2011 Provider Seminar - Blue Cross of Northeastern Pennsylvania
advertisement

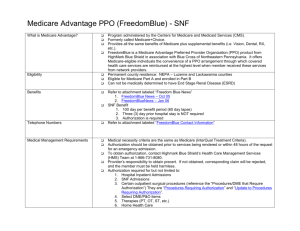
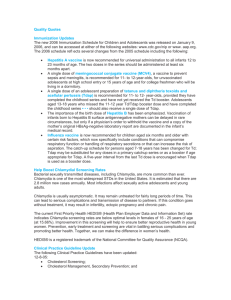
PROVIDER SEMINAR BlueCross of Northeastern Pennsylvania October 5, 2011 WELCOME Jeanne Wisnewski Director, Provider Relations HEALTH PLAN UPDATES Odette Ashby Provider Relations Consultant Updates BlueCross of Northeastern Pennsylvania BCNEPA Updates Radiology Management Program • Effective with date of service November 1, 2011, prior authorization through NIA is required for select nonemergent, advanced outpatient radiology services • All professional offices or free-standing radiology providers who perform these select studies must be privileged by NIA for BCNEPA • Excludes services performed in emergency room, observation, inpatient and qualified contracted urgent care centers BCNEPA Updates Radiology Management Program • Applies to FPLIC and FPH Group Products and CHIP • Does NOT apply to self-funded groups or individual products • In Luzerne County, the existing capitated radiology program still applies for FPH members BCNEPA Updates Radiology Management Program • Ordering physician is responsible for OBTAINING authorization • Luzerne County members whose PCP is part of the Cap Rad program must still be directed to the capitated provider for CT, CTA, CCTA • Rendering providers should VERIFY that authorization has been obtained BCNEPA Updates Radiology Management Program • Applies to the following studies: • Nuclear Cardiology • Stress Echo Cardiology Procedures • CT/CTA/CCTA* • MRI/MRA* • PET Scans* * Continue to call BCNEPA to request authorization for select services for individual members and self-funded accounts BCNEPA Updates Radiology Management Program-Privileging • Establishes consistent standards for all diagnostic imaging services • Establishes minimum participation guidelines – Facility accreditation – Equipment capabilities – Physician and technologist education, training and certification – Procedures for handling emergencies – Radiation safety guidelines BCNEPA Updates Radiology Management Program Training will be offered via webinar on the following dates: • October 18, 2011 • October 19, 2011 • October 20, 2011 • October 25, 2011 • October 27, 2011 There will be 2 hour-long webinars each day – 8:00 am and 12:00 pm To register, contact NIA at 1-800-327-0641 at least one week prior to the session you wish to attend BCNEPA Updates Radiology Management Program Complete information is available at the BCNEPA Provider Center Select “Resources and Tools” Select “BCNEPA NIA Radiology Management Program” Quick Reference Guide for Facilities Quick Reference Guide for Ordering Physicians FAQ’s BCNEPA Updates New Products – Offered August 1, 2011 • AffordaBlue • BlueCare QHD EPO – Developed to: Provide new products with reduced premiums Significantly reduce out of network utilization to keep healthcare $$ and services in our service area Position our portfolio for healthcare reform BCNEPA Updates AffordaBlue – Alpha Prefix - QFZ – 3 Levels (Tiers) of Benefits 1. Custom PPO Network (FPLIC PPO network plus Lehigh Valley, Berwick, Bloomsburg providers and Bon Secours Hospital 2. Hospitals that charge a facility fee for an outpatient visit with a hospital based physician and whose costs exceed specific thresholds 3. BlueCard PPO Network BCNEPA Updates AffordaBlue • Member Cost Sharing –$ Tier 1 Provider = lowest cost – $$ Tier 2 Provider = median out-of-pocket cost – $$$ Tier 3 Provider = highest out-of-pocket cost • Separate deductible and co-insurance applies to each tier • Services rendered by non-network providers are covered for emergency services only BCNEPA Updates AffordaBlue Key Benefit Features • No PCP selection is required • No Referrals • Deductible/co-insurance plan design – no co-pays • Prescription coverage is offered as a rider Multi-tiered Generic-based BCNEPA Updates AffordaBlue Key Benefit Features • Benefits are applied based on the provider’s network participation • Preventive services are covered without cost-sharing at the Tier 1 and Tier 2 providers • Member will be liable for costs associated with services provided by Tier 2, Tier 3, and nonparticipating providers even if the service is not available from a Tier 1 provider. • No coverage is provided for non-emergency services rendered by a non-network provider BCNEPA Updates BlueCare QHD EPO • Alpha Prefix – QFI • Two Tiers of Benefits 1. Current FPLIC EPO Network (FPLIC PPO Network plus Lehigh Valley, Berwick, Bloomsburg providers and Bon Secours Hospital) 