DNA and RNA: molecules of heredity
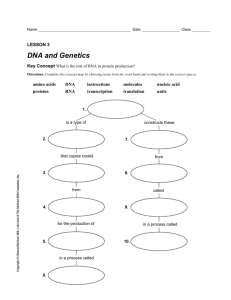
advertisement

NAGE – Nucleic Acids and Gene Expression L1 – Nucleic acids and chromosomes DNA and RNA: molecules of heredity DNA carries genetic information. The genes of all cells are made of DNA. Chromosomes (DNA + proteins) segregate as cells divide DNA and RNA each contain 4 different types of nucleotides that are arranged in different sequences. 3D structure of DNA: double helix made up of two chains wrapping around each other. RNA can assume a variety of shapes. A nucleotide consists of a nitrogenous base, a sugar and one or more phosphate groups. E.g. A nucleotide: deoxyadenosine 5’triphosphate dATP. Sugars DNA: deoxyribose, lacks an oxygen atom that is present in ribose, the parent compound. RNA: Ribose. Primes (’) are used in numbering the carbon atoms in the ribose: 1’ to 5’. The 1’ C is linked to the base; the 5’ C is linked to the phosphate. PURINES: Adenine and guanaine PYRMIDINES: Cytosine, thymine and uracil. Nucleosides Base Base + (deoxy)ribose = nucleoside adenine (deoxy)adenosine guanine cytosine uracil thymine Nucleoside (deoxy)guanosine (deoxy)cytidine (deoxy)uridine (deoxy)thymidine Nucleotides Base + ribose + phosphate = nucleotide E.g. Adenosine monophosphate A long chain of deoxyribonucleotide units linked by phosphodiester links. The 3’-OH of sugar of one nucleotide is linked to phosphate group, which in turn is joined to 5’-OH of adjacent sugar. On each deoxyribose there is a base. The chain has two ends, the 5’ end and the 3’ end. It is not symmetrical. The PRIMARY STRUCTURE of a nucleic acid chain is the sugar-phosphate backbone with the bases, defined by the linear sequence of the bases. The bases carry genetic information, the sugar and phosphates perform a structural role. By convention, the nucleotide sequence is specified from the 5’ to the 3’ end. The first nucleotide in a sequence has a free 5’ phosphate, and the last one a free 3’ OH. SECONDARY STRUCTURE, right-handed double helix shown by x-ray diffraction patterns. Antiparallel chains running in opposite directions. The deoxyribose and phosphate groups run along the outside with the negative charges outside (allows electrophoresis). The bases point inwards and the flat planes are perpendicular to the helix. The two chains are held together by hydrogen bonds between the bases. A and T, 2 hydrogen bonds. Less stable. C and G, 3 hydrogen bonds. More stable. Approx. 10 base pairs per helical turn. Hydrogen bonds between the bases stabilise the structure. Pairing of specific bases (Watson - Crick base pairs). Melting and Reannealing High temp or low salt conc causes 2 strands to melt and dissociate. Lowering temp or increasing salt conc causes 2 strands to reanneal into a double helix. HYBRIDISATION: in a mix of DNA with different sequences, complementary strands will find each other. E.coli Genome The entire DNA coding for an organism constitutes its genome. E.coli has 4.6 x 106 base pairs in a single circular double-stranded molecule. The length of E.coli DNA is 1.4 mm. Human Genome ~ 3 x 109 base pairs of DNA divided into chromosomes that each contain a single, linear doublehelical DNA molecule of ~ 200 x 106 base pairs. Chromosomes are visible only just before cells divide but not in non-dividing cells Mitotic chromosomes: highly condensed form of chromosomes Interphase chromosomes: extended form. A KARYOTYPE is an organised profile of someone’s chromosomes. A diploid human cell has 46 chromosomes 22 pairs of ‘normal’ chromosomes (autosomes) and 2 sex chromosomes (X and Y) Sex chromosomes: XX for female; XY for male. 2 homologues of each chromosome. Abnormal karyotypes: Abnormalities in breast tumour, 48 chromosomes instead of 46, multiple translocations, eg two pieces of chromosome 8 (green) plus piece of chromosome 17 (purple). DNA in interphase chromosomes is less compact than that in mitotic chromosomes. Electron micrograph showing chromosomal DNA spilling out of lysed interphase nucleus. Also, a condensed mitotic chromosome, to scale… Packaging of eukaryotic DNA Eukaryotic DNA is tightly packaged, forming a complex with proteins. This complex is called chromatin. During interphase, when cells are not dividing, chromatin is more extended. Further condensation during mitosis produces chromosomes. The lowest level of packaging is the nucleosome, which consists of DNA wrapped around histone proteins. Core DNA wrapped around core histones. ‘Beads on a string’ Structure of nucleosome Histones: positively charged; interact with negatively charged sugar-phosphate backbone of DNA About 150 base pairs of DNA wrapped around the histones (core DNA). The nucleosome causes an approximately 7-fold condensation of DNA. The chain of nucleosomes is further packed to generate a more compact structure In the interphase nucleus the DNA is further condensed about 100-1000 fold. DNA double helix Beads on a string form of chromatin. Nucleosomes joined by linker DNA. 30 nm chromatin fibre of packed nucleosomes Section of chromosome in extended scaffold (interphase chromosome) Condensed section of chromosome Entire mitotic chromosome. Semi-conservative replication - each daughter cell inherits one old and one new strand. Green = old strands. Red = new strands. Opening of DNA helix The DNA helix is very stable and has to be unwound before replication. This is done by a DNA helicase. Enzyme that uses ATP as source of energy to break hydrogen bonds between base pairs New DNA is synthesized by enzymes called DNA polymerases. DNA polymerases add nucleotides to the 3’ end of a growing chain. DNA polymerases require: a template strand an oligonucleotide primer. Oligonucleotide = a short nucleic polymer with typically 50 or fewer bases. a supply of deoxynucleotide triphosphates (dNTPs) (Free nucleotides) DNA polymerases add dNTPs to the 3’ end of a DNA molecule. DNA (and RNA) synthesis occurs in 5’ to 3’ direction. Energy is released by hydrolysis of the triphosphate. This drives the reaction. A free 3’ hydroxyl group is required. Image p.27 Nucleoside analogs used as drugs DIDEOXYCYTOSINE for HIV drug Zalcitabine. AZIDOTHYMIDINE for HIV drug Zidovudine. CYTOSINE ARABINOSE as chemotherapy drug. Lecture 2/3 – DNA replication, the cell cycle and mitosis. THE REPLICATION FORK Replication begins at discrete points on the DNA molecule called origin of replication. The two daughter molecules are identical, each containing an old and a new strand The site of DNA synthesis is called a replication fork: the fork moves along during the process. The templates for the two new daughter strands have opposite orientations: 3’ to 5’ and 5’ to 3’. The leading strand is synthesised continuously, whereas the lagging strand is synthesised in short pieces termed Okazaki fragments. RNA primes the synthesis of new DNA. A specialised RNA polymerase called DNA primase synthesises a short RNA fragment (~ 5 nucleotides). The RNA primer is only transient and removed at a later stage of replication. Joining of Okazaki fragments A special ribonuclease removes RNA primer using a 5’ to 3’ exonuclease activity. A repair DNA polymerase then replaces RNA with