Urinary System
advertisement

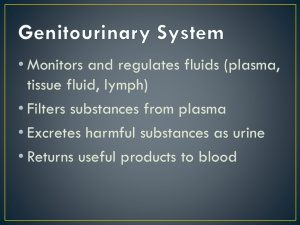
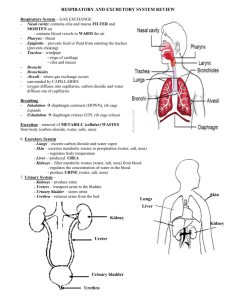
Overview of the Urinary System The urinary system has three major functions: (1) excretion, the removal of organic waste products from body fluids (kidneys) (2) elimination, the discharge of these waste products into the environment, and (bladder and urethra) (3) homeostatic regulation of the volume and solute concentration of blood plasma. Other functions Regulating blood volume and blood pressure, by adjusting the volume of water lost in urine. Regulating plasma concentrations of sodium, potassium, chloride, (electrolytes) and other ions, by controlling the quantities lost in urine. Helping to stabilize blood pH, by controlling the loss of hydrogen ions and bicarbonate ions in urine. Conserving valuable nutrients, by preventing their excretion in urine while excreting organic waste products. Assisting the liver in detoxifying poisons. These activities are carefully regulated to keep the composition of blood within acceptable limits. Kidneys The kidneys are located on either side of the vertebral column, between vertebrae T12 and L3. The left kidney lies slightly superior to the right. The superior surface of each kidney is capped by an adrenal gland. A typical adult kidney is reddishbrown and about 10 cm long, 5.5 cm wide, and 3 cm thick. Each kidney weighs about 5.25 oz. The hilum, a prominent medial indentation, is the point of entry for the renal artery and renal nerves, and the point of exit for the renal vein and the ureter. Kidney function Urine production begins in microscopic, tubular structures called nephrons kidneys receive 20–25 percent of your total cardiac output Each kidney receives blood through a renal artery Controled by sympathetic innervation (1) adjusts rates of urine formation by changing blood flow and blood pressure at the nephron (2) stimulates the release of renin, which ultimately restricts losses of water and salt in the urine Principles of Renal Physiology The goal of urine production is to maintain homeostasis by regulating the volume and composition of blood. Involves the excretion of solute waste products: Urea: is the most abundant organic waste. You generate roughly 21 g/day, most of it through the breakdown of amino acids. Uric Acid: a waste product formed during the recycling of the nitrogenous bases from RNA molecules. You produce approximately 480 mg of uric acid each day. Principles of Renal Physiology Creatinine: is generated in skeletal muscle tissue through the breakdown of creatine phosphate, high-energy compound that plays an important role in muscle contraction. Your body generates roughly 1.8 g of creatinine/day, and virtually all of it is excreted in urine. Principles of Renal Physiology These waste products are dissolved in the bloodstream and can be eliminated only while dissolved in urine. As a result, their removal is accompanied by an unavoidable water loss. The kidneys also ensure that the fluid that is lost does not contain potentially useful organic substrates that are present in blood plasma, such as sugars or amino acids. These valuable materials must be reabsorbed and retained for use by other tissues. Basic Process of Urine Formation The kidneys rely on 3 distinct processes: Filtration: blood pressure forces water and solutes across the wall of the capillaries and into the capsular space. Solute molecules small enough to pass through the filtration membrane are carried by the surrounding water molecules. Reabsorption: removal of water and solutes from the filtrate. Most of the reabsorbed materials are nutrients the body can use. Whereas filtration occurs solely based on size, reabsorption is a selective process involving either simple diffusion or the activity of carrier proteins. Water reabsorption occurs passively, through osmosis. Secretion: transport of solutes. Secretion is necessary because filtration does not force all the dissolved materials out of the plasma. Tubular secretion, which provides a backup process for filtration, can further lower the plasma concentration of undesirable materials. Secretion is often the primary method of excretion for some compounds, including many drugs. Composition of Urine More than 99 percent of the 180 liters of filtrate produced each day that is reabsorbed and never reaches the renal pelvis. The composition and concentration of urine are two related but distinct properties. composition of urine reflects the filtration, absorption, and secretion activities of the nephrons. Some compounds (such as urea) are neither actively excreted nor reabsorbed along the nephron. Organic nutrients are completely reabsorbed, and other compounds, such as creatinine, that are missed by the filtration process are actively secreted into the tubular fluid. The concentration of these components in a given urine sample depends on the osmotic movement of water. Composition of Urine Normal urine is a clear, sterile solution. Its yellow color results from the presence of the pigment urobilin, generated in the kidneys from the urobilinogens produced by intestinal bacteria. The evaporation of small molecules, such as ammonia, accounts for the odor of urine. Other substances not normally present, such as acetone or other ketone bodies, can also impart a distinctive smell. Urine Transport Filtrate modification and urine production end when the fluid enters the renal pelvis. The urinary tract (the ureters, urinary bladder, and urethra) is responsible for the transport, storage, and elimination of urine. The sizes of the minor and major calyces, the renal