2. BlueCard PPO Network BCNEPA Updates BlueCare QHD EPO • Member Cost Sharing – $ Tier 1 Provider = lowest cost – $$ Tier 2 Provider = highest out-of-pocket cost • Separate deductible and co-insurance applies to each tier • Deductible and out-of-pocket maximums must differ in each tier • Services rendered by non-network providers are covered for emergency services only BCNEPA Updates BlueCare QHD EPO • No PCP selection is required • No Referrals • Deductible/co-insurance plan design – (no co-pays except for prescriptions) • Integrated Prescription Drug Benefit BCNEPA Updates BlueCare QHD EPO • Benefits are applied based on the provider’s network participation • Preventive services are covered without cost-sharing at Tier 1 providers • Member will be liable for costs associated with services provided by Tier 2 and non-participating providers even if the service is not available from a Tier 1 provider. • No coverage is provided for non-emergency services rendered by a non-network provider BCNEPA Updates Security 65 Processing After Medicare Exhausts • Claim must be submitted on an original red and white UB-04 claim form • Report the applicable occurrence codes and dates in locator #31 – A3 Benefits Exhausted, Payer A – B3 Benefits Exhausted, Payer B – 24 Date Insurance Denied See October, 2011 Provider Bulletin BCNEPA Updates • Medicare Part B claim must be billed to Medicare prior to submitting the Medicare exhaust claim to BCNEPA Include the Medicare EOMB with the paper claim • Written documentation of the Medicare allowed amounts must be attached to the form (i.e. a screen print from the Medicare system showing the amount they would allow) • Submit claims to: BCNEPA Claims P.O. Box 890179 Camp Hill, PA 17089-0179 BCNEPA Updates Home Health Precertification Requests • The Home Health Initial Precertification Worksheet has been updated and now requires an explanation of member’s homebound status. The worksheet is located on our Provider Center • Precert must be requested prior to assessing the patient or rendering services • Retro requests must be submitted within 5 days of the start of services BCNEPA Updates Utilization Management Department • Complete ALL fields on request forms • Check the monthly Provider Bulletin for updates to processes throughout 2011 • Precertification requests may now be e-mailed directly to our Utilization Management Department through a secure, confidential e-mail address: umreviews@bcnepa.com • Current Focus PAC listings for FPLIC, EPO and BC (Non-FPLIC) lines of business are available on our Provider Center BCNEPA Updates Provider Claim Issues For providers without NaviNet access, ALL claim inquiries, reconsiderations and research requests must be initiated through the appropriate Blue Cross of Northeastern Pennsylvania (BCNEPA) address or by contacting the appropriate customer service department * Claim issues directed to any other area may result in a delay in responding to your request BCNEPA Updates • All written Blue Cross/FPLIC claim issue requests must be sent to: Claims PO Box 890179 Camp Hill, PA 17089-0179 • Continue to use the Claims Research Request Form and send FPH claim issue requests to: BlueCare HMO 19 N. Main St. Wilkes-Barre, PA 18711 BCNEPA Updates Provider Bulletins • Be sure to review/print the monthly provider bulletin from the BCNEPA Provider Center; this can be accessed via NaviNet or www.bcnepa.com • For those providers with NaviNet access, there is a monthly Blue Alert message indicating the current bulletin is now available BCNEPA Updates Provider Center Our Re-designed BCNEPA Provider Center is your resource for important information and updates. Please check the Provider Center site via NaviNet or www.bcnepa.com prior to contacting us for bulletins, forms, policies, manuals, etc. BCNEPA Updates BCNEPA Updates BCNEPA Updates BCNEPA Updates BCNEPA Updates BCNEPA Updates Highmark Blue Shield Updates Highmark Blue Shield Updates Authorization Requirement Update • 15 new codes added to authorization list effective October 3, 2011 • Applies to Direct Blue (group only) and Freedom Blue PPO • Highmark-sponsored NaviNet should be used to request authorization for services See Special Bulletin dated June 23, 2011 for a complete list of codes Highmark Blue Shield Updates Reimbursement Changes Approved • Increases to specific services effective 7/1/11 • Minimal number of codes decreased effective 9/26/11 • Payment differential updated for E&M services performed in a facility vs. non-facility effective 9/26/11. Highmark Blue Shield Updates Reimbursement Changes • Fee information is available via Highmark’s NaviNet From the Plan Central Menu, select Allowance, then select Allowance Inquiry to view pricing for specific procedure codes by plan or product type OR Use “Provider Center/Medical and Claims Payment Guidelines/ Fee Modification” to view the complete list of adjustments Highmark Blue Shield Updates Technical Component Multiple Procedure Payment Reductions • Two or more services on contiguous body parts, same patient, same day • Effective 9/26/11, the highest priced procedure is paid in full • Payment reduction of 50% will be applied to the technical component allowance of each additional procedure • See PRN dated June, 2011 for list of affected procedure codes Highmark Blue Shield Updates Elimination of Paper Initiative • Phase I: Effective 10/01/10, all new assignment accounts and new practitioners are automatically enrolled in Highmark’s NaviNet, paperless EOB’s, and EFT • Phase II: By 6/30/11, all current NaviNet-enabled practitioners will be required to enroll in paperless EOB’s and EFT • Phase III: By 12/31/11, all practitioners doing business with Highmark will be required to enroll in NaviNet, paperless EOB’s and EFT IMPORTANT NOTE: Change in banking information or authorized person requires completion of a new form. Highmark Blue Shield Updates Reminder: Paper versions of the Policy Review and News (PRN) and Behind the Shield publications have been eliminated. Each issue of the newsletters is posted online in the Provider Resource Center • PRN contains medical policies • Behind the Shield is bimonthly newsletter • Special Bulletins are a companion to the above regularly scheduled periodicals and will still be issued • Consider enrolling in E-subscribe Highmark Blue Shield Updates Credentialing & Recredentialing • Effective October 17, 2011, CAQH will be the sole credentialing/recredentialing system for Highmark • Paper will be accepted until 10/16/11 • If no internet access, contact CAQH Help Desk at 1-888-599-1771 for other options Highmark Blue Shield Updates Prescription Drug Formulary • Updated quarterly via Special eBulletin • eBulletins are available on-line at: Highmark’s Provider Resource Center NaviNet Plan Central • Walgreen’s Specialty Pharmacy (formerly MedMark) exclusive provider for self-administered injectables or oral biotechnology drugs Highmark Blue Shield Updates Medicare Advantage Updates Global Surgery Period • Highmark adopted CMS global surgery values of 0 (zero) and 90 (ninety) days in 1999 • 10-day post-op was not recognized due to system limitations and 0 (zero) was used • Effective 7/22/11, Highmark recognizes a 10-day post-op period for Freedom Blue Members only Medicare Advantage Updates Medicare Advantage PPO Network Sharing • A reminder that all “Blue” Medicare Advantage PPO Plans are participating in reciprocal network sharing • The “MA” in the suitcase on the member’s card will help you identify these members • Providers should always check the out-of-area member’s benefits via the Blue Exchange transaction on NaviNet, or by calling the BlueCard eligibility line – 1-800-676-BLUE Medicare Advantage Updates Medicare Advantage PPO Claim Submission • Submit all Medicare Advantage claims to Highmark. – Electronic claims are to be submitted directly to Highmark via trading partner agreement (TPA) with 378 plan code / NAIC # 54771C – To establish a TPA, visit Highmark’s Provider Resource Center, Electronic Data Interchange (EDI) Services and complete the request on-line – Paper Claims: FreedomBlue PPO Claims PO Box 890062 Camp Hill, PA 17089-0062 Medicare Advantage Updates National Correct Coding Initiative (NCCI) • Developed by CMS to prevent improper payment when incorrect code combinations are reported • NCCI edits will be applied to all Freedom Blue claims received on or after 10/15/11 Medicare Advantage Updates • CMS rates Medicare Advantage plans annually • Results are posted using a “star” hotels, cars, and other services score similar to • Allows Medicare beneficiaries to compare plan options when choosing a Medicare Advantage plan • Highmark Freedom Blue received a four star rating! Medicare Advantage Updates Annual Wellness Visit Covered • Extends the Initial Preventive Personal Examination (IPPE), also known as the “Welcome to Medicare Visit” • AWV is NOT covered during the first 12 months of beneficiary’s initial enrollment in Medicare • Medicare has provided a physician quick reference for the AWV Medicare Advantage Updates Advanced Illness Services Program • Provides 100% coverage for 10 comprehensive, interdisciplinary