DNA. DNA ligase joins the two fragments together using ATP. This makes the DNA strand continuous. The high fidelity of DNA replication requires a proof-reading mechanism to ensure no mistakes are made. Before a new nucleotide is added, the previous nucleotide is checked for correct base-pairing. Any incorrect bases are removed by 3’ to 5’ exonuclease activity of DNA polymerase. A new, correct nucleotide is then added. Replication of the E.coli chromosome Replication starts at a unique origin, OriC. Two replication forks proceed simultaneously in opposite directions. The two forks meet at the other side of the circular chromosome. Bidirectional replication. Replication in eukaryotic chromosomes Eukaryotic chromosomes are linear and very long. Multiple replication origins are distributed at intervals of about 100 kilobase pairs. Each replication origin gives bi-directional replication forks. Replication is finished when all the forks have met. CELL CYCLE M phase: Mitosis; cell division; 1hr G1 phase: Gap phase 1 (prior to DNA syntesis); 10 hrs S phase: period of DNA synthesis (replication); 9hrs G2 phase: Gap phase 2 (between DNA synthesis and mitosis); 4 hrs G0: cells which have stopped dividing I: Interphase. Includes G1, G0, S and G2 G1: DNA of each chromosome present as a single linear double helix of DNA S phase: the DNA is replicated G2: each chromosome has two identical sister chromatids Mitosis: the two chromatids separate to the daughter cells L4 – Gene organisation and transcription – II mRNA processing When a gene is used we say it is “expressed” 10,000 - 30,000 different genes are expressed in human cells / tissues Some genes are expressed in all cells. These include “Housekeeping Genes” - needed for normal cell function and viability ~ 25% of genes expressed in the cell are required for cell specific function. The initial product of gene expression is always Ribo Nucleic Acid (RNA) RNA is a single stranded nucleic acid species The pentose sugar in RNA is Ribose Thymine is not a base used in RNA. It is replaced by Uracil. Cells contain three major species of RNA: transfer RNA (tRNA), ribosomal RNA (rRNA) and messenger RNA (mRNA) Gene expression occurs in the cell nucleus. RNA is exported to the cell cytoplasm, to be used in “Protein Translation”. Transcription: Making an RNA copy of a DNA strand • Gene transcription is carried out by enzymes called “RNA Polymerases” • Gene transcription also involves special gene regulatory proteins called “Transcription Factors” • The “start” of a gene contains DNA sequences that are important in bringing about transcription SENSE STRAND (CODING) = strand of DNA that has the same sequence as the mRNA. ANTISENSE STRAND (TEMPLATE) = complementary to the sense/coding strand. Stand on which the RNA is built up. Eukaryotic cells contain three types of RNA polymerases: • RNA Polymerase I -Transcribes rRNA genes • RNA Polymerase III- Transcribes tRNA and 5S RNA genes • RNA Polymerase II - Transcribes genes encoding proteins into mRNA The elongation reaction of RNA synthesis requires a separate and distinct initiation step to build a transcription complex. The DNA sequences at which the initiation complex assembles is called a gene promoter . The level of transcription from a given gene is regulated by the activity of DNA binding proteins, or Transcription Factors. • Can activate gene expression- “Transcriptional Activators” • Can suppress gene expression- “Transcriptional Repressor” Act collectively to bring about cell specific / developmental / inducible gene expression. TF II D contains TATA Binding Protein(TBP) and TBP Accessory Factors (TAF’s). On binding to DNA TF II D:• Partially unwinds the DNA helix, widening the minor grove to allow extensive contact with bases within the DNA • This unwinding is asymmetric with respect to the TBP-TATA complex,thereby assuring transcription is unidirectional Next, TFIIA and TFIIB bind. TFIIB is particularly important, as it is able to bind to TFIID and RNA Polymerase II. RNA polymerase binds to TF IIB with TF IIF bound. The final steps involve the binding of TFIIE,TF IIH and TFIIJ. TFII H promotes further unwinding of the DNA helix to facilitate RNA synthesis by RNA Polymerase II. The Basal Transcription Complex allows RNA polymerase II to be phosphorylated and then engage in transcription. In the absence of binding of other Transcription Factors this produces a Basal (low) level of transcription. Transcription factors “bend DNA” on binding. They can interact with each other and the Basal Transcription Complex to modulate transcription. Transcription factors also facilitate transcription by helping to remodel “chromatin”. They do this by recruiting proteins with enzymatic activities that modify histones. Deacetylated histones “CLOSED” Acetylated histones “OPEN” Histone tails extend from nucleosome => subject to post-translational modification HYPERACETYLATION CORRELATES WITH GENE EXPRESSION HYPOACETYLATION CORRELATES WITH GENE REPRESSION Cell lineage is a major determinant of Transcription Factor expression. Cell lineage = related to the cells derivation from undifferentiated tissue of the embryo. Transcription Factor expression / activity are altered by signals external to the cell, e.g.: hormones, growth factors, mechanical stress, heat, cell contact, light, touch and voltage. Transcription factors and disease Mutated Transcription Factors have been implicated in several human hereditary disorders Abnormal Transcription Factor expression is found in several human cancers. Mutations affecting the regulation of specific genes have been described in certain human disease. • Describe the addition of a “cap” and “poly A tail” to pre-messenger (hn-) RNA. Primary RNA transcripts need to be processed to form mature mRNA. Post transcriptional modification of mRNA The promoter lies at the start (5’ end) of the gene The sequence information contained in the final mRNA is encoded “discontinuously” in the DNA of the gene Segments of the gene which contain sequences that form part of the final RNA are called “exons” “Introns” are sequences in the gene which are transcribed but are edited out of the final mRNA. A “CAP” structure is added to the 5’ end of the mRNA. The CAP is formed by hydrolysis of the terminal triphosphate of the mRNA to a diphosphate. This then reacts with the phosphate of GTP to form a 5’-5’ phosphate linkage. The CAP is further modified by methylation at the N7 position in the purine ring to form a 7methylguanylate cap. The cap acts to protect mRNA at the 5’ end and also greatly enhances the translation of mRNA. Viruses such as polio are able to interfere with the recognition of the cap during translation. Polyadenylation is the addition of a poly A tail to the pre-mRNA The poly A tail is added one base at a time. The poly A tail is added 11-30 bases downstream of the sequence AAUAAA, which is found in all mRNAs • Define what is meant by a “splice donor site” Site at the 5’ end of an intron. Between AG of exon and GU of intron. • Define what is meant by a “splice acceptor” site. Site at 3’ end of an intron. Describe the “lariat” intermediate in mRNA splicing Exposed