Anomalous Coronary Artery: Nursing Care Plan & Case Study
advertisement
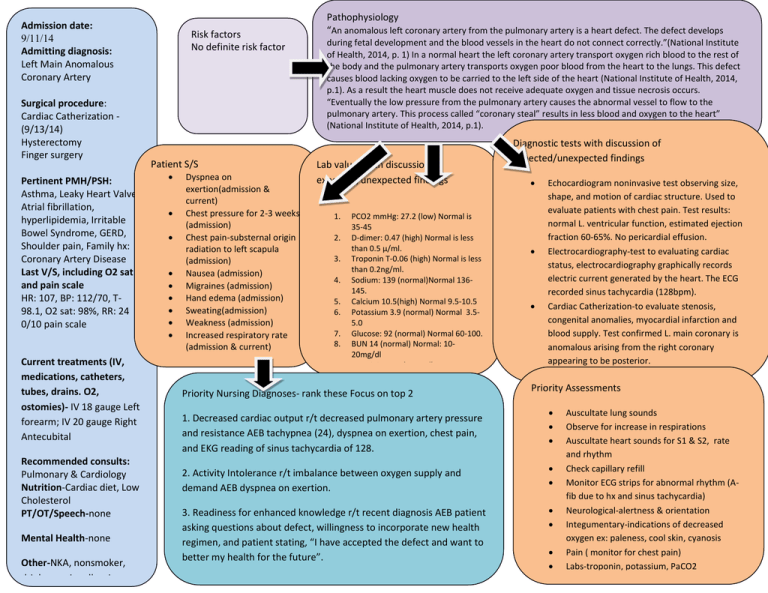
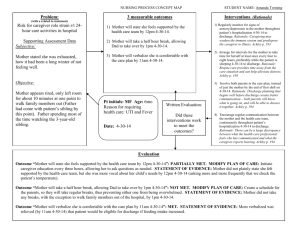
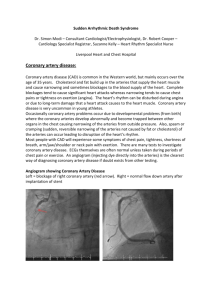
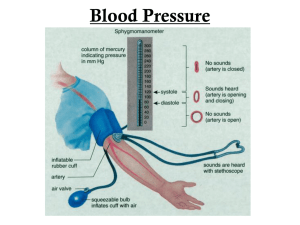
Admission date: 9/11/14 Admitting diagnosis: Left Main Anomalous Coronary Artery Surgical procedure: Cardiac Catherization (9/13/14) Hysterectomy Finger surgery Pertinent PMH/PSH: Asthma, Leaky Heart Valve Atrial fibrillation, hyperlipidemia, Irritable Bowel Syndrome, GERD, Shoulder pain, Family hx: Coronary Artery Disease Last V/S, including O2 sat and pain scale HR: 107, BP: 112/70, T98.1, O2 sat: 98%, RR: 24 0/10 pain scale Current treatments (IV, medications, catheters, tubes, drains. O2, ostomies)- IV 18 gauge Left forearm; IV 20 gauge Right Antecubital Recommended consults: Pulmonary & Cardiology Nutrition-Cardiac diet, Low Cholesterol PT/OT/Speech-none Mental Health-none Other-NKA, nonsmoker, drink occasionally wine Risk factors No definite risk factor Patient S/S Dyspnea on exertion(admission & current) Chest pressure for 2-3 weeks (admission) Chest pain-substernal origin radiation to left scapula (admission) Nausea (admission) Migraines (admission) Hand edema (admission) Sweating(admission) Weakness (admission) Increased respiratory rate (admission & current) Pathophysiology “An anomalous left coronary artery from the pulmonary artery is a heart defect. The defect develops during fetal development and the blood vessels in the heart do not connect correctly.”(National Institute of Health, 2014, p. 1) In a normal heart the left coronary artery transport oxygen rich blood to the rest of the body and the pulmonary artery transports oxygen poor blood from the heart to the lungs. This defect causes blood lacking oxygen to be carried to the left side of the heart (National Institute of Health, 2014, p.1). As a result the heart muscle does not receive adequate oxygen and tissue necrosis occurs. “Eventually the low pressure from the pulmonary artery causes the abnormal vessel to flow to the pulmonary artery. This process called “coronary steal” results in less blood and oxygen to the heart” (National Institute of Health, 2014, p.1). Lab values with discussion of expected/unexpected findings 1. 2. 3. 4. 5. 6. 7. 8. 9. PCO2 mmHg: 27.2 (low) Normal is 35-45 D-dimer: 0.47 (high) Normal is less than 0.5 µ/ml. Troponin T-0.06 (high) Normal is less than 0.2ng/ml. Sodium: 139 (normal)Normal 136145. Calcium 10.5(high) Normal 9.5-10.5 Potassium 3.9 (normal) Normal 3.55.0 Glucose: 92 (normal) Normal 60-100. BUN 14 (normal) Normal: 1020mg/dl Creatinine 0.7 (normal) Priority Nursing Diagnoses- rank these Focus on top 2 1. Decreased cardiac output r/t decreased pulmonary artery pressure and resistance AEB tachypnea (24), dyspnea on exertion, chest pain, and EKG reading of sinus tachycardia of 128. 2. Activity Intolerance r/t imbalance between oxygen supply and demand AEB dyspnea on exertion. 3. Readiness for enhanced knowledge r/t recent diagnosis AEB patient asking questions about defect, willingness to incorporate new health regimen, and patient stating, “I have accepted the defect and want to better my health for the future”. Diagnostic tests with discussion of expected/unexpected findings Echocardiogram noninvasive test observing size, shape, and motion of cardiac structure. Used to evaluate patients with chest pain. Test results: normal L. ventricular function, estimated ejection fraction 60-65%. No pericardial effusion. Electrocardiography-test to evaluating cardiac status, electrocardiography graphically records electric current generated by the heart. The ECG recorded sinus tachycardia (128bpm). Cardiac Catherization-to evaluate stenosis, congenital anomalies, myocardial infarction and blood supply. Test confirmed L. main coronary is anomalous arising from the right coronary appearing to be posterior. Priority Assessments Auscultate lung sounds Observe for increase in respirations Auscultate heart sounds for S1 & S2, rate and rhythm Check capillary refill Monitor ECG strips for abnormal rhythm (Afib due to hx and sinus tachycardia) Neurological-alertness & orientation Integumentary-indications of decreased oxygen ex: paleness, cool skin, cyanosis Pain ( monitor for chest pain) Labs-troponin, potassium, PaCO2 Nursing Diagnosis Decreased cardiac output r/t decreased pulmonary artery pressure and resistance AEB tachypnea (24), dyspnea on exertion, chest pain (on admission) , and EKG reading of sinus tachycardia of 128. Interventions Expected Outcomes (2) 1. The patient will tolerate activity without experiencing severe chest pain or severe dyspnea by the end of the shift. 