availability of O2 2 Kidney (and liver to Erythropoietin stimulates red bone marrow. 3 a smaller extent) releases erythropoietin. Homeostasis: Normal blood oxygen levels 1 Stimulus: Hypoxia (low blood O2- carrying ability) due to • Decreased RBC count • Decreased amount of hemoglobin • Decreased availability of O2 Enhanced erythropoiesis increases RBC count. 4 2 Kidney (and liver to 3 Erythropoietin stimulates red bone marrow. a smaller extent) releases erythropoietin. Homeostasis: Normal blood oxygen levels 1 Stimulus: O2- carrying ability of blood increases. 5 Hypoxia (low blood O2- carrying ability) due to • Decreased RBC count • Decreased amount of hemoglobin • Decreased availability of O2 4 Enhanced erythropoiesis increases RBC count. 2 Kidney (and liver to 3 Erythropoietin stimulates red bone marrow. a smaller extent) releases erythropoietin. Induced Polycythemia Increasing the number of red blood cells in circulation - Training at higher altitudes - Blood doping Who is he? WHY DO BRUISES TURN YELLOW Fate and destruction of RBCs Hemoglobin Aged and damaged red blood cells are engulfed by Heme Globin macrophages of liver, Bilirubin Iron stored Amino spleen, and bone acids In liver marrow; the Iron is released to hemoglobin is blood from liver as broken down. needed for erythropoiesis. Urine gets its color from urochrome (comes from bilirubin) Bilirubin is picked up from blood by liver, secreted into intestine in bile, metabolized by bacteria, and excreted in feces. Circulation Food nutrients are absorbed from intestine and enter blood. Raw materials are made available in blood for erythrocyte synthesis. Fate and destruction of RBCs Circulation Erythrocyte disorders Anemias = abnormally LOW oxygen carrying capacity • low RBCs – blood loss, RBC destruction, defective bone marrow • low Hemoglobin content – low iron, B12 deficiency • abnormal hemoglobin – sickle cell Polycythemia = abnormal excess of RBCs • increases blood viscosity • increases blood pressure Can be due to disease, high altitude or blood doping Leukocytes • Granulocytes = have cytoplasmic granules – Basophils – release histamine (inflammation); contain heparin (anticoagulant) – Neutrophils – phagocytize bacteria – Eosinophils –role in allergies and asthma •Agranulocytes = lack cytoplasmic granules •Monocytes – phagocytize foreign invaders •Lymphocytes – involved in immune response Leukopoiesis – formation of WBCs Leukemia – abnormally high WBC count of abnormal WBCs Leukopenia – low WBC count Thrombocytes aka Platelets •Responsible for Blood Clotting Hemostasis Stoppage of blood flow Step 1 Vascular spasm • Smooth muscle contracts, causing vasoconstriction. Step 1 Vascular spasm • Smooth muscle contracts, causing vasoconstriction. Collagen fibers Step 2 Platelet plug formation • Injury to lining of vessel exposes collagen fibers; platelets adhere. Step 1 Vascular spasm • Smooth muscle contracts, causing vasoconstriction. Collagen fibers Platelets Step 2 Platelet plug formation • Injury to lining of vessel exposes collagen fibers; platelets adhere. • Platelets release chemicals that make nearby platelets sticky; platelet plug forms. Chemicals that aid platelet plug formation • Serotonin – Enhances vasoconstriction • Thromboxane – Enhances vasoconstriction – Attracts platelets to the wound What is aspirin, and how does it work? Inhibits thromboxane increases bleeding time Step 1: Vascular spasm • Smooth muscle contracts, causing vasoconstriction. Collagen fibers Platelets Fibrin Step 2: Platelet plug formation • Injury to lining of vessel exposes collagen fibers; platelets adhere. • Platelets release chemicals that make nearby platelets sticky; platelet plug forms. Step 3: Coagulation • Fibrin forms a mesh that traps red blood cells and platelets, forming the clot. Inactive Clotting Factors Collagen exposure Becomes The catalyst Ca+2 Active Clotting Factors Prothrombin Activator Prothrombin Becomes The catalyst Thrombin Fibrinogen Fibrin Fibrin Platelets RBC Figure 17.15 Clot Retraction •Platelets contract within 30–60 minutes •Platelets pull on the fibrin strands pulling ends of wound together Fibrinolysis •Clot dissolving –Takes several days to occur