adjacent exons are ligated together Define the function of the “Spliceosome” The binding of U2, U4, U5 and U6 completes the formation of the splicing complex or “spliceosome”. This causes the cleavage in the splice donor sequence. • With examples, describe how mutations in splice sites feature in human disease. POLIOMYLITIS (POLIO) Polio virus can invade the nervous system, and cause total paralysis in a matter of hours The virus enters the body through the mouth and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck and pain in the limbs Polio virus is able to interfere with the recognition of the cap during translation THALASSAEMIA A genetic, haematological, disease in which there is an imbalance in the relative amounts of alphachains and beta-chains making up Haemoglobin. In b-Thalassemia there is a relative deficiency of beta-chains Several types of b-Thalassemia feature splice site mutations in the beta-globin gene L5 - Small RNAs in the Regulation of Biological Processes • Have a good understanding of the complexity of genome and gene regulation in eukaryotic organisms There is a constant amount of genetic material in cells from the same species. However, the complexity of an organism is not necessarily related to its genome size (C-value). Transcription of a genome Only 5% of human and mouse genomes are conserved – this includes nearly all protein coding genes and a substantial number of genes for non-coding RNAs The remaining 95% of the human and mouse genome has historically been regarded as ‘junk’. Junk DNA is transcriptionally active The majority of mutations that cause genetic disease don’t map to junk DNA, they map to genes that encode proteins • Understand the concept of small non-coding RNAs in gene regulation and the experimental support for this. Non-coding RNAs Any RNA molecule that is not translated into protein (ie Does not include mRNA) Includes housekeeping ncRNAs (ie ribosomal RNA, tRNA and spliceosome snRNAs) Also includes regulatory ncRNAs • microRNA • siRNA / RNAi – viral defence, experimental tool • piRNA – fascinating, clearly important for germ cell production • Endo siRNAs small endogenous RNA • long ncRNA:- Xist – important for X chromosome inactivation. H19 – involved in imprinting of the IGF-1 gene plus many more anti-sense RNAs with potential for imprinting and gene regulation - control the translation of perhaps most genes Gene regulation by non-coding RNAs C. elegans (nematode worm) is one of the simplest organisms with a nervous system. In the hermaphrodite, this comprises 302 neurons whose pattern of connectivity, or "connectome", has been completely mapped and shown to be a small-world network. The developmental fate of every single somatic cell (959 in the adult hermaphrodite; 1031 in the adult male) has been mapped. • Have a biochemical understanding of gene regulation through dsRNAs (double stranded)– RNA interference Antisense RNA: a single-stranded RNA that is complementary to mRNA strand transcribed within a cell. Antisense RNA may be introduced into a cell to inhibit translation of a complementary mRNA by base pairing to it and physically obstructing the translation machinery. Transgenic tomatoes have been constructed that carry in their genome an artificial gene (DNA) that is transcribed into an antisense RNA complementary to the mRNA for an enzyme involved in ethylene production. These tomatoes make only 10% of the normal amount of the enzyme. Ethylene synthesized by the tomato causes them to ripen and spoil before they reach the customer. dsRNA is the silencing trigger in Caenorhabditis elegans RNA silencing: the expression of one or more genes is reduced or entirely suppressed by the introduction of an antisense RNA molecule. RNA silencing is used by plants as a defence mechanism against virus infection. Works through the generation of small single stranded RNAs that anneal to viral RNA and cause these to degrade. • Describe the biochemical processes underlying RNA interference siRNA = small interfering RNA Dicer is an essential gene Lethality in early embryonic stages, embryonic stem cells unable to differentiate, depletion of multipotent stem cells. Limb morphogenesis defects, lung development defects, incomplete embryonic myogenesis, epidermal, hyperproliferation, reduced development of ventricular myocardium RNAi - a targeted gene expression knockdown technique Through the use of synthetic dsRNAs, the RNA interference pathway has been used as a route to obtain gene targeted knockdowns in eukaryotic cells With vertebrate systems, particular attention has been paid as to how to deliver such dsRNAs into cells without invoking a detrimental cytokine response This had led to the use of siRNA mimics and shRNAs (small hairpin). • Describe what micro RNAs (miRNAs ) are and how they act in gene regulation Micro RNAs are genomically encoded small hairpin RNAs. First miRNA discovered was lin-4 in C.elegans by Lee et al., 1993 and Wightman et al., 1993 Let-7 was later discovered in 2000 – has a human homologue Typically 18-26 nucleotides in length Evolutionarily conserved >700 miRNAs identified in humans (miRBase) Predicted to regulate the expression of >30% of all protein-coding genes miRNA binding sites miRNAs inhibit target mRNAs through base pairing with incomplete complementarity The “Seed” region is the most important region of the miRNA for targeting. Lies between nucleotide positions 2 to 8 from the 5’ end, and is often flanked by adenosines. Mismatches, predominantly in the centre forms a bulge, often followed by a less stringent degree of complementarity in the 3’ region The vast majority of known miRNA target sites lie within 3’UTRs. The position and number of binding sites can influence repression efficiency. • Cite at least one example of miRNA involvement in human disease (taken from the lecture, or from directed reading) CHRONIC LYMPHOID LEUKAEMIA – caused by alterations in ncRNA and miRNA. miRNA 15a and 16-1 L6 – Protein translation and post translational modification • Outline the mechanisms by which ribosomes can translate a mRNA sequence into a protein sequence mRNA is transported out of the nucleus and translated in the 5’->3’ direction into protein (N->C direction) in the cytoplasm and on the rough endoplasmic reticulum The machinery for translating mRNA is the ribosome, a large 2 subunit complex of proteins and ribosomal RNA (rRNA) Translation: a) Initiation Step 1: dissociation of ribosomal subunits 40S and 60S Step 2: assembly of preinitiation complex. Consists of elF-2, GTP, 40S subunit and Met-tRNA. Only initator Met-tRNA can bind to 40S subunit on its own. Step 3: preinitiation complex binds to mRNA. Initiator Met binding sets the translation frame. elF4E and G recognised by 40S/Met-tRNA/elF2 Step 4: binding of 60S subunit. GTP GDP + Pi (ensures correct base pairing) Translation b) Elongation Step 1: binding of new tRNA carrying second amino acid to A (amino acyl site). New tRNA binds to adjacent A site in frame to Met-tRNA. Step 2: catalysis of peptide bond between 2 amino acids by peptidyl transferase on 60S subunit. Step 3: translocation of peptidyl transferase to P site. Elongation factors