2. The patient will verbalize 3 actions or precautions in decreasing heart rate by discharge. Evaluation Jlj 1.Outcome #1-Goal met AEB patient ambulating to the waiting room area and to patient room and reporting moderate dyspnea and no chest pain. 2. Outcome #2- Goal met AEB patient verbalizing to nurse 1.healthier food choices such as decaffeinated coffee and tea, 2.taking breaks while ambulating, and 3. incorporating more rest periods during the day absent of activity. Outcome: #1 1. Monitor for symptoms of heart failure and decreased lung sounds. Rationale: “These symptoms are major criteria for Clinical Concept diagnosis of heart failure”(Ackley, 2011, p. 198). Map 2. Administer oxygen as needed per physician’s order. Rationale: “Clinical practice guidelines should be administered to relieve symptoms related to hypoxemia” (Ackley, 2011, p.199). 3.If chest pain is present, have the client lie down, monitor cardiac rhythm, give oxygen, check vital signs, run a monitor strip, medicate for pain, and notify the physician. Rationale: “Prompt assessment of the client with acute coronary symptoms is critical because the incidence of ventricular fibrillation is 15 times greater during the first hour after symptoms of an acute myocardial infarction” (Ackley, 2011, p.199). 4. Observe for chest pain or discomfort and note location, severity, radiation, quality, duration, precipitating and relieving factors Rationale: “Chest pain is often indicative of an inadequate blood supply to the heart, which can compromise cardiac output” (Ackley, 2011, p. 199). 5. Titrate inotropic and vasoactive medications within defined parameters to maintain contractility, preload, and afterload. Rationale: “By following parameters, the nurse ensures maintenance of a balance of medications that stimulate the heart to increase contractility, while maintaining adequate perfusion of the body” (Ackley, 2011, p.199). 6. Schedule rest periods after meals and activities. Rationale: “Rest help lowers arterial pressure and reduce the workload of the myocardium by diminishing the requirements for cardiac output” (Ackley, 2011, p.199) Outcome #2 1.The patient will gradually increase activity when the client’s condition is stabilized by encouraging slower paced activities or shorter periods of activity and take pulse and blood pressure before and after activity. Rationale: “Activity of the cardiac client should be closely monitored” (Ackley, 2011, p.200). 2.Serve small, frequent, sodium-restricted, low-cholesterol meals. Rationale:” Clients with cardiac disease tolerate smaller meals better because they require less cardiac output to digest” (Ackley, 2011, p.200). 3.Serve only small amounts of coffee or caffeine-containing beverages if requested (no more than 4 cups in 24 hrs) if no resulting dysrhythmia. Rationale: “A review of studies on caffeine and cardiac arrhythmias concluded that moderate caffeine consumption does not increase the frequency or severity of cardiac arrhythmias” (Ackley, 2011, p.200). 4.Assess for the presence of anxiety in the patient. Rationale: “Descriptive studies have found higher complication rates following infarction in clients with increased anxiety”(Ackley, 2011, p.201). 5.Include significant others in client teaching opportunities. Rationale: “A study assessed the influence of significant other support in HF client care found increased support was moderately associated with medication and dietary adherence, among other aspects of care” (Ackley, 2011, p.205). 6.Teach stress reduction such as controlled breathing and muscle relaxation techniques. Rationale:” The HF patients participating in regular relaxation reported greater improvements in fatigue” (Ackley, 2011, p. 206). 7. Teach the client actions, side effects, and importance of consistently taking cardiovascular medications. Rationale: ”Taking medication as directed can help prevent decompensation, rehospitalization, and morbidity” (Ackley, 2011, p. 206). Nursing Diagnosis Activity Intolerance r/t imbalance between oxygen supply and demand AEB dyspnea on exertion. Expected Outcomes (2) 1. The patient will state 3 adverse effects of exercise and symptoms to report immediately to a physician upon discharge. 