visits by appropriately accredited hospice providers • This benefit is in addition to the hospice benefit Medicare Advantage Updates Advanced Illness Services Program • Members may receive services in their home or in a healthcare facility • Members are not required to be homebound or meet a skilled level of care to be eligible for services • “AIS” page has been added to Provider Resource Center Medicare Advantage Updates Wheelchair Van Transportation Benefit • Covers trips to medical appointments if provided by a wheelchair van when: Medicare’s medical necessity criteria are met, and Billed with the appropriate HCPCS modifiers indicating a medically acceptable origin and destination Medicare Advantage Updates Wheelchair Van Transportation Benefit • Wheelchair van transportation is not separately reimbursable when the member is in a covered Part A inpatient stay in an acute care hospital, LTAC or SNF. Medicare Advantage Updates NaviNet Enhancements Home Health and Hospice Providers: New NaviNet enhancement will permit home health agencies and hospice providers to submit authorization requests electronically A template for the clinical information has been developed which replaces the free text field See August, 2011 BCNEPA Provider Bulletin for complete information Medicare Advantage Updates NaviNet Enhancements Acute Care Hospitals: Effective 4/18/11, authorizations for transfers from acute care to post-acute care facility should be completed on NaviNet A template for the clinical information has been developed which replaces the free text field See August, 2011 BCNEPA Provider Bulletin for complete information Medicare Advantage Updates Important Changes for Freedom Blue PPO Plans effective Jan 1, 2012 • Annual deductible and out-of-pocket limits decreased for PPO-HD Plan • Member cost-sharing amounts increased for certain services • Quarterly cap on Medicare Part B covered medications eliminated • Determination of refractive state not a covered benefit For additional information see the Special Bulletins dated September, 2011. Questions? HIPAA 5010 / ICD-10 UPDATES Dawn Reece Project Manager, Claims 5010 Updates All HIPAA mandated EDI transactions sent to BCNEPA after December 31, 2011 must be version 5010a1 All HIPAA mandated EDI transactions sent by BCNEPA after December 31, 2011 must be version 5010a1 The following are HIPAA mandated EDI transactions: Professional Claims (837P) Institutional Claims (837I) Remittance Advice (835) Claim Status Inquires & Responses (276/277) Benefit Inquires & Responses (270/271) Request for Authorization (278) What Does This Mean For My Office? • BCNEPA will reject all 4010 transactions received after December 31, 2011 • NaviNet was converted to 5010a1 in July. All transactions conducted through NaviNet are 5010a1 compliant • Emdeon clearinghouse transactions converted to 5010a1 in May • You must be prepared to send your electronic claims in 5010a1 and to receive your Electronic Remittance Advices (ERA/835) in version 5010a1 by 12/31/2011 Conversion Issues • Many practice management and software vendors are sending 4010 claims data to clearinghouses who made the cut over to 5010a1 with BCNEPA, such as Emdeon • The clearinghouse converts the 4010 data received into 5010a1 and then sends it to the payer (BCNEPA) • Significant data gaps between 4010 and 5010a1 cause this conversion to result in claims rejected by the payer (BCNEPA) for missing or invalid data Example: 5010a1 requires the related surgical procedure for all anesthesia services. This data element does not exist in 4010; therefore, can not be sent when 4010 data is converted to 5010a1. The end result is the claim is rejected by BCNEPA for the missing data Data Flow Your Office 5010a1 Claim File Claims Data Transfer Clearing House 2 Clearing House 1 4010 Claim File BCNEPA 4010 to 5010a1 4010 to 5010a1 Conversion Conversion Who Is The Weakest Link? • Everyone in the chain must be using a format that fulfills the 5010a1 data requirements • Many offices do not know that their data is passed to multiple vendors before it gets to its final stop, the payer • Please contact all your vendors to be sure all parties are conducting business in manner that fulfills the 5010a1 data requirements • Do not wait until December 31, 2011 to convert to 5010a1. Your data may pass through several vendors and have many stops before it gets to BCNEPA. It’s possible that 4010 data released prior to 12/31/2011 will not get to BCNEPA in time ICD-10 ICD-9 will no longer be used as of October 1, 2013 • The government