pelvis, the ureters, the urinary bladder, and the proximal portion of the urethra are somewhat variable, because these regions are lined by a transitional epithelium that can tolerate cycles of distension and contraction without damage. The ureters are a pair of muscular tubes that extend from the kidneys to the urinary bladder—a distance of about 30 cm (12 in.). Urine Storage The Urinary Bladder: a hollow, muscular organ that functions as a temporary reservoir for the storage of urine. The dimensions of the urinary bladder vary with its state of distension, but a full urinary bladder can contain as much as a liter of urine. The smooth muscle fibers of this sphincter provide involuntary control over the discharge of urine from the bladder. Urination In females, the urethra is very short, from the bladder to the external urethral orifice near neck of the urinary bladder to the anterior wall of the vagina. the exterior of the body. In both sexes, where the urethra In males, the urethra extends passes through a circular band from the neck of the urinary of skeletal muscle called the bladder to the tip of the penis. external urethral sphincter. The male urethra can be This muscular band acts as a subdivided into three valve. portions: prostatic urethra, The external urethral sphincter, membranous urethra, and which is under voluntary spongy urethra. control has a resting muscle tone and must be voluntarily relaxed to permit micturition (peeing) The Urethra: extends from the Urination Urine reaches the urinary bladder by peristaltic contractions of the ureters. The process of urination is coordinated by the micturition reflex. Stretch receptors in the wall of the urinary bladder are stimulated as the bladder fills with urine. The urge to urinate generally appears when the bladder contains about 200 ml of urine. Infants lack voluntary control over urination, because the necessary spinal connections have yet to be established. Incontinence is the inability to control urination voluntarily. Trauma to the internal or external urethral sphincter can contribute to incontinence in otherwise healthy adults. Aging and the Urinary System In general, aging is associated with an increased incidence of kidney problems. Age-related changes in the urinary system include the following: A Decline in the Number of Functional Nephrons. Problems with the Micturition Reflex. Three factors are involved in such problems: (1) The sphincter muscles lose muscle tone and become less effective at voluntarily retaining urine. This leads to incontinence, often involving a slow leakage of urine. (2) The ability to control micturition can be lost after a stroke, Alzheimer’s disease, or other CNS problems affecting the cerebral cortex or hypothalamus. (3) In males, urinary retention may develop if enlargement of the prostate gland compresses the urethra and restricts the flow of urine. Excretory Systems The urinary system is not the only organ system involved in excretion. The urinary, integumentary, respiratory, and digestive systems are an anatomically diverse excretory system whose components perform all the excretory functions that affect the composition of body fluids: Integumentary System. Water and electrolyte losses in sensible perspiration can affect the volume and composition of the plasma. The effects are most apparent when losses are extreme, such as during peak sweat production. Small amounts of metabolic wastes, including urea, also are eliminated in perspiration. Respiratory System. The lungs remove the carbon dioxide generated by cells. Small amounts of other compounds, such as acetone and water, evaporate into the alveoli and are eliminated when you exhale. Digestive System. The liver excretes small amounts of metabolic waste products in bile, and you lose a variable amount of water in feces. These excretory activities have an impact on the composition of body fluids. Fluid Balance Most of your body weight is water: up to 99 percent of the volume of the fluid outside cells, and it is an essential ingredient of cytoplasm. Water accounts for roughly 60 percent of the total body weight of an adult male, and 50 percent of that of an adult female. This difference between the sexes primarily reflects the proportionately larger mass of adipose tissue in adult females, and the greater average muscle mass in adult males All of a cell’s operations rely on water as a diffusion medium for the distribution of gases, nutrients, and waste products. If the water content of the body changes, cellular activities are jeopardized. EX. When water content reaches very low levels, proteins denature, enzymes cease functioning, and cells die. To survive, we must maintain a normal volume and composition of both the extracellular fluid or ECF, and the intracellular fluid or ICF. The ionic concentrations and pH (hydrogen ion concentration) of these fluids are as important as their quantities. Volumes and Concentrations Fluid Balance. You are in fluid balance when the amount of water you gain each day is equal to the amount you lose to the environment. The maintenance of normal fluid balance involves regulating the content and distribution of body water in the ECF and the ICF. The digestive system is the primary source of water gains; a small amount of additional water is generated by metabolic activity. The urinary system is the primary route for water loss under normal conditions. Although cells and tissues cannot transport water, they can transport ions and create concentration gradients that are then eliminated by osmosis. Volumes and Concentrations Electrolyte Balance. Electrolytes