are proteins that promote the movement of the 60S subunit along the mRNA using GTP. EFs use the energy of GTP to enhance the efficiency and accuracy of translation by providing “pauses” (e.g. GTP hydrolysis) that allow incorrect base pairs to dissociate First tRNA dissociates and steps repeat. Translation c) Termination Step 1: recognition of stop codon. Release factors bind to empty A site, not tRNAs. Step 2: release of peptide chain Peptidyl transferase catalyses transfer of the completed protein chain to water and releases it from the ribosome. Step 3: dissociation of release factors and ribosomes • Describe the role of aminoacyl tRNAs in ensuring the fidelity of the genetic code Aminoacyl tRNA synthetases: one for each aa. Important role in fidelity of translation (selectivity for correct aa; hydrolysis of incorrect aa-tRNA) An enzyme that catalyzes the esterification of a specific amino acid or its precursor to one of all its compatible cognate tRNAs to form an aminoacyl-tRNA. • State how a ribosome recognises the start and end of a sequence to be translated Reading mRNA: • Ribosome scans from 5’ end of mRNA (cap) • Translation starts at first AUG, continues in frame, i.e. with immediately succeeding triplet codon (CAU) and so on….. • Translation stops at first in frame termination codon Ribosomes do not work singly on a mRNA but in multiple copies on the mRNA – a polyribosome – like a string of beads • Explain why some antibiotics inhibit protein synthesis in prokaryotes but not eukaryotes Antibiotics exploit differences between prokaryotic and eukaryotic ribosomes and translation factors Antibiotics selectively inhibit prokaryotes • Identify the features of a newly-synthesised protein that are required for it to enter the secretory pathway Most cellular compartments are bounded by a membrane so the cell needs a mechanism to transfer proteins across membranes First 20-24 amino acids = “signal sequence” Step 4: cleavage of signal sequence by signal peptidase (co-translational) and folding. Transmembrane proteins have an extra hydrophobic sequence holding them in the membrane. • Give examples of the ways in which newly-synthesised proteins can be post-translationally modified e.g. insulin Insulin biosynthesis in pancreatic β cells Insulin undergoes extensive post-translational modification along the production pathway: disulphide bond formation in the ER and proteolytic cleavage (cleaved to form the mature version of the protein) in the secretory vesicle to produce active insulin. Forms of post-translational modification: • Disulphide bond formation (e.g. insulin) • Proteolytic cleavage (e.g. insulin -> A and B chains) • Addition of carbohydrate (Glycosylation) • Addition of phosphate (Phosphorylation) • Addition of lipid groups (Prenylation, Acylation) • Hydroxylation (e.g. Collagen; Leitinger lecture) L7 – Mrs Jones’ first consultation Congenital Abnormalities Apparent at birth in 1 in 50 of all new-born infants 20-25% of all deaths during perinatal period and childhood up to the age of 10 years Genetic factors contribute to about 40% of all congenital abnormalities Malformation – primary structural defect e.g. atrial septal defects, cleft lip. Usually involves a single organ showing multifactorial inheritance. Disruption – secondary abnormal structure of an organ or tissue e.g. amniotic band causing digital amputation. (Caused by ischaemia, infection, trauma. Not genetic, but genetic factors can predispose). Deformation –abnormal mechanical force distorting a structure e.g. club foot, hip dislocation. (Occurs late in pregnancy and has a good prognosis as the organ is normal in structure). Syndrome –consistent pattern of abnormalities with a specific underlying cause, e.g. Down syndrome Sequence –multiple abnormalities initiated by primary factor e.g reduced amniotic fluid leads to Potter sequence. Oligohydramnios – reduced volume of amniotic fluid due to failure to produce urine. Usually due to bilateral renal agenesis (failure of foetal kidneys to develop Dysplasia –abnormal organisation of cells into tissue e.g thanatophoric dysplasia. Single gene defect. Short flat bones, small thorax, large head Association –non-random occurrence of abnormalities not explained by syndrome. Cause is typically unknown. e.g. VATER association. Vertebral, Anal, Tracheo-Esophageal, Renal Chromosomes FISH – fluorescent in-situ hydbridisation. Chromosome Banding Nomenclature Chromosome Banding Nomenclature Bands are labelled according to the chromosome number, short (p) or long (q) arm and numbered out from the centromere. Chromosomal Abnormalities: Trisomy 21 – Down Syndrome, Monosomy X – Turner Syndrome, Polysomy X, Sex Determination, Microdeletion Syndromes Numerical – aneuploidy, loss or gain. • Monosomy - loss of a single chromosome is almost always lethal Monosomy X – Turners’ Syndrome Generalised oedema and swelling in neck region can be detected in 2nd trimester. Low posterior hairline. Normal intelligence 80% caused due to loss of X or Y chromosome in paternal meiosis. Also ring chromosome, single arm deletion and mosaicism (the presence of two or more populations of cells with different genotypes in one individual). Ring chromosome: breaks occur at the ends of a chromosome and the sticky ends attach to each other. Fragments are lost. Often unstable at mitosis so mosaicism is common. Polysomy X in females: • 10-20 point decrease in IQ • No physical abnormalities • 1:1000 have 47,XXX karyotype • 95% have extra maternal X arising in meiosis I • Normal fertility • 48,XXXX and 49,XXXXX karyotypes show mental retardation Polysomy X in males: • Klinefelter’s syndrome (47,XXY) • 1 in 1000 male live births • X chromosome from either Male or Female • 48,XXXY and 49,XXXXY are rare It’s possible to be chromosomally one sex, but phenotypically the other. Chromosomal microdeletion disorders Di George Syndrome: • Congenital Heart Disease • Palatal abnormalities • Thymic/Parathyroid Hypoplasia • Characteristic Facies • Learning Difficulties • Commonest microdeletion disorder • Approx 1/4000 live births • Trisomy - gain of one chromosome can be tolerated Trisomy 21 – Down Syndrome. Approx 1 in 700 incidence. Strong correlation between incidence and maternal age. Clinical features: • Newborn period - severe hypotonia (lack of muscle tone), sleepy, excess nuchal skin • Craniofacial – macroglossia (enlarged tongue), small ears, epicanthic folds, upward sloping palpebral fissures, Brushfield spots (spots on iris) • Limbs – single palmar crease, wide gap between first and second toes • Cardiac - A and V septal defects • Other - short stature, duodenal atresia (duodenum not properly developed). 95% are trisomy: 90% of which is extra chromosome from mother and 5% from meiotic nondisjunction. 