mandated the usage of ICD-10 DM and ICD-10 CM effective with dates of service October 1, 2013 • ICD-10 CM replaces both the ICD-9 DM code set used for reporting diagnosis and ICD-9 CM code set used for inpatient procedure code reporting Submission Requirements • The conversion to ICD-10 is based on service date • Please look for further details on ICD-10 billing requirements in future bulletins • Medicare issued MLN Matters bulletin MM7492 on 8/29/2011, which contains ICD-10 submission requirements for Medicare claims How Are ICD-10 Diagnosis Codes Different? The Humorous Side Of ICD-10 The Wall Street Journal recently published an article on ICD-10 that illustrates the complexity of ICD-10 in a humorous way. “Walked Into a Lamppost? Hurt While Crocheting? Help’s on the Way” The full article can be found at http://online.wsj.com/article/SB100014240531119041034045765607427 46021106.html A medical coding company, Find A Code, published a series of YouTube videos which also show the funny side of the level of detail found in ICD-10. The video suite can be found at - www.youtube.com/user/findacode • Example Of Fracture Diagnosis ICD-10: S52 – Fracture of forearm S52.5 – Fracture of lower end of radius S52.52 – Torus fracture of lower end of radius S52.521 – Torus fracture of lower end of right radius S52.521A - Torus fracture of lower end of right radius, initial encounter closed fracture ICD-9: 813.5 – Fracture of radius 813.45 - closed; torus fracture of radius (alone) How Are ICD-10 Procedure Codes Different? ICD-10 PCS Coding Structure 1. Section = The broad procedure category or section where the code is found. 2. Body System = The general physiological system or anatomical region involved. 3. Root Operation = The objective of the procedure, such as bypass, excision, etc. 4. Body Part = The specific anatomical site where the procedure was performed. 5. Approach = The technique used to reach the procedure site, such as open or percutaneous (through the skin) endoscopic. 6. Device = Any device (whether biological, synthetic, therapeutic or mechanical) left in place after the procedure is completed. 7. Qualifier = An additional attribute of the procedure. ICD-10 Impact To Providers • Clinical and administrative system changes • Impacts most of the processes in your practice Pre-patient visit activities such as eligibility checks and prior authorizations Patient visit activities such as documenting the patient’s condition requires more detail for the coder to choose an ICD-10 diagnosis code Post visit activities such as claim form changes and coding ICD-10 Impact To Providers • The change in code sets requires a major change in clinical documentation requirements • Significant training and changes in procedures would be necessary to support this change • Continuing to code the “unspecified” versions of a diagnosis will at best delay reimbursement • The ICD-10 documentation requirements increase the amount of time and effort that practices spend on each patient encounter • This is not a temporary decrease in productivity due to learning a new code set and does not just impact the coding staff. This increase is permanent and may warrant additional staff • The points above are based on the Nachimson Advisor’s report on IC9-10 impact to providers • The full report can be found at: http://nachimsonadvisors.com/Documents/ICD-0%20Impacts%20on%20Providers.pdf Learning The ICD-10-CM System • It is important to become aware of the various coding concepts related to ICD-10-CM and to recognize the differences from ICD-9-CM • Clinical AND coding professionals should review the ICD10-CM information Center for Disease Control (CDC) /National Center for Health Statistics Web site (NCHS) http://www.cdc.gov/nchs/icd/icd10cm.htm • Training for all staff, including physicians and other clinicians is necessary What Can I Do To Prepare? • Begin talking to your vendors • Raise awareness of ICD-10 in your clinical office • Train clinical staff on ICD-10 coding so they fully understand how to change their clinical documentation for the billing staff to correctly report the service/diagnosis • Take a sample of your existing charts and try to find an ICD-10 diagnosis for them. You will quickly see the gaps Discussion and Comments NAVINET UPDATES Becky Krasson EDI Specialist NaviNet Enhancements for HIPAA 5010 In July 2011, the HIPAA 5010 mandates were implemented in NaviNet by BCNEPA. With this implementation, most of the transactions were updated to accommodate these changes. NaviNet is no longer maintaining transactions utilizing