Clinical Case
advertisement

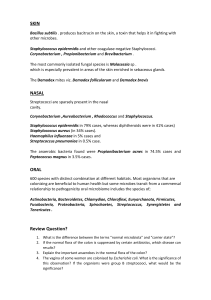
Fascinoma Rounds Coagulase negative staphylococcus in the urine October 26th, 2005 Sharmistha Mishra, Vanessa Allen, And with great thanks to Subash Mohan Case 2: Coagulase negative staphylococcus in the urine • What is the clinical significance of finding CN staph in urine? Pathogens • Coagulase negative staphylococcus • 35 spp. ~ 15 potential human pathogens – Staphylococcus saprophyticus • Common cause of UTI in young women • Treated as outpatients – Staphylococcus epidermidis • Rare growth in urine • Generally hospital acquired – Distiguished by novobiocin in the lab Urinary Tract Infections Caused by Coagulase-Negative Staphylococci: Characteristics of Infections Organism S. epidermidis S. saprophyticus Age and sex of affected patients Men and women equal Usually older than 50 years Women 95% 16 to 35 years old Population at risk Hospitalized patients with urinary tract complications Healthy outpatients Incidence Uncommon: 3.5% or less of all urinary tract infections in hospitalized patients Common: 20% or more of all urinary tract infections in this age group Presentation 90% asymptomatic 90% symptomatic Therapy Often resistant to multiple antibiotics Responds readily to urinary tract antimicrobials; except nalidixic acid Outcome Bacteriuria often persists after therapy Relapse rare; occasional reinfection Septicemia Associated with Staph epidermidis UTI - Case #1 • 77M with DM and HTN • Right hip sub-trochanteric fracture and ORIF • Subsequent urinary incontinence -> indwelling Foley catheter • Two weeks later he had high grade fever, confusion, and lethargy (foley had already been removed), temperature was 39.4° C , blood pressure 70/0 mm Hg, HR 126/min • IV NS, ampicillin, and aztreonam and dopamine • Two blood cultures = S epidermidis. • Urine specimen = S epidermidis (> 106 colony-forming units/mL) • Same susceptibility pattern (vancomycin, tetracycline, and trimethoprim-sulfamethoxazole). Cadorna, EA. et al, SMJ, 0038-4348, Aug 1, 1995, vol. 88, issue 8 Septicemia Associated with Staph epidermidis UTI - Case #2 • 64M in MVA , traumatic rupture of left hemidiaphragm • Exploratory laparotomy with repair of diaphragm, left chest tube thoracostomy, and feeding jejunostomy placement • 3 weeks later, pulmonary embolism -> placement of an IVC filter • @ 8 weeks, the jejunostomy tube, Foley catheter, intravenous lines, and tracheostomy tube were removed. • Three weeks later, his temperature rose to 39.4°C; blood pressure was 64/46 mm Hg, and the heart rate was 124/min. • Two blood cultures = S epidermidis. • Urine culture S epidermidis (>106 CFU/mL) with the same antimicrobial susceptibility pattern (vancomycin, tetracycline, trimethoprimsulfamethoxazole). Possible Explanations • Hematogenous spread of staphylococcus epidermidis • Staphylococcus lugdunensis – vs other CN staph species S. lugdunensis • CN staph • Transient skin flora, inguinal area • Identified by PYR hydrolysis and ornithine decarboxylate activity • More virulent than other CN staph – lipase, esterase, glycocalyx and fibrinogen affinity factor • Focus of infection (229) – – – – – – – – skin and soft tissue infections (7, 65) respiratory infections (13) endocarditis Bacteremia (15) brain abscess vascular prosthesis infection (11) osteomyelitis. Abscesses 14 Staphylococcus lugdunensis UTIs • Generally reported as mixed flora in urine • Rarely a contaminant • Case #1 – 6F admitted with a 16 h history of fever to 39.7°C, flank pain, nausea and vomiting. – WBC 18.14 – A catheter specimen urinalysis showed proteinuria (1+), traces of blood and absence of nitrites – microscopic analysis showed 10–20 leukocytes with a small number of bacteria. – Urine culture showed growth of >100,000 colonies/ml of S. lugdunensis in a pure culture. Casanova-Roman M. et al. Scandinavian Journal of Infectious Diseases. 36(2):149-50, 2004. Clinical correlate of staph lugdunensis in urine culture • Mayo Clinic • 500 isolates of coagulase-negative staphylococci from 4,652 consecutive urine specimens • 31/500 (6%) staph lugdunensis • 29/31 of mixed flora • 70% not treated Haile Dt et al. Journal of Clinical Microbiology. 40(2):654-6, 2002 Feb.