Pulmonary complications post SCI
advertisement

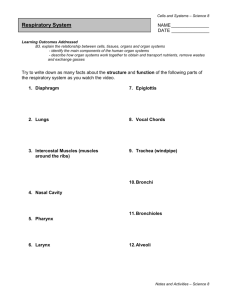
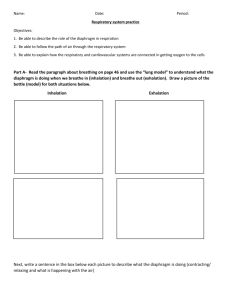
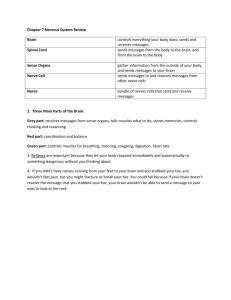
Pulmonary complications post SCI By Melanie Boulet SCI fellow Objectives Mempunyai pengetahuan yang tinggi terhadap : • Anatomi dan fisiologi paru. • Pemeriksaan komplikasi pernafasan akibat SCI • Analisa masalah dan menentukan apa yang dapat dilakukan untuk membantu peningkatan fungsi respirasi. Epidemiology Epidemiology • 67% of acute SCI experience some respiratory complications; – Atelectasis 36% – Pneumonia 31% – Respiratory failure 22.6% • Increased prevalence with: – Age – Level of injury – Completeness of injury Anatomy • Lungs – Trachea = windpipe – Bronchus+bronc hioli = branching of windpipe – Alveoli = air sacs Anatomy • Muscles involved in inspiration – Diaphragm – Intercostal – Accessory muscles • • • • • Scalene, Platysma, Mylohyoid Sternocleidomastoid Trapezius Pectoralis Latissimus dorsi CRANIAL NERVES 12 pairs of nerves from the brain Numbering the Nerves • In classic anatomy we use Roman numerals to number the cranial nerves: • I is one, II is two, III is three, IV is four, V is five, VI is six, VII is seven, VIII is eight, IX is nine, X is ten, XI is eleven and XII is twelve • The modern way of numbering the cranial nerves is by using CN followed by an Arabic number. For example: VIII is written CN 8. I - Olfactory Nerve • • • • Provides sense of smell Damage causes impaired sense of smell Test with coffee grounds, spice not perfume, Why? Test for smell NOT recognition of smell. (Ch. 16) II - Optic Nerve • Provides vision • Damage causes blindness in visual field III - Oculomotor Nerve • Provides eye movement, opening of eyelid • Damage causes ptosis (drooping eyelid), double vision IV - Trochlear Nerve • Moves eye down and out • Damage causes double vision & inability to look down and out VI - Abducens Nerve • Moves eye laterally (ABduction) • Damage results in inability to move eye ______ Innervation of Eye Muscles V - Trigeminal Nerve • Main sensory nerve to face (touch, pain and temperature) and muscles of mastication • Damage produces loss of sensation & impaired chewing or can cause increased pain = trigeminal neuralgia VII - Facial Nerve • Provides facial expressions, sense of taste on anterior 2/3’s of tongue, salivary glands and tear, nasal & palatine glands • Damage produces sagging facial muscles & disturbed sense of taste (missing sweet & salty) called Bell’s Palsy VIII - Vestibulocochlear Nerve • Provides hearing & sense of balance • Damage produces deafness, dizziness, nausea, loss of balance & nystagmus IX - Glossopharyngeal Nerve • Provides control over swallowing, salivation, gagging, sensations from posterior 1/3 of tongue, control of BP and respiration • Damage results in loss of bitter & sour taste & impaired swallowing. X - Vagus Nerve • The wonderer • Provides swallowing, speech, regulation of 2/3 of GI tract • Damage causes impaired voice, swallowing and digestion XI - Accessory Nerve • Contracts upper trap muscles (I don’t know) • Damage causes impaired shoulder movement XII - Hypoglossal Nerve • Provides tongue movements of speech, food manipulation & swallowing • Damage results in inability to protrude tongue, TEST – Stick tongue out and it points right then the _____ XII is broken CN 1- 12 (Summary) (Know the number and the nerve) • On Old Olympus Towering Tops A Famous Vocal German Viewed Some Hops • • • • • • • • • • CN 1- Smells like an old factory. CN2- Two eyes see CN 3, 4, 6- moves the eyes CN 5- Trigeminal, three finger on face CN7- Facial, closes eye lids CN 8 Vestibulocochlear, ear CN 9 Glossopharyngeal, G looks like a nine CN 10 Vagus, two Vs CN 11 Accessory- Trapezius muscle, shoulders up CN 12 Hypoglossal Anatomy • Diaphragm – Phrenic nerve – c3-C4-c5 – Contributes to 65% of Vital Capacity Anatomy • Intercostal – Intercostal nerves – T1-T11 • Both layers act as inspirators at low volumes, and expirators at large volumes Anatomy • Scalene – C4-C8 • Platysma • Mylohyoid Anatomy • Pectoralis • Latissimus dorsi Anatomy • Sternocleidomastoid • Trapezi – Cranial nerve XI Anatomy • Muscles involved in expiration – Abdominal muscles • Recti • Obliques • Transversus-abdomini • Clavicular portion of pectoralis