4% caused by translocation, and 1% from mosaicism from mitotic nondisjunction. • Tetrasomy - gain of two chromosomes can be tolerated Loss of a chromosome gives a 50% reduction in fully expressed gene products, gain of a chromosome gives a 33% increase. Partial Aneuploidy – translocations, can be balanced or unbalanced. Structural – translocations, deletions, insertions, inversions, rings. Mosaicism – different cell lines L8 – Mrs Jones (2) – Risk of transmission of transmission of genetic disease GENETIC DISEASE Monogenic: Clear inheritance, no environmental impact, rare. (Huntingtons, CF, Haemophilia) Complex disorders: No clear inheritance, environmental impact, more common. (Type II diabetes, obesity, Parkinson’s) Mendelian Inheritance: process whereby individuals inherit and transmit to their offspring, one of the two alleles present in homologous chromosomes. Alleles: Alternate forms of gene or DNA sequence at the same chromosome location (locus) Homologous chromosomes are a matching (but non-identical) pair, one inherited from each parent. Different alleles may be described as mutations (any heritable change in the DNA sequence) or polymorphisms (called mutations if they cause monogenic disease, may contribute to complex disease) Types of Mutation Point Missense and nonsense. Change in (usually) one DNA base pair that results in the substitution of one amino acid for another in the protein encoded by a gene. Missense Nonsense Frameshift Insertion and deletion Mendelian Inheritance patterns Autosomal Dominant At least one parent affected. Transmitted from M or F, 50% chance of vertical inheritance. E.g. Huntington’s. The HTT gene on encodes a protein called huntingtin patients inherit one copy of a mutated form of the huntingtin gene. Altered gene encodes a toxic form of the protein that forms ‘clumps’ Cell death in basal ganglia of brain, leading to symptoms. Caused by an unstable triplet repeat (CAG): the number of repeats may expand with each generation. Autosomal Recessive No affected parent. Transmitted by M or F, 25% chance of inheritance and 50% of becoming a carrier. E.g. Cystic Fibrosis The CFTR gene encodes a protein called the CF transmembrane conductance regulator. Patients inherit two copies of a mutated form of the CFTR gene, so protein folds abnormally. Absence of functional CFTR protein affects chloride ion channel function in epithelial cells. Disruption of salt /water regulation causes thick mucus and leads to symptoms. Congenital absence of the vas deferens (CAVD) is also usually caused by a mutation in the CFTR gene. X-linked domnant – Rare – Rett Syndrome Penetrance – frequency with which symptoms are present in an individual who inherits a diseasecausing mutation. Variable expressivity – degree of severity in an individual who inherits a disease-causing mutation Phenocopy - having the same disease but with a different underlying cause Epistasis – interaction between disease gene mutations and other modifier genes can affect phenotype Dominant vs recessive: molecular mechanisms DOMINANT: normally caused by gene mutations that produce a toxic protein. need to neutralise the effects of the toxic protein or ‘switch off’ the mutant gene, “unmasking” the normal gene RECESSIVE: caused by the absence of a working protein. need to restore the activity of the missing protein, by replacing the gene or protein product, or even affected tissues CODOMINANT: the effects of both normal and faulty gene are seen in the person with both. X-linked Recessive No affected parent, M affected, transmitted by a carrier F. 50% sons affected, 50% daughters carriers. E.g. Haemophilia A blood-clotting disorder. Affected people bruise easily and bleed for longer. Two main types, A and B. The F8 gene encodes a protein called coagulation factor VIII. Boys with Haemophilia A inherit one copy of a mutated form of the F8 gene. Lack of functioning Factor VIII causes symptoms. Haemophilia B is caused by mutations in the F9 gene, also on the X chromosome. F9 gene codes for coagulation factor IX. Symptoms are identical to those of Haemophilia A. Haemophilia B is much rarer than Haemophilia A • Same disease, different genes – eg. Bardet-Biedl Syndrome caused by defects in 15 different genes • Same disease, different genes, different inheritance patterns – eg. different forms of epidermolysis bullosa (skin blistering disease) can be autosomal dominant or autosomal recessive Mitochondrial L9 – More stories from the genetic clinic IMPRINTING DISORDERS Parental origins of chromosomes are important 46,XX where genome is only from one parent Maternal – Ovarian Teratoma (an encapsulated tumour with tissue or organ components resembling normal derivatives of all three germ layers) Paternal – Hydatidiform Mole (abnormal form of pregnancy wherein a non-viable fertilized egg implants in the uterus and converts a normal pregnancy into an abnormal one) The genome carries an imprint of its parental origin Imprinting is a reversible epigenetic effect DNA Methylation is the mechanism Prader-Willi/Angelman Syndromes Same chromosomal region involved on Chr15. Result from loss of function of one of the two parental chromosomes Paternal = Prader-Willi Maternal = Angelman Prader-Willi: Symptoms include; Muscle hypotonia, Hyperphagia, Obesity/Diabetes, Mental retardation, Short stature, Small hands and feet, Delayed/Incomplete Puberty, Infertility. Lack of a functional paternal copy of the PWS critical region on 15q11-q13 ~70% Deletion of the critical region on the paternal chromosome ~25% Inheritance of two maternal copies by uniparental isodisomy ~5% due to translocations, point mutations Uniparental Isodisomy • Non-Disjunction in Meiosis II • Fertilisation of normal monosomic gamete • Loss of chromosome from parent contributing the single chromosome Angleman Syndrome: Severe developmental delay, Poor or absent speech, Gait ataxia (lack of voluntary coordination of muscle movements.), “Happy demeanour”, Microcephaly, Seizures. Loss of function of the maternal chromosome from chromosome 15. MITOCHONDRIAL DISORDERS Transmission is exclusively through females Affects both males and females Disease can be very variable because of heteroplasmy presence of a mixture of more than one type of an organellar genome (mitochondrial DNA (mtDNA) or plastid DNA) within a cell or individual. Mitochondrial Genome ~16kb 37 genes; 13 for respiratory chain complexes, 22 for tRNA, 2 for rRNA and 2-10 copies per mitochondrion. Mitochondrial disorder MELAS: Mitochondrial myopathy, Encephalopathy, Lactic Acidosis and Stroke. Progressive neurodegenerative disorder. Symptoms: Muscle Weakness, episodic seizures and headache, hemiparesis, vomiting and dementia. Diagnosed by muscle biopsy. Single point mutations in several genes MTTL1 – tRNA translates codon as Phe instead of Leu during mitochondrial protein synthesis MTND1, MTND5 – NADH dehydrogenase (Complex 1) LHON: Leber’s hereditary optic neuropathy. Much more common in males. Bilateral, painless, loss of central vision and optic atrophy. >90% of the mutations are in MTND1, MTND4, MTND5, MTND6 and MTCYB NADH dehydrogenase subunits 1,4,5 and 6 Cytochrome B INBORN ERRORS OF METABOLISM ‘One gene, one enzyme’ concept. Mostly autosomal recessive or X linked diseases, over 200 known. Defective proteins are mostly enzymes. UK newborn screening programme Phenylketone urea (PKU), congential hypothyroidism, sickle cell disorders, cystic fibrosis, MediumChain Acyl-CoA Dehydrogenase Deficiency. PKU: Severe mental retardation and convulsions Blond hair/blue eyes; eczema