the 4010A1 format The following slides are intended to show the new features and functionality when accessing the transactions On the Patient Search screen, the “Subscriber/Dependent” labels have been renamed “Patient” A description is now required for Not Otherwise Classified, Not Elsewhere Specified or Unlisted procedure codes Blue Exchange Authorization Submission Updates Prior Authorization Submission New Feature: Patient Event Information One of these sections is required in order to submit a Blue Exchange Prior Authorization Transactions to enhance your office output Facility Report Options Professional Report Options Claim Submission Reports – Display on NaviNet the next day Customer Support is the source to locate all BCNEPA updates recently added to NaviNet Transactions Updated on July 1, 2011 BCNEPA NAVINET EXPANSION Kevin Quaglia Project Manager, Provider Relations BCNEPA NaviNet Expansion NaviNet Expansion Split Into Two Phases: • Phase I - BCNEPA NaviNet granted to all providers currently NaviNet enabled through another Health Plan • Phase II - BCNEPA NaviNet available to remainder of BCNEPA Provider Network As of June, 2011: • 20% of BCNEPA’s provider network (573 provider entities) had access • 80% of BCNEPA’s provider network (2295 provider entities) did NOT have access As of September, 2011: • 53% of BCNEPA’s provider network (1522 provider entities) have access • 47% of BCNEPA’s provider network (1346 provider entities) do NOT have access BCNEPA NaviNet Expansion Phase I: July-August 2011 – BCNEPA NaviNet granted to any provider who was NaviNet enabled through another Health Plan Impacted providers notified via a message on their NaviNet Home Page All NaviNet “users” for each provider were notified of BCNEPA NaviNet expansion via email – Any Provider who currently has NaviNet access through another Health Plan who did not receive notification of BCNEPA NaviNet access should contact BCNEPA Provider Relations BCNEPA NaviNet Expansion Phase II: September-December 2011 • BCNEPA NaviNet now available to ALL providers who do not have NaviNet through any other Health Plan • NaviNet training opportunities (on-site, webinars) available by BCNEPA Provider Relations once NaviNet set-up is complete BCNEPA NaviNet Expansion Providers must provide the following information to BCNEPA via e-mail: BCNEPANavi@bcnepa.com to finalize NaviNet set up: Provider/Group/Facility Name, Tax Id Number, and Type II NPI FPH/FPLIC Legacy Number(s) Security Officer contact name, phone number, and e-mail address For professional groups, list all physicians within the group and provide their NPI and FPH/FPLIC legacy numbers Refer to August and September Provider Bulletins THE MEDICAL HOME NEIGHBORHOOD BCNEPA Medical Director, Quality Improvement, Disease/Case Management, Behavioral Health MEDICAL HOME CONCEPT Thomas Curry, MD Medical Director, Network Management and Provider Operations Health Care System Realities • Rising Health Care Costs • Rising Cost of Insurance • Questionable Quality • Poorly Coordinated Care • Burden of Uninsured • Cost Shifting • General Dissatisfaction • Primary Care in Crisis Chronic Care Model • Concept formulated and advanced by Edward H. Wagner, M.D. • Focus on delivery of primary care to patients with chronic illness – Comprehensive – Coordinated – Continuous Chronic Care Model The six key components include: 1. Self-Management Support 2. Delivery System Design 3. Decision Support 4. Clinical Information Systems 5. Community Partnerships 6. Quality Improvement Incentives Medical Home • Personal Physician • Physician-Directed Teams • Whole Person Orientation • Coordinated/Integrated Care • Enhanced Access • Quality and Safety • Appropriate Reimbursement Medical Home Quality and Safety – Care Planning involves medical team, patients, and patient’s family – Evidence-based clinical decision support tools – Use of Information Technology – Practice redesign – Performance measurement – Continuous Quality Improvement Core Concepts Team building Improve care management Self-management support at every encounter Planned visits Improved coordination with specialty and inpatient care Patient-Centered Medical Home Neighborhood Recognizes the importance of collaboration with specialty and subspecialty practices Ensures effective communication with PCMH practices Ensures appropriate and timely consultations and referrals PROCESS IMPROVEMENT Cathy Gorski, BS, MSHA, RN, CCM Manager, Quality Management and Quality Improvement Transitions In Care "Care transitions is a team sport, and yet all too often we