2. The patient will be able to resume activities of daily living and maintain respiratory rate within normal limits by discharge. Evaluation Outcome #1- Goal Met AEB the patient stating the following symptoms to report to the physician immediately: 1. Increased heart rate 2. Chest pain 3. Fatigue. Outcome #2-Goal partially met AEB the patient having respiratory rate of 24 after ambulation and decreasing to 20 five minutes after the activity. The patient has resumed ADLs with modified health regimen AEB taking a shower, resuming personal care, engaging in low energy activities. Interventions with rationale and citation Outcome #1 1.When getting a patient up observe for signs of intolerance such as nausea, pallor, dizziness, visual dimming, and impaired consciousne vital signs. Rationale:” As a result of blood pooling in the extremities symptoms of central nervous hypoperfusion may occur” (Ackley, 201 2.Instruct the client to stop the activity immediately and report to the physician if the client is experiencing the following symptoms: Ne intensity or increased frequency of discomfort; tightness or pressure in chest, back, neck, jaw, shoulders, and/or arms; palpitations, dizz unusual and extreme fatigue.” Rationale: These are common symptoms of angina and are caused by a temporary insufficiency of corona If symptoms last longer than 5-10 minutes, the client should be evaluated by a physician”(Ackley, 2011, p.120). 3. Monitor and record the client’s ability to tolerate activity: note pulse, blood pressure, monitor pattern, dyspnea, use of accessory mu color before, during, and after the activity. If the following signs occur during activity, the activity should be stopped immediately: onset discomfort, dyspnea, excessive fatigue, lightheadedness, confusion, cyanosis, excessive rise in blood pressure (systolic > 180mmHg or di >110mmHg), bradycardia (drop in heart rate >10 bpm or <50 bpm, or increased heart rate above 100 bpm). Rationale: “Pulse rate and a oxygenation indicate cardiac/exercise tolerance; pulse oximetry identifies hypoxia” (Ackley, 2011, p.120). 4. Monitor a client’s respiratory response to activity by observing for symptoms such as dyspnea, use of accessory muscles, nasal flaring facial distress, and skin tone changes. Rationale: “A respiratory rate exceeding these parameters along with physiological changes demo significant physiological alteration” (Ackley, 2011, p. 124). 5. Allow for periods of rest before and after planned exertion periods such as meals, baths, treatments, and physical activity. Rationale: and emotional rest help lower arterial pressure and reduce the workload of the heart” (Ackley, 2011, p. 122). 6. Teach the client/ family the importance of and methods for setting priorities for activities, especially those having a high energy dema in patients and patients’ families on realistic expectations. Rationale: “Unrealistic expectations provoke guilty feelings in the clients, lead that can exceed the client’s energy capacity” (Ackley, 2011, p.123). Outcome #2 1.Teach the client/ family the importance of and methods for setting priorities for activities, especially those having a high energy dema patients and patients’ families on realistic expectations. Rationale: “Unrealistic expectations provoke guilty feelings in the clients, leading can exceed the client’s energy capacity” (Ackley, 2011, p.123). 2.Refer to heart failure program or cardiac rehabilitation program for education, evaluation, and guided support to increase activity and Rationale: “A carefully monitored exercise program can improve both exercise capacity and quality to life in heart failure patients” (Ackle 3.Observe for pain before activity. If possible, treat pain before activity. Rationale:” Pain restricts the client from achieving a maximal ac level”(Ackley, 2011, p. 121). 4.Obtain any necessary assistive devices or equipment needed before ambulating the client. Rationale: “Assistive devices can help increa (Ackley, 2011, p.121.) 5.Assess the home environment for factors that contribute to decreased activity tolerance such as stairs and distance. Refer to occupati needed to assist the patient resume activities of daily living. Rationale: “During hospitalization, clients and families often estimate energ home inaccurately because of the availability of hospital staff” (Ackley, 2011, p. 123). 