Phenylalanine hydroxylase deficiency Phenylalanine accumulates and is converted to phenylpyruvic acid - excreted in urine Tyrosine deficiency - reduced melanin Newborn screening for elevated levels of phenylalanine in blood Remove phenylalanine from diet Pregnant women have to avoid phenylalanine (present in aspartame). MCAD Deficiency: Medium-Chain Acyl-CoA Dehydrogenase Commonest disorder of fatty-acid oxidation Episodic hypoketotic hypoglycaemia Commonly presents > 3 months Can present as coma, metabolic acidosis, encephalopathy Sudden death can occur, with a 25% mortality rate in undiagnosed cases MCAD gene is called ACADM Detected using blood spot test. Maintenance of adequate calorie intake to prevent need for fatty acid oxidation. Avoidance of fasting (<12 hours), children given teaspoons of honey. L10 – Cancer in families and individuals 1) Explain the difference between somatic and germline mutations Somatic mutations: cause sporadic cancer cases, caused by alterations in somatic tissue. Germline mutations: 1% of cases of cancer are initiated by the inheritance from one parent (or occasionally both) of a mutation in germline tissue, usually in a tumour suppressor (hit 1) 2) Understand why genetic changes cause cancer and describe the 2 main classes of cancer gene Cancer is driven by an accumulation of genetic changes that lead to altered levels of transcription or aberrant gene transcripts resulting protein changes activate signal transduction pathways that confer a selective advantage to the cell. Commonly affected pathways include those that control cell cycle, proliferation, apoptosis, and adhesion ONCOGENES and TUMOUR SURPRESSORS Normal oncogene functions: Growth and proliferation. E.g. Growth factors, transcription factors and tyrosine kinases. Normal functions of TS genes: Regulating cell division. DNA damage checkpoints (damage=no division), apoptosis and DNA repair. 3) Understand the contribution of chromosome rearrangements to the formation of gene fusions and their contribution to oncogenesis. Sporadic malignancy: Acquired chromosome abnormalities and oncogenic fusion genes as disease markers in patient management Most tumour suppressor genes require damage to both alleles for tumorigenic effects. Hit1 reduces transcript/protein level but is insufficient to cause a phenotypic effect. Requires inactivation of second allele (hit 2) causing total loss of transcription for malignant phenotype to be conferred. “2-hit model” A few tumour suppressor genes only require damage to one allele. Single hit causes reduction in transcription and in level of protein product which for these genes is sufficient to have a biological effect via “haploinsufficiency” Loss of Heterozygosity (LOH): describes a region of apparent homozygosity, probably a deletion, in cancer tissue that may mark the location of a TS gene. (i) a historical method of analysing stability of cancer genomes (ii) looking for location of TS genes (iii) another term for deletion (iv) unmasking of mutated copy of TS gene. 4) Discuss how inherited mutations in BRCA1 and BRCA2 genes influence risk of breast and ovarian cancer 2-4% of breast cancer cases are caused by germline mutation of BRCA1 or BRCA2 genes (“hit 1”). Inactivation of second allele is usually via somatic deletion. Also confer increased risk of ovarian cancer BRCA2 mutations also predispose to breast cancer in men Normal function of BRCA1 and BRCA2 is DNA repair, specifically a process called homologous recombination. A truncated/non-functional protein causes impaired DNA repair, so mistakes or damage go uncorrected. Impaired DNA repair is a common theme in cancer. 5) Outline how defects in cell division or DNA repair influence risk of colorectal cancer 2 most common syndromes are caused by inheritance of one mutated allele of a TS gene: 1) FAP (familial adenomatous polyposis) • Characterised by the growth of 1000s of intestinal polyps, one or more of which is likely to become cancerous • >1% of all colorectal cancers • Mutation of APC (adenomatous polyposis coli) gene • APC controls cell division • Virtually 100% lifetime risk of cancer 2) Hereditary non-polyposis colorectal cancer (HNPCC or Lynch syndrome) • 3% of all cases, • Most common inherited form (90% of familial cases) • Mutation of MLH1 or MSH2 (DNA repair genes) • Lifetime risk of cancer 80% 6) Explain, using an example, how chromosome translocations are used to quantify residual disease in some leukaemias. Cytogenetics and leukaemia Our knowledge of contribution of gross chromosomal rearrangements to cancer pathogenesis comes from “cytogenetic” (branch of genetics that is concerned with the study of the structure and function of the cell, especially the chromosomes) investigations of malignant tissue This knowledge is most extensive in haematological malignancies (leukaemias and lymphomas) for 2 main reasons 1) Generally leukaemic genomes are more stable than those of solid tumours – therefore easier to pinpoint pathogenetic changes driving disease 2) Relative ease of performing cytogenetics on haematopoeic circulating cells Chronic Myeloid Leukaemia A clonal myeloproliferative (a group of diseases of the bone marrow in which excess cells are produced) disorder of the pluripotent haematopoeic stem cell (form the cellular components of blood) leading to an overproduction of mature granulocytes. 1 to 2 cases per 100,000 15% of all adult leukaemias Triphasic - indolent chronic phase, accelerated and terminal acute stage Consistent pathogenomic marker is a translocation between chromosomes 9 and 22 resulting in a fusion gene called BCR-ABL1 Targeted molecular therapy for CML: Imatinib (Glivec) – an effective tyrosine kinase inhibitor (TKI) The amount of BCR-ABL1 mRNA in a peripheral blood sample is quantified very precisely in a biochemical assay called a polymerase chain reaction (PCR) Acute promyelocytic leukemia (APML/AML-M3) RARα is a member of the nuclear family of receptors; its ligand, retinoic acid is a form of Vitamin A and acts as a regulator of DNA transcription The translocation product is the PML-RARα fusion protein – binds too strongly to DNA via enhanced interaction with co-repressor molecules, blocking transcription APML responds to all trans retinoic acid (ATRA) therapy, a vitamin A derivative. ATRA dissociates corepressors allowing normal transcription and cell differentiation ATRA is not the same as other chemotherapy- it does not kill cells. It is effective when taken continuously but residual stem cells remain Like CML, APML is monitored by cytogenetics and/or FISH and/or RQ-PCR 7) Explain with examples what is meant by a “pharmacogenomic marker” Pharmacogenomics: an emerging branch of pharmacology which deals with the influence of genetic variation on drug response In cancer treatment, pharmacogenomic tests are used to identify which patients are most likely to respond to certain cancer drugs based on the presence or absence of particular somatic mutations. In summary… • Cancer caused by abnormalities of tumour suppressors or oncogenes • TS genes usually require “2 hits” the second of which is often a deletion (manifesting as LOH) • Usually