don't know who our teammates are, or how they can help.” ~ Eric A. Coleman, MD, MPH • Actions designed to ensure the coordination and continuity of health care as patients transfer between different locations or different levels of care • Consider: – Post inpatient and ER telephonic outreach and in-office visit – Bi-directional communication with specialty providers on patient plan of care – Coordination with specialty and ancillary providers to ensure medication reconciliation and adherence to follow-up recommendations Planned Visits & Care Coordination • Planned Visits: – Pre-visit plan to ensure labs/testing results available – Patient screening prior to each visit for medication changes and other health providers seen – Patient dashboard • Care Coordination: – Develop feedback loop with IP/OP providers to get timely status on patient – Community Resources – Payor processes/contacts to ensure appropriate utilization of benefits/services Care Management Center for Health Care Strategies: • The goal of care management is to achieve an optimal level of wellness and improve coordination of care while providing cost effective, non-duplicative services. • Engage the patient and their support system in a collaborative process to manage their medical/social/mental health conditions effectively Components: – Identification and prioritization – Intervention – Evaluation – Payment/Financing Self-Management Support • Self-management support is what health care practitioners provide to assist a person with their selfmanagement practices, and to support their self efficacy and ability to effectively self-manage • AAFP recommendations for offices: – Motivational Interviewing – Address goal setting and problem solving in each visit – Provide self-management education – Refer patient to community or health plan support programs – Follow-up plan/tracking using telephone/e-mail or other contact with nurse as a way to improve blood sugar control and weight loss in patients with diabetes Continual Process Improvement • Small Steps, Big Concepts – – – – – – Transitions in Care Medication Reconciliation Planned Visits Coordination of Care Care Management Chronic Care Self-Management • Team approach to improved patient outcomes and satisfaction CPI: Model For Improvement Three Questions: 1. What are we trying to accomplish? 2. How will we know that a change is an improvement? 3. What changes can we make that will result in an improvement? Plan-Do-Study-Act DISEASE MANAGEMENT CASE MANAGEMENT Donna Koepfler, RN, BS, CCM Manager, Case Management Blue Health Solutions We help individuals at every level of need Healthy Acute Chronic Catastrophic Nurse Call Line; On-line Portal; Health Care Reminders; Education; Advocacy Wellness Programs HIGH RISK LOW RISK Health Coaching/ Intermediate Care Disease Management Case Management/Transition of Care Clinical Intensity Wellness & Lifestyle Management Programs • Designed for members interested in making changes to their current lifestyle or in getting support or information to continue making healthy choices Wellness & Lifestyles Management Blood Pressure Cholesterol Management Diet Exercise GERD Healthy Back Metabolic Syndrome • Provides individualized education and support, self-management tools and phone access to Health Coaches Nutrition Maternity Management Stress Management Tobacco Cessation Weight Management Disease Management • Integrated management of comorbidities, use of evidence-based guidelines, individualized care plans • Supports the physician’s plan of care including registry with gaps-in-care, alerts and feedback on progress to goals • Focus on prevention and early detection of complications, education and development of care plans Diseases and Conditions Asthma Chronic Obstructive Pulmonary Disease (COPD) Cardio-Vascular Disease (CVD) Depression Diabetes Heart Failure Case Management Catastrophic Case Management • Require high-tech or extensive home care • Are terminally ill • Have sustained traumatic injury • Require frequent hospital admissions • Have chronic illnesses with complications • Require extensive discharge planning • Require coordination of benefits and/or services • Have an extended LOS Intermediate Care Management • Chronic, long-term illness that may include multiple sclerosis, rheumatoid arthritis, renal disease, migraines Transition of Care • Planning for an elective surgery • Recovery from surgery 24/7 Nurse Now • Access to medical information 24 hours a day 7 days a week • Members are referred to Blue Health Solutions programs from Nurse Now Blue