RACGP Powerpoint template - Health Networks
advertisement

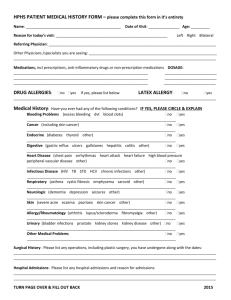
An Integrated Primary Care sector: a view from the front line Dr Frank R Jones – President RACGP Bessie 85 years old 30 years of continuous care 18 inter-related complex co-morbidities: 14 medications ADLs Number of consults Number of referrals, pathology, radiology, specialists, allied health Number of presentations to ED, real and prevented Number of admissions, real and prevented Discharge protocol and timing Communication and teams Continuity of care Topsy-Turvy What? Integrated care is care that crosses boundaries between primary, community, allied health and hospital care and extends beyond health into social care and support too. Providing integrated care is a goal of health systems around the world and is a way of optimising the outcomes for patient, provider and system. According to the WHO, integrated service delivery is ‘the organisation and management of health services so that people get the care they need, when they need it, in ways that are user-friendly, achieve the desired results and provide value for money’. Digital technology General practice - hospital interface Studies demonstrate that improved integration of care result in: • Reduced hospital presentations • Reduced hospital admissions • Reduced hospital stay • High end of town costs Patients first 30% presentations in General Practice are acute health issues 70% presentations are now related to chronic health issues: high end users of our health system -Team based -Coordination and systems critical Digital technology [up to 1/3 of total presentations do not fit into a recognised medical model of illness] Complex co-morbidities Chronic disease costs 70% of the budget and 70% hospital beds are for chronic disease About the RACGP • Sets the standards for education and training, including prevocational, vocational, Fellowship, and continuing professional development • Develops clinical resources and support for an integrated practise • Sets the standards for general practices • Supports and foster primary health care research • Advocacy… The problems 1 Science and technology Sub-specialisation Patient expectation Journalist expertise Hospitals! Complexity [Costs: 46% of FFS Medicare billings spent on 10% of the population] Rx Primum non nocere The problems 2 Duplication Fragmentation Blame games [politics and geography] Our funding model Digital technology Change for integration to happen! The STRUCTURE [systems] The CULTURE [people and professionals] General practitioners – what we dowhere do we fit? • General practice is defined as whole person, patient centred, ongoing coordinated care • The expert generalist : diagnosis: therapeutics: continuity: prevention • Provide undifferentiated care • Treat the person, not just the disease • Our practice is not limited by age, a body part, or a condition WHO view “The first physicians were generalists. Family doctors have always been the backbone of health care Family doctors have always been the bedrock of comprehensive, compassionate, and people centred care” Margaret Chan DG WHO The efficiency of general practice • General practice is the most efficient component of the health system • Continuity of care with a regular GP not only reduces ED visits, it also leads to a fall in elective hospital admissions. • Government costs per person per year for GP (in real $) have remained relatively steady for 15 years [$23.80 per month] • Hospital costs per person (in real $) have increased by approximately 50% over a similar period1 The medical culture Over diagnosis Over treatment Referral pathways Diagnosis creep Poly pharmacy: over prescribing Defensive medicine “ can’t let go” Death defying Watchful waiting The hospital issue Real life happens outside hospitals! Our systems encourages the use of hospital care A death defying health business 8.2% hospital admissions preventable [572,124 patients] ED presentations up by 6% annually 18% admissions iatrogenic 35% referrals to hospital may be inappropriate Why do these patients present? • Complexity of management of chronic disease, particularly for patients with multiple needs • Fragmentation of care – overuse, underuse and misuse of health resources • Over diagnosis – patient harm and health system cost • Medication error and poly-pharmacy • Lack of patient compliance ? What does this mean? • Ultimately, mismanaged care of patient because no one is responsible for coordinating care • Digital technology Collusion of anonymity Collusion truly occurs when "the patient is passed from one specialist to another with nobody taking responsibility for the whole person“ (Editorial: The Doctor, his Patient and the Illness - revisited. Balint Society Journal; 2005. 