are ions released through the dissociation of inorganic compounds; they are so named because they can conduct an electrical current in a solution Electrolyte balance primarily involves balancing the rates of absorption across the digestive tract with rates of loss at the kidneys, although losses at sweat glands and other sites can play a secondary role. Acid–Base Balance. You are in acid–base balance when the production of hydrogen ions in your body is precisely offset by their loss. Preventing a reduction in pH is the primary problem, because your body generates a variety of acids during normal metabolic operations. The kidneys play a major role by secreting hydrogen ions into the urine. The lungs also play a key role through the elimination of carbon dioxide. Intracellular vs Extracellular The principal ions in the ECF are sodium, chloride, and bicarbonate. The ICF contains an abundance of potassium, magnesium, and phosphate ions, plus large numbers of negatively charged proteins. If the cell membrane were freely permeable, diffusion would continue until these ions were evenly distributed across the membrane. But it does not, because cell membranes are selectively permeable: Ions can enter or leave the cell only via specific membrane channels. In addition, carrier mechanisms move specific ions into or out of the cell. Intracellular vs Extracellular Despite the differences in the concentration of specific substances, the osmotic concentrations of the ICF and ECF are identical. Osmosis eliminates minor differences in concentration almost at once, because most cell membranes are freely permeable to water. Because changes in solute concentrations lead to immediate changes in water distribution (Na+, Cl) the regulation of fluid balance and that of electrolyte balance are tightly intertwined. when you lose body water, plasma volume decreases and electrolyte concentrations rise. When you gain or lose excess electrolytes, there is an associated water gain or loss due to osmosis. Fluid Movement Water circulates freely within the ECF compartment. At capillary beds, pressure forces water out of plasma and into interstitial spaces. Some of that water is reabsorbed along the distal portion of the capillary bed, and the rest enters lymphatic vessels for transport to the venous circulation. Water Losses. You lose roughly 2500 ml of water each day through urine, feces, and insensible perspiration—the gradual movement of water across the epithelia of the skin and respiratory tract. The losses due to sensible perspiration vary with the activities you undertake. Sensible perspiration can cause significant water deficits, with maximum perspiration rates reaching 4 liters per hour. Fever can also increase water losses. Water Gains. A water gain of roughly 2500 ml day is required to balance your average water losses. You obtain water through eating (1000 ml), drinking (1200 ml), and metabolic generation (300 ml). Gonads, or reproductive organs that produce gametes and hormones. Ducts that receive and transport the gametes. In both males and females, the ducts are connected to chambers and passageways that open to the exterior of the body. The structures involved constitute the reproductive tract. Males The Testes Each testis has the shape of a flattened egg that is roughly 5 cm (2 in.) long, 3 cm (1.2 in.) wide, and 2.5 cm (1 in.) thick. Each has a weight of 10–15 g (0.35–0.53 oz). The testes hang within the scrotum In adult males, the testes, or male gonads, secrete sex hormones called androgens. The testes also produce the male gametes, called spermatozoa, or sperm—one-half billion each day. Spermatogenesis begins at puberty and continues until relatively late in life (past age 70). During emission, mature spermatozoa travel along a lengthy duct system, where they are mixed with the secretions of accessory glands. The mixture created is known as semen Spermatozoa Seminal fluid (prostate) enzymes Female A woman’s reproductive system produces sex hormones and functional gametes, and it must also be able to protect and support a developing embryo and nourish a newborn infant. The principal organs: ovaries, the uterine tubes, the uterus, the vagina, and the components of the external genitalia. Ovaries The ovaries perform three main functions: (1) production of immature female gametes, or oocytes, (2) secretion of female sex hormones, including estrogens and progestins (3) secretion of inhibin, involved in the feedback control of pituitary Follicle Stimulating Hormone production. Oogenesis Ovum production, or oogenesis, begins before a woman’s birth, accelerates at puberty, and ends at menopause. Between puberty and menopause, oogenesis occurs on a monthly basis as part of the ovarian cycle. Ovarian cycle Menses The uterine cycle begins: degeneration of the functional zone of the endometrium. Deprived of oxygen and nutrients, the secretory glands and other tissues in the functional zone begin to deteriorate. Eventually, the weakened arterial walls rupture, and blood pours into the connective tissues of the functional zone. Proliferative Phase: In the days after menses, the epithelial cells of the uterine glands multiply and spread across the endometrial surface, restoring the integrity of the uterine epithelium. Further growth and vascularization result in the complete restoration of the functional zone. The Secretory Phase During the secretory phase of the uterine cycle, the endometrial glands enlarge, accelerating their rates of secretion, and the arteries that supply the uterine wall elongate and spiral through the tissues of the functional zone. ?????