6.Provide the client/family with resources such as senior centers, exercise classes, educational and recreational programs that can aid in appropriate activity. Rationale: “ Social isolation can be an outcome of and contribute to activity intolerance” (Ackley, 2011, p.123). Nursing Process Concept Map References: Ackley, B.J., & Ladwig, G.B. (2011). Nursing diagnosis handbook: An Evidence-Based Guide to Planning Care. (9th ed.). St. Louis, MO: Mosby Elsevier Dionne et. al. (2013). A rare case of anomalous origin of the left main coronary artery in an adult patient. Journal of Cardiothoracic Surgery. 8(15), 1-3. Retrieved from http://www.cardiothoracicsurgery.org/content/8/1/15/abstract National Institute of Health. (2014). Anomalous left coronary artery from the pulmonary artery. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/article/007323.htm Article Summary This article examines a patient admitted to the hospital with anomalous left coronary artery (Dionne et. al, 2013, p.1). The article also explain the pathophysiology and procedures associated with the anomaly. According to the article, “anomalous left coronary artery (ALCAPA) is rare congenital anomaly occurring in 1/300,000 births” (Dionne et. al, 2013, p.1). The left to right shunt as known as “coronary steal” that develops causes decreased myocardial perfusio and volume overload. Most patients present with heart failure secondary to myocardial ischemia or die during infancy (p.1). The patient mentioned in this article the oldest person reporting ALCAPA. A 44 year old man went to the hospital with the chief complaint of dyspnea on exertion and mild chest pain in 2007. The physician suggested surgery and the patient refused at first because the symptoms had been tolerated well. A coronary angiography lead to the diagnosis of ALCA (Dionne et. al, 2013, p.1). At the age of 48, the man experienced increased dyspnea on exertion but pre-operative coronary angiography discovered the symptom were directly linked to ALCAPA. Left ventricular ejection fraction was normal on the echocardiography (p.1). An elective surgery was scheduled for re-implantatio the left main coronary artery. During surgery, cardiopulmonary bypass (CPB) was started. “After mobilization of the proximal coronary vessels, the left main coronary artery was double ligated at its origin on the pulmonary artery without signs of ischemia, the tissues were fragile, and small epicardial collaterals had formed” (Dionne et. al, 2013, p.1). In order to provide dual coronary perfusion, the surgeon performed on pump beating CABG of the left anterior descending coronary with a saphenous vein graft from the calf (p.2). The patient was transitioned from CPB, transferred to ICU, and extubated that same evening, and discharged 6 days later with anticoagulant therapy (p.2). The case is interesting from a medical standpoint because most patients rarely live past infancy and live shorter lifespans with correction. Physicians believe patients can live into adulthood with the anomaly without extensive myocardial ischemia due to the collatera flow from RCA. Re-implantation of the left main coronary to the aorta is the most physiological correction. However, left coronary artery ligation in combination CABG are the preferred surgery if re-implantation is possible because it provides dual coronary flow (Dionne et. al, 2013, p.2). This information in this article correlates with my patient because she has the same anomaly and is living at 51 years old without any surgery thus far. Bot individuals presented to the emergency department with dyspnea on exertion and chest pain. During my assessment, the patient told me she never had serious symptoms before the hospitalization. She played sports during high school, had children, worked currently, never smoked, and participated in extracurricular activities currently. The echocardiogram of my patient indicated normal ejection fraction of 60-65% like the man presented in this article. The cardiac catherizatio performed on my patient revealed the left main anomalous arising from the right coronary artery ostia and it appeared to be posterior. Re-implantation is not an indication at this time. The physician discharged the patient with clopidogrel (Plavix) 75mg, tab, PO, daily with a follow up stress test. The physicians, nurses, and myself were amazed by how her body has compensated and her overall health condition. I was surprised she never suffered heart problems before. She played h energy sports, gave birth twice, and works at a job requiring walking long distances. All these activities placed high demand on the heart and resulted in sudden death. Faculty comment on Clinical Care Map Article Reference & Summary Faculty Comments: Faculty comment on Nursing Process Map