muscle Anatomy • Abdominal muscles – T6-L1 Physiology • What is Breathing? – Movement of air, in and out, through nose or mouth • To get oxygen to feed our tissues • To remove waste product: carbon dioxide Physiology • Inspiration: – Diaphragm contraction becomes flattened moves downward abdominal content creation of negative pressure passive movement of air – Diaphragm in better biomechanical posture if rib cage stabilized by other respiratory muscles Physiology • Expiration: – Passive exit of air after diaphragm relaxation • Forced expiration: – Contraction of abdo muscles increased intraabdominal pressure superior movement of diaphragm expiration and cough – Clavicular portion of pectoralis major can act as expirator in tetraplegia Physiology • Restrictive pulmonary syndrome – Decreased TLC, VC, ERV, FRC – Increased RV • VC of newly injured = 24-31% of predicted – Halo may further restrict VC by up to 8% Physiology • Chronic improvement with: – Improved strenght – Intercostal and abdominal tone • Doubling of VC 3 months after injury for C4-C6 Impairment by level of injury L1 or lower: no impairment T5 to T12: Impairment of forceful ventilation and cough T1-T5: Impairment of quiet respiration C4-C8: Greater impairment of quiet respiration C4: important impairment of quiet respiration C3: usually need ventilation assistance in acute phase C2 and above: no diaphragm function 3 main categories • 1) C2 and above: no funtion of diaphragm, need ventilatory assistance • 2) C3-C4: potential to wean from ventilatory assistance – 83% wean eventually • 3) C5 and below: Breathe without respiratory assistance. Any compromise can result in ventilatory insufficiency. Acute complications • Pneumothorax and chest injuries – From initial injury – From barotrauma – Keeping long-term and short-term risks of treatment in mind, it is recommanded that the patient with a pneumothorax be treated with large tidal volumes (<1000cc) – Risk of barotrauma is small if PIP <40ccH2O • Atelectasis – 40% of high tetras • Pneumonia – Risks: high levels, age, atelectasis – 63% of high tetras Acute complications • Pulmonary embolism – Increased risk • Aspiration – 5% of SCI (13% if > 60yo) – Higher risk: • • • • • • High level Anterior-approach surgery Age Trachestomy Sedation and immobilisation Halo – Cause pneumonia and ARDS Acute complications • Pleural effusion – Atelectasis lower lobe pulls away from diaphragm and parietal pleura space filled by fluid • Empyema – Atelectasis + effusion + pneumonia empyema • Trapped lung – Caused by scarring and fusion of parietal and visceral pleura, or organisation of exsudate in pleural space • Ex: post chest tube • Worse if ventilated at low tidal volumes Acute complications • Respiratory failure – Muscle paralysis – Fatigue of remaining muscles • Abdominal complications – Abdominal distention can prevent diaphragm to descend Acute complications Pulmonary Complications 40.00% 35.00% 30.00% 25.00% 20.00% 15.00% Paraplegia (incomplete) Paraplegia (complete) Tetraplegia (incomplete) 10.00% 5.00% Tetraplegia (complete) 0.00% Aspiration Atelectasis Pneumonia Ventilatory Failure Bad comorbidities • Tobacco – Increases secretions – Increases likelyhood of infection – Decreases clearing capacity • COPD • Narcotics and sleep med. Tests • • • • • • Pulmonary function tests Nocturnal oxymetry Arterial blood gas X-ray Ct-scan Fluoroscopy Tests Management • 3 main issues: –Secretion management • Reduced ability to cough • Unopposed vagal nerve –Atelectasis –Hypoventilation • Weak inspiratory muscles • Unopposed vagal nerve Management • Causes of Problems with secretion management – Acute phase secretion production with unopposed vagal tone – Infection – Poor cough flow • • • • • • • Vital capacity below 1.5 L Weak abdominal muscles Loss glottic control Weakened bulbar muscles Trachestomy Tracheal stenosis COPD Management • Assistance in secretion clearance – Hydration – Limit dairy products? – Postural drainage • Prone • Rotating beds – Chest physical therapy • Chest clapping, percussion, vibration – Suctionning Management – Assisted cough techniques • Improves peak cough flow by 15-33% • Provide max insufflation if VC < 1.5L – Glossopharyngeal breathing can help • Self assist, manually or electrically assist cough – Similar