sporadic but can be inherited – some genetic causes with obvious mendelian inheritance are well characterised • Somatic abnormalities, particularly those involving a novel fusion gene can be used to monitor therapy (if successful therapy available) • Certain somatic abnormalities confer resistance or response to new targeted therapies – “Pharmagogenomics” L11 – Analysis of nucleic acids Personalised medicine- HER2 and breast cancer Overexpression of HER2 leads to more aggressive breast cancer (involved in cell growth and proliferation) 20% of breast cancer is Her2 positive- more aggressive Drugs (biologic therapy) have been developed specifically for cancer where individuals have a Her2 mutation e.g. Trastuzumab (Herceptin) Potential in future for personalised medicine from personal genome… DNA cloning A method of selectively amplifying DNA sequences of interest to generate homogenous DNA populations Cell-based DNA cloning (in vivo) 1) Construction of recombinant DNA molecules in vitro by: cutting a target DNA and a replicon (sequence capable of independent replication – e.g. plasmid, lambda phage, YAC) with restriction endonucleases, ends of the two DNA sequences are compatible Mixing and joining the DNA fragments by using the enzyme DNA ligase 2) Transformation of the recombinant DNA molecules into host cells (bacteria, yeast) 3) Selective propagation of individual cell colonies on an agar plate. Can use antibiotic markers. 4) Expansion/growth of the cell culture and id of recombinant DNA. Type II restriction endonucleases: enzymes that cleave DNA at specific recognition sequences, normally 4-8 bps and palindromic. The longer the recognition sequence, the less common. One half of bacterial restriction-modification systems. Host DNA is protected by methylation of a base in the RE site by a specific methylase - RE will only cleave unmethylated DNA from invading organisms, not host DNA Nucleic acid hybridisation A method for detecting specific nucleic acid sequences in which homologous single-stranded DNA or RNA molecules combine to form double-stranded molecules Standard assay involves a labelled ( * ) nucleic acid probe to identify homologous related target molecules in a mixture of unlabelled nucleic acids Hybridisation assays Target DNA (e.g. from an agar plate or gel) is immobilised on a solid support – nylon or nitrocellulose membrane - which readily binds single-stranded nucleic acid (e.g. denatured DNA or mRNA) Hybridised with a solution of (radioactively or fluorescently) labelled (*) probe. Blotting: DNA can be isolated from the gel or transferred to a membrane to form a replica for hybridisation with a labelled probe ( * ) detected by exposure of photographic film. Southern blot hybridisation (DNA target and DNA probe) (after Ed Southern) Northern blot hybridisation (RNA target and DNA probe) Colony blot hybridisation (bacterial DNA target, DNA probe) Tissue in situ hybridisation (RNA target and RNA probe) Chromosome in situ hybridisation (Chromosome target and DNA probe) Reverse hybridisation – Microarrays (immobilised DNA or oligonucleotide probe, target DNA solution) In situ hybridisation can locate genes on chromosomes. Melting temperature and hybridisation stringency • Denaturation of a probe DNA is achieved by heating until the hydrogen bonds between the bases holding the two strands together are disrupted • The energy needed to do this depends on: – Strand length: longer strand = more hydrogen bonds to break – Base composition: G-C pair has one more hydrogen bond than A-T, so harder to break – Chemical environment: • Monovalent cations (Na+) stabilise the DNA duplex (double stranded) by neutralising charge on phosphate backbone • denaturants (formamide / urea) destabilise the DNA duplex Melting temperature (Tm) - measure of nucleic acid duplex stability – Midpoint temp. of transition from double stranded (DS) to single stranded (SS) forms of nucleic acid – For mammalian genomic DNA (40% GC) this is ~87oC Hybridisation is carried out at temperatures <25oC below Tm Hybridisation stringency (i.e. the power to distinguish between related sequences) increases with: – Increase in temperature – Decrease in Na+ concentration reaction conditions, notably temperature and salt, that dictate the annealing of single-stranded DNA/DNA, DNA/RNA, and RNA/RNA hybrids High stringency, duplexes form only between strands with perfect one-to-one complementarity Lower stringency allows annealing between strands with some degree of mismatch between bases Cell-free DNA cloning Polymerase Chain Reaction (PCR): In vitro method to allow selective amplification of a specific target DNA within a heterogeneous collection of DNA sequences PCR Method: • Some sequence information is needed to design 2 primers (15 - 25 nucleotides in length), one complimentary to each strand of the DNA to be copied • Primers are specifically annealed to heat denatured DNA by lowering temperature • Thermostable Thermophilus aquaticus DNA polymerase + dNTPs extend 5’->3’ from the primers and generate new strands • Denature, and repeat cycle many times. Denature 94oC Anneal 50-60oC Extend 72oC PCR Primers: around 20 nucleotides for complex genomic DNA target. Avoid tandem repeats as they can form hairpins. Avoid complementarity at 3’ ends as primer dimers can form. PCR uses: • • • • • • • Typing genetic markers (Restriction Fragment Length Polymorphisms) Detecting point mutations – restriction site changes, Allele-specific amplification cDNA cloning Genome walking Gene expression – Reverse Transcription-PCR (reverse transcribe mRNA to DNA using oligodT [binds to polyA tail], then amplify) Introducing mutations experimentally (base mismatches) DNA sequencing • DNA microarrays DNA (oligonucleotide) Microarrays A DNA (or oligonucleotide) microarray is a collection of microscopic DNA (or oligonucleotide) spots, commonly representing single genes, robotically arrayed on a solid surface, e.g. a glass slide Qualitative or quantitative measurements with DNA microarrays utilize the selective nature of DNA-DNA or DNA-RNA hybridisation under high-stringency conditions, with fluorophore-based detection DNA arrays are commonly used for expression profiling, i.e. monitoring expression levels of thousands of genes simultaneously, or for comparative genomic hybridization • mRNA or gene expression profiling • SNP detection arrays - looking for Single Nucleotide Polymorphisms in the genome of populations Green – gene more highly expressed in normal cells Red - gene more highly expressed in cancer cells Yellow – gene equally expressed L12 – Prenatal diagnosis of genetic disease • Indications for Prenatal Diagnosis High Risk of Aneuploidy (abnormal no. chromosomes): High risk on Down Syndrome screening. Previous aneuploid fetus. Maternal request eg.Age Known Genetic Disorder: Achondroplasia, Cystic Fibrosis, Haemoglobinopathies, X Linked disorder, Parental Balanced Translocation Structural Anomaly detected in Fetus on Routine Ultrasound Screening • • Ultrasound detection of anomalies Antenatal Screening for Aneuploidy (Down Syndrome) Maternal age, nuchal translucency and serum screening. Combined test at 11-14 weeks. 