33http://www.balint.co.uk/journal). We know • Early intervention prevents deterioration and promotes management of chronic disease • The evidence shows that prevention is a cost-effective way of improving population health3 • Centralised coordination of patients with complex needs reduces the risk of an adverse event leading to hospitalisation • General practice is centrally placed to deliver preventive and coordinated health care • General practice has unrivalled capacity and population reach, with: • Over 134 million consultations per year4 • 89% of the Australian population visiting their GP at least once a year4 The business case • There is a strong business case for integration to improve the interface between hospitals and general practice • Investment upstream (i.e. primary health care) will result in savings downstream (i.e. the acute setting) • Keep patients in the community for longer, and if admitted to hospital – get them back into the community sooner • Even a modest reduction of 10% in avoidable chronic disease separations would provide a savings of over $100,000,000 nationally • Digital technology The evidence…. • • • • An increase of 1 general practitioner per 10,000 population is associated with a 6% decrease in mortality: conversely a higher ratio of specialists per population is associated with increased costs and poorer health outcomes The effective delivery of primary health care services results in a significant positive impact on health outcomes at a national level6 Australian and international evidence demonstrated that structured, integrated GP led primary care, reduces: • Hospital presentation (32 – 40% drop) • Hospital admission (16 – 24% drop) • Length of stay (36% drop).7,8,9,10 These are not theoretical figures: real reductions, involving real patients, and real practitioners What does integrated care involve? • Strengthen the interface between GPs and hospitals – we need to communicate better: SILOS OF CARE UNNACEPTABLE • Support GP-led team care arrangements for patients with complex needs, which includes: • Patient handover – genuine GP involvement in admission to hospital and discharge • Improved clinical communication between providers, reducing fragmentation • Service coordination, including patient reminders, follow-up, and clinical advice • Ultimately, we need to support patients with complex needs navigate the health system, improving health outcomes, managing them better, and reducing hospital costs • Digital technology Hearing but not listening What do we need to make it happen? • Expectation is that general practice and primary health care will manage the majority of chronic conditions • GPs can assume this role – but are not currently supported to facilitate integrated care • It is not possible for GPs to absorb the additional work required without appropriate support • Require programs aimed at promoting and supporting the integration of care between the community and hospital • Programs that support integrated care will save hospital funds at local, state and national levels True integration how? 1 Structure -Follow the patient via the medical home concept: patient enrolment -Get the digital technology working -Break down the traditional GP-hospital divide “the head of the bed” -Locally responsive -Totally re-evaluate OPD services -Governance issues -Flexibility -Enhance generalist training -Red tape issues -Where are the Social services? True integration how? 2 Culture -Re evaluate the role of 2o hospitals as community hubs -Clinical leadership: use consultants as consultants -Them and us philosophies -Use GP expertise on admission and discharge -Referral pathways -Digital technology The patient centred medical home: PCMH The PCMH is an approach to providing comprehensive care, whereby each patient has a stable and ongoing relationship with a general practice that provides continuous and comprehensive care from infancy to old age The PCMH facilitates partnerships between individual patients, their personal GP and extended healthcare team, allowing for better targeted and effective coordination and integration of clinical resources to meet patient needs The concept of continuous care supports the critical and core role of the GP as the coordinator of patient care References 1 Australian Government Productivity Commission. Report on Government Services 2013. Canberra: Productivity Commission, 2013. Available at www.pc.gov.au/gsp/rogs/2013 [Accessed 5 May 2014]. 2 Australian Institute of Health & Welfare, Australian Hospital Statistics 2012-13 3 The Department of Health, Annual Medicare Statistics 2013-14 4 Vos T, Carter R, Barendregt J, Mihalopolous C, Veerman L, Magnus A, Cobiac L, Bertram M and Wallace A. Assessing Cost-Effectiveness in Prevention (ACE-Prevention): Final report. September 2010. University of Queensland, Brisbane and Deakin University, Melbourne. 5 Starfield B, Leiyu S, Grover A, Macinko J. The Effects of Specialist Supply on Populations' Health: Assessing the Evidence. Health Affairs 2005: doi: 10.1377/hlthaff.w5.97 6 Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health Services Research. 2003;38(3):831– 865 7 Grumbach K and Grundy P. Outcomes of implementing patient centred medical home interventions: A review of the evidence from prospective studies in the United States. Patient-Centred Primary Care Collaborative. . November 16 2010. Available from: http://www/pcpcc.net 8 GilfillanR, Tomcavage J, Rosenthal M, Davis D, Graham J, and Roy, J. E.Value and the Medical Home: Effects of Transformed Primary Care. American Journal of Managed Care 2010;16(8):607-614 9 Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA Jr. Community care of North Carolina: improving care through community health networks. Ann Fam Med 2008;6: 361-367 10 Geisinger Health System. Presentation at White House Roundtable on Advanced Models of Primary Care:August 10, 2009; Washington DC, United States [food for thought] Minimise errors in diagnosis Discontinue low or no value practices Defer unproven interventions Select care options as compared to cost Target clinical interventions to those who will derive greatest benefit End of life considerations Actively involve our patients Minimise day to day operational waste Convert healthcare institutions into rapidly learning institutions Integrate patient care across all settings