to Heimlich • Contraindications: – – – – Fractured ribs Chest trauma Abdominal complications New IVC (reports of displacement with cardiac compressions) Management – Mechanical assisted cough • Insufflation-exsufflation – Delivery of positive pressure followed by negative pressure » +40 to -40 cm H2O – Especially useful if on noninvasive ventilatory support » Because succionning difficult – Can clear out larger mucus plugs than succion cath and more efficient with left main bronchus – Indicated if VC < 1.5L, or inability to cough or clear secretions – Contrindications: » History of bullous emphysema » Susceptibility to pneumothorax » Recent barotrauma Management • Assistance in secretion clearance – IPV • Vibrations (200cycles/min) with constant pressure – Bronchodilators – Fiberoptic bronchoscopy if large mucus plug • Risk of tracheobronchial irritation, edema, hypoxemia, aspiration Management • Atelectasis prevention and treatment – IPPB • Gradual increase of pressure delivery (15cmH2O to 40 cm H2O) • Can be used to deliver nebulizer treatments – IPP • Nasal or oral interface – BiPAP or CPAP – Incentive spirometry Management • Assistance in ventilation – Muscle training • • • • Inspiratory resistance training Abdominal weights Incentive spirometry and resistive devices Clavicular portion (C5-7) of pectoralis major (expiration) Management • Assistance in ventilation – Positionning of patient • Supine for tetras • Head up for central cords with no diaphragm – Abdominal binder • When in chair • Below rib cage Management – Non invasive ventilation • Glossopharyngeal breathing – Take 6-9 small gulps with thong and pharyngeal muscles – Can help to assist cough and prolong vent-free time if no cuff on trach • Pneumobelt – Good cosmesis – Pump noise, stomach gas, positionning difficulties Management • Assistance in ventilation – Invasive ventilation • High tidal volume to prevent atelectasis – Faster weaning an average 21 days for thoses with Tidal Volume >20ml/kg compare to <20ml/kg – Decreased atelectasis problems (16% vs 52%) • AC prefered to SIMV when weaning – Success in weaning: 68% vs 35% • Many possible complications with invasive ventilation – Nosocomial pneumoniae, mucus plugging, cardiac arrhythmias, accidental disconnection, granulation tissue formation, tracheomalacia, vocal cord paralysis…. Weaning • Prognosis: – Initial VC on admission > 1L Management • Assistance in ventilation – Pharmacology • Mucolytics – Guaifenesin – SSKI – Acetylcysteine » Nebulized or injected in trachea diluted with saline » Tastes like rotten eggs » May cause bronchospasm Management • Pharmacology – Theophylline • • • • • • Relaxes smooth muscles Stimulates medullary respiratory centers Can improve diaphragmatic contractility Can reduce diaphragmatic fatigue Stimulates the release of surfactant Potential deleterious effects: – Arrhytmias – Seizuree – Nausea Management – Pharmacology • Bronchodilators – Long and short acting B-agonist » Offset unopposed parasympathetic stimulation » Reduce inflammation » Stimulate secretion of surfactant – Ipratropium » Theorically blocks effects of parasympathetic stimulation » However, atropine has been shown to block production of surfactant • Smoking cessation program Management • Assistance in ventilation – Electrophrenic pacing • Indications – Disruption of central control over phrenic nerve motoneurons – Malfunction of respiratory control centers • Contraindications – Lower motoneurons injuries – Parenchymal lung diseases – Acute respiratory failure • Full time support often achieved after 3-4 months of progressive bilateral pacing • Permanent tracheostomy usually necessary Management • Risks: – Electrical failure – Not being able to develop deep enough breaths to prevent atelectasis Management • Vaccination – Influenza yearly – Haemophilus influenzae yearly if splenectomy – Streptococcus pneumoniae yearly • If you get a cold – Do more breathing exercises – More assistive cough Chronic complications • Sleep apnea (stop breathing while sleeping) – 15-60% (10 times more in the SCI) – Complications: • Hypertension, cor pulmonale, congestive heart failure, deterioration of mental function, daytime sleepiness, cognitive changes, impotence – Test: overnight oxymetry formal sleep study – Tx: • • • • CPAP or