90% detection rate, 5% false positive rate. • Prenatal Testing Chorionic villus, amniocentesis (>15 weeks) and foetal blood test. Cytogenetic Techniques Cytogenetic analysis: Fetal cells concentrated in centrifuge. Cells cultured in multiple cultures (14 days) Non-Invasive prenatal testing Cell-free foetal DNA (cffDNA) Derived from placental tissue and found in maternal circulation >5 weeks gestation, accounts for 510% of total free DNA cffDNA rapidly cleared from maternal circulation within 30min of delivery cffDNA is made up of short fragments of DNA The whole of the fetal genome is represented in cffDNA If fetal DNA could be studied from maternal circulation: » » » » No risk of miscarriage Reduced Maternal anxiety Performed early Difficult to extract pure cffDNA from maternal cell free DNA Unreliable in Multiple pregnancies Can give false results in early pregnancy if “Vanishing Twin” Rarely placental tissue different from fetal DNA (Mosaicism) cffDNA in Rhesus Disease Three rhesus proteins: C(c), D(d) and E(e) 15% Caucasian Rh d 2% Asian Rh d 5% Afro-Caribbbeans Rh d <1% Chinese Rh d Routine management of Rhesus negative women during pregnancy ALL RHD NEGATIVE WOMEN No antibody detected Anti D at 28, 34 and 40 weeks. Antibody detected Monitored with weekly scans and blood tests. Clinical use for RhD genotyping Genotyping possible from maternal blood. If RhD gene is found in RhD Negative maternal blood, then it must have come from RhD Positive foetus If no RhD gene found in maternal blood and other fetal specific genes found then fetus must be RhD Negative Now all RhD negative women with antibodies are tested at 12 weeks – Only pregnancies with RhD positive foetus need monitoring Other uses for cffDNA Non-invasive prenatal testing: Identify foetal genes not found in maternal circulation, sex determination, finding gene mutations. Sex determination: targeting Y chromosome material - DYS14 or SRY. Conditions that are X-linked Duchene muscular dystrophy (DMD) and fragile X syndrome. Endocrine conditions associated with ambiguous genitalia Congenital adrenal hyperplasia (CAH) Down syndrome screening Maternal Ch21 cffDNA. All studies to date are performed on “High Risk Women”- Results in “Low Risk” population may be less accurate Cost of Next Generation Sequencing still high: extremely accurate, generates a lot of data meaning can detect small differences. NIPD doesn’t look for other Chromosomal anomalies: Even if NIPD normal and structural anomaly in fetus still needs Amnio Ethical issues: Informed Consent, Social pressure to have test as no risk, Social pressure to abort L13 – The future of genomic medicince Advances in genomic medicine • • • • ‘Next generation’ DNA sequencing Finding the causes of monogenic disease Pharmacogenetics Risk of common, complex diseases Personalised healthcare • • • Direct-to-consumer genetic testing Ethical issues Future perspectives • • • • Embryo testing Preimplantation genetic diagnosis (PGD) Uses and limitations Ethical issues Cost of genome/DNA sequencing has been dramatically reduced. Applications of whole genome (or whole-exome) sequencing - Identify genetic changes in cancer cells - Identify novel gene mutations in monogenic disease - Catalogue all genetic variation in populations Miller syndrome: multiple malformation syndrome, cupped ears and missing toes. Caused by mutation on DHODH gene. Schinzel-Giedion syndrome: severe mental retardation, multiple congenital abnormalities, characteristic appearance. Cause by mutation on SETBP1 gene. Pharmacogenetics (cont..) Studying the genetic basis for the difference between individuals in response to drugs. E.g. Type 1 diabetes can be misdiagnosed for maturity onset diabetes of the young (MODY) Genome Wide Association Studies (GWAS) Can identify the many genetic variants responsible for common, complex traits and diseases. Direct to consumer (DTC) genetic tests For monogenic disease: can give carrier status information, predict risk of late onset disease. Must have a counselling service. For complex disease: often have limited clinical utility, can cause undue alarm, false reassurance, data privacy concerns. Personal Genomes All variants may one day be able to be identified in one analysis. PGD: Pre-implantation genetic diagnosis. Test IVF embryos for disease before implantation. Tests include FISH and PCR. Ethical issues: discarding embryos, disability rights arguments, designer babies (?) and eugenics. Limitations: requires use of in vitro fertilisation (IVF): physically and emotionally demanding - and expensive Only suitable for diseases where genetic/chromosome abnormality is known Can only select for traits that are present/absent in embryos obtained. Permitted in the UK: Severe early onset genetic disease, eg. Tay Sachs Severe late onset conditions, eg. Huntington disease Disease with incomplete penetrance, eg. hereditary breast cancer (BRCA1/2 mutations) To choose a tissue-matched baby that can provide umbilical cord blood to treat a sick sibling. Provides stem cells. Choosing sex for non-medical reasons is not allowed L14 – Can genes make us fat? Obesity: Syndromic, monogenic and common obesity. Defines as a BMI ≥ 30kg/m2 Morbid obesity ≥ 40kg/m2 Necessity of fat Storge of food and water Insulation Support and protection of vital organs Source of humans, regulator of reproduction Sexual signalling Regulator and fueller of the immune system Source of new immune cells Aids would healing BMI – body mass index Doesn’t take into account ethnicity, body weight is affected by muscle/fat ratio as muscle heavier than fat. CAUSES: 1. 2. 3. 4. Lack of physical activity High density calorie diet Stress (cortisol hormone) Gene variations – behaviours and physiology are controlled/affected by genes. Genetic affects individual responses to the obesogenic environment. SYNDROMIC OBESITY Prader-Wili syndrome most common. Imprinting defect, paternal deletion or maternal isodisomy (both sex chroms from mum) MONOGENIC OBESITY Leptin hormone produced by fat cells. Travels to hypothalamus, centre for hunger control. Control hunger. Experiment where 2 mice were joined together, one fat one thin. Thin mouse got leptin from obese mouse and gained weight. Evidence for blood born factor controlling obesity. No leptin hunger, obesity, no puberty, poor growth, low thyroid activity, immune problems. Most fat people have LOTS of leptin. If leptin receptors aren’t working, leptin is unable to control hunger. Patients cannot be treated with leptin. MC4R (melanocortin 4 receptor) :most common single-gene form of obesity (monogenic). PC1 – Recessive obesity. Pro-opiomelanocortin gene: dominant mutation. Hunger Obesity Red hair Low adrenal activity COMMON OBESITY GWAS identified single nucleotide polymorphisms. Explain only a small proportion of common obesity risk. Contribution to genetic component of BMI estimated to be low <5% Key points 1) Common diseases may have a range of causes, some very strongly genetic 2) Progress in genetics is very fast 3) Genetic cause does not imply that there’s nothing that can be done 4) Do not suspend evidence-based medicine because of stigmatisation of particular patients