Health Solutions Is Here To Help! • We are here to act as an extension of your office when self-management assistance, patient education, and support navigating the health care system will make a difference. • Just call…. Triage Nurse Health Management 1-866-262-4764 Case Management 1-800-346-6149 BEHAVIORAL HEALTH Susan Ferry, LCSW Clinical Care Manager, CBHNP Behavioral Health Care • Mental illness…a scary thought • The reality & prevalence of mental illness • Statistics • Help is available Mental Illness…A Scary Thought Mental illness refers collectively to all of the diagnosable mental disorders. When the average person hears the phrase mental illness, they conjure up images of a person being tortured by demons only he sees or by voices no one else hears. This, of course, comes from the TV & movie versions of mental illness which often rely on the extraordinary symptoms of psychotic illnesses like schizophrenia. “ There is someone in my head but it’s not me”. Pink Floyd The Reality & Prevalence Of Mental Illness • Few mental illnesses have hallucinations as symptoms. The reality is that the most prevalent mental health illnesses are anxiety disorders, depression and substance abuse. The good news is that they are among the most treatable of the psychiatric illnesses. • Anyone, no matter what age, economic status or race can develop mental illness. During any one year, more than 22% of the adult population suffers from a clearly diagnosable mental disorder. The Reality & Prevalence Of Mental Illness • • • • • • • • • • • • • • • Isaac Newton Beethoven Abe Lincoln Winston Churchill Jane Pauley Betty Ford Carrie Fisher Vivien Leigh Bette Midler Patty Duke Ernest Hemingway Marlon Brando Howie Mandel Jim Carrey Charles Dickens Statistics • Some 8 to 14 million Americans suffer from depression each year • As many as 1 in 5 Americans will suffer at least one episode of major depression during their lifetime • 6% - 9% of older Americans in the primary care setting suffer from major depression • Women are 70% more likely than men to experience depression during their lifetime • Depression very often co-occurs with other medical illnesses and conditions such as cancer, stroke, heart attack and diabetes Statistics Almost any medical condition can trigger a mental health issue (i.e. celiac disease can lead to depression & symptoms of an eating disorder). Vincent Van Gogh, a Dutch post–impressionist painter, suffered from a lifetime of mental illness, anxiety, depression (possibly bi-polar disorder) and ultimately committed suicide at age 37. Statistics • Suicide is the 3rd leading cause of death for people between the ages of 15 and 24 • Male physicians have a 40% higher rate of suicide than the general population, and a whopping 130% for female physicians • 15.4 million American adults and 4.6 million adolescents experience serious alcohol-related problems • 12.5 million Americans suffer from drug abuse or dependence Statistics • 20% of the ailments for which Americans seek a doctor’s care are related to anxiety disorders, such as panic attacks, that interfere with the ability to live normal lives • Women are 60% more likely than men to experience an anxiety disorder • Nearly ¼ of the elderly who are labeled as senile actually suffer some form of mental illness that can be effectively treated Statistics • Only a small fraction of those who suffer from mental illness ever receive mental health treatment • Of those patients who do receive treatment, 80%-90% of them will respond positively Help Is Available Community Behavioral Network of Pennsylvania 1-800-599-2428 CBHNP is a managed care company who Blue Cross has contracted with to provide triage, referral and utilization management for behavioral health. We have licensed behavioral health clinicians available 24 hours a day and 7 days a week to help with referrals to behavioral health specialists. MEDICAL HOME NEIGHBORHOOD Thomas Curry, MD Medical Director, Network Management and Provider Operations Specialists •Transition of care information • Behavioral health integration PCMH •Problems list •Medication list BCNEPA •Office Transformation •Reports •Treatment •Care Coordination •Tracking •Education •Care Coordination (Onsite & Telephonic) •Admission & Discharge Info (Inpatient & ER) •Onsite UM •Discharge Information & •Follow-up Plan Patient •Discharge Information & •Follow-up Plan •CM •DM •Wellness •Member Portal •24-hour Nurse Line HMS-BHS Hospitals •Discharge Planning THANK YOU “Your feedback is important to us. Please take a moment to complete our survey.”