BiPAP Stop alcohol and sleep medicine Lose weight Sleep on side Chronic complications • 55% of vent dependent experience yearly pulmonary problems with average hospital stay of 22 days – 37% mortality in 3 years • Risks of late onset respiratory insufficience – Hx of ventilator usage at onset – VC < 2L – Nocturnal hypercapnia – SaO2 < 95% Follow up • • • • • Level of injury VC X ray Oxygenation Symptoms of sleep apnea Take home messages • Breathing can be seriously impaired after a spinal cord injury • To prevent dangerous complications: – Stop smoking – Do your breathing exercises and treatments – Get vaccinated every year – Take your bronchodilators regularly – When you have a cold, do more breathing exercises and assistive cough Bibliography • Respiratory Dysfunction in Spinal Cord Injury, Sassoon and Baydur, Spinal Cord Medicine, 2003, pp155-168 • Pulmonary management of Spinal Cord Injury, Peterson and Kirshblum, Spinal Cord Medicine, pp 135-152 • Nuts and Bolds of SCI management, Dr Gregory Nemunaitis • Respiratory management following Spinal Cord Injury: a clinical practice guideline for health-care professionals, Consortium for Spinal Cord Medicine, 2005 DAERAH PERTUKARAN O2 Dan CO2: 1. Brokus respiratoris 2. Ducctus 3. Succus dan 4. Alveoli Pertahanan Respiratory system 1 Inhalasi melalui hidung Mempunyai keuntungan 1.Udara disaring. 2.Udara dilembabkan. 3.Udara dihangatkan. 4.Cegah peradangan jalan nafas bag atas. Proses pernafasan. 1. External Respiration a. Inspirasi. b. Expirasi. 2. Internal Respiration. a. Tranportasi (sirkulasi). b. Buffer 1. Exchange O2 1. Air to blood 2. Blood to cells 2. Exchange CO2 1. Cells to blood 2. Blood to air 3. Regulate blood pH 4. Vocalizations 5. Protect alveoli External and cellular respiration Oksigen = 20,93 % Carbon diaksida= 0,03 % Nitrogen = 79,04 % TEKANAN OKSIGEN Di Daerah SEA LEVEL Pulmonary ventilation (breathing) is the proses by which air is moved into and out of the lungs. It has two phases: inspiration and expiration. Inspirasi is an active process in which the diaphragm and the external intercostal muscles increase the dimensions, and thus the volume, of the thoracic cage. This decreases the pressure in the lungs and draws air in. Tekanan alveoli minus 3 s/d 10 mmHg < dari 760 mmHg. • Normal expiration is the passive process. The inspiratory muscle relax and the elastic tissue of the lungs recoils, returning the thoracic cage to its smaller, normal dimensions. This increases the presure in the lungs and forces air out. Forced or labored inspiration and expiration are active proceses, dependent on muscle actions. Aktif inspirasi dibantu otot-otot: Scalani, Sterno cledo mastoideus, pektoralis, membantu angkat sternum dan costae ke depan atas. Tekanan alveoli turun sampai 100-80 mmHg. Aktif ekspirasi dibantu otot-otot : Abdominalis, Latisimus dorsi Inspirasi. Ekspirasi 1. Tranportasinya 2. Pertukaran oksigen dan carbondioksida di cells 3. buffer Perfusi eksterna Eksteranal respirasi: paru Dipengaruhi: respirasi Dalam 1. Cairan surfaktan 2. Tebal membran. 3. Volume darah 4. Hb darah 5. Kecepatan sirkulasi. 6. Vicositas darah. 7. pH darah Tranportasi O2 dan CO2 dalam darah • Kemampuan jantung (COP= HR X Stroke volume). • Tahanan perifer. • Fleksibilitas pembuluh darah. • Lumen. • Vikositas. • Hb. • Saturasi darah dll. Ventilation: The Pumps 1. Inspiration 2. Expiration 3. Diaphragm 1. Low energy pump 2. Concavity – flattens 4. Thorax: ribs & muscles 5. Pleura: double membrane 1. Vacuum seal 2. Fluid-lubrication Pengaruhi internal terhadap kemampuan tubuh suply O2 1. Jalan nafas yang adeguat. 2. Fleksibilitan otot, fasia, kulit sangkar thorax. 3. Perfusi O2 dan CO2 4. Volume, Hb, Ph, Plasma darah 5. Keadan pleurae 6. Pusat kontrol fungsi pernafasan 7. Fungsi bufer. Pengaruh eksternal terhadap kemampuan tubuh suply O2 1. Kadar Oksigen udara. 2. Posisi tubuh 3. Usia jenis kelamin. 2. Pembersih jalan nafas oleh cillia dan fungsi menelan Factors Affecting Ventilation 1. 2. 3. 4. 5. 6. Airway Resistance Diameter Mucous blockage Bronchoconstriction Bronchodilation Alveolar compliance 1. Surfactants 2. Surface tension 7. Alveolar elasticity Base of Plan • Epidemiology • Anatomy-physiology • Acute complications and their management • Chronic complications and their management