11. Structure and function of the respiratory system

Section A: Applied Anatomy and
Physiology
11. Structure and function of the respiratory system
Syllabus
• Structure of the nasal passages, trachea, bronchii, bronchioles, and alveoli
• Lobes of the lung and pleural membrane
• Mechanics of breathing at rest and during exercise
• Respiratory muscles, to include: diaphragm, external intercostals, sternocleidomastoid, pectoralis minor, internal intercostals, and abdominal muscles
• Control of ventilation
• Definitions, values and measurement of respiratory volumes at rest and during exercise
• Effect of exercise on respiratory volumes and pulmonary ventilation
• Gaseous exchange, partial pressures and tissue respiration
• The effect of altitude on the respiratory system
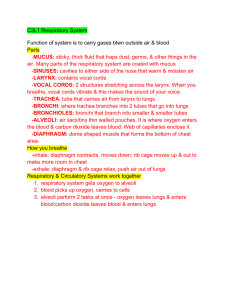
External Respiration
• Involves the movement of gases into and out of the lungs.
• The exchange of gases between the lungs and blood is known as pulmonary diffusion.
Nasal Passages
• Nasal cavity is divided by a cartilaginous septum that forms the passages.
• Interior structures aid the process by:
– Mucous membranes and blood capillaries moisten and warm the inspired air
– Ciliated epithelium filters and traps dust particles
– Small bones (chonchae) increase the surface area to improve efficiency
Oral Pharynx and Larynx
• Air entering the larynx passes over the vocal chords and into the trachea
• Swallowing – the larynx is drawn upwards and forwards against the base of the epiglottis
(preventing entry of food)
Trachea
• Approx. 10cm in length and lies in front of the oesophagus.
• Composed of 18 ‘rings’ of cartilage, which are also lined by a mucous membrane and ciliated cells.
• Extends from larynx and directs air into the right and left primary bronchi.
Bronchi and Bronchioles
• Trachea divides into right and left bronchi, which further subdivide into lobar bronchi
– Three feeding the lobes of the right lung
– Two feeding the lobes of the left lung
• Further subdivision of these form bronchioles
• Bronchioles enable the air to pass into the alveoli via the alveolar ducts
Alveoli
• Responsible for the exchange of gases between the lungs and the blood
• The alveolar wall are extremely thin, are lined by a film of water
– Essential for dissolving oxygen from inspired air
– Alveoli walls also contain elastic fibres further increasing surface area
– Surrounding each alveolus is an extensive capillary network
Mechanics of Breathing
Breathing
• Lungs are surrounded by pleural sacs containing pleural fluid, which reduces friction
• Sacs are attached to both the lungs and the thoracic cage, which enables the lungs to inflate and deflate as the chest expands and flattens
Inspiration
• Active
• Occurs as a result of contraction of;
– External intercostals
– Diaphragm
• As the chest expands through these muscular contractions, the surface tension created by the film of pleural fluid causes the lungs to be pulled outwards
Inspiration During Exercise
• Additional muscles;
– Sternocleidomastoid
– Scalenes
– Pectoralis major
Expiration
• Generally a passive process
• During exercise, the process becomes more active;
– The internal intercostals
– Abdominals
– Latissimus dorsi
Respiratory Regulation
• Controlled by nervous system
• Basic rhythm is governed and co-ordinated by the respiratory centre (medulla)
• Inspiration generally lasts up to 2 seconds after which impulses cease and expiration occurs by elastic recoil of lungs
Factors Controlling Rate of Breathing
• Chemoreceptors
– CO2 levels
• Proprioceptors and Mechanoreceptors
• Stretch receptors
– Hering-Breur reflex (prevents overinflation)
• Thermoreceptors
– Temperature of blood
–
• Baroreceptors
– State of lung inflation
Neural Control
The respiratory centre in the medulla of the brain controls breathing.
It is made up of two main areas:
• The inspiratory centre is responsible for the rhythmic cycle of inspiration and expiration
• The expiratory centre is inactive during quiet ventilation. When the rate and depth of breathing increases (detected by stretch receptors in the lungs) the expiratory centre inhibits the inspiratory centre and stimulates expiratory muscles.
Cont.
• In most circumstances the neural control of breathing is involuntary
• The resp centre sends out impulses via the phrenic and intercostal nerves to the respiratory muscles
• The muscles are stimulated for a short period, causing insipration
• Then when the stimulus stops, expiration occurs
Other factors influencing the neural control of breathing include:
1. A large drop in oxygen tension.
This is monitored by chemoreceptors in the aorta and carotid arteries and results in an increase in the rate and depth of breathing.
2. A rise in blood pressure, monitored by baroreceptors in the aorta and carotid arteries, resulting in a decrease in ventilation rate
3. Proprioceptors in the muscles responding to movement stimulate the respiratory centre, increasing the rate and depth of breathing
4. The respiratory centre can also be affected by higher centres in the brain, e.g. emotional influences
Chemical Control
• The respiratory centre responds mainly to changes in the chemistry and temperature of the blood
• The most significant factor is a lowering in pH
• This occurs when there is an increase in the amount of
CO
2 being produced by the cells
• The increase is detected by the respiratory centre (in the brain)
• It results in an increase in the rate and depth of breathing
• A rise in body temperature will cause an increase in the rate but not the depth of breathing
Reminder
• Pulmonary diffusion – gaseous exchange at the lungs
• Its functions
– Replenish oxygen
– Remove carbon dioxide
Partial Pressure of Gases
• Central to understanding of gaseous exchange is the concept of partial pressure
• “the individual pressure that the gas exerts when it occurs in a mixture of gases”
• The pressure is proportional to its concentration
• Partial pressures added together = total pressure of gas
Composition of Air
• Nitrogen = 79%
• Oxygen = 20.9%
• Carbon dioxide = 0.03%
• The percentages are obviously the relative concentrations!
Calculating Partial Pressure
Effect of Altitude
Effect of Altitude
• With altitude there is a decrease in atmospheric pressure BUT the percentages of gases within the air remain identical to those found at sea level
• It is the partial pressure of the gases that changes in direct proportion to an increase in altitude
Effect of Altitude cont.
• E.G. – at rest the pO
2 of arterial blood is approx
100mmHg, while in the resting muscles and tissues it is 40mmHg.
• The difference between the two indicates the pressure gradient.
• The pO
2 of arterial blood at an altitude of 8000ft drops to 60mmHg, while that in the muscles remains at 40mmHg!
Altitude Training
• The principle:
– With an increase in altitude, the partial pressure of oxygen in the atmosphere decreases by about a half, causing the body to adapt by INCREASING
RED BLOOD CELL MASS AND HAEMOGLOBIN
LEVELS to cope with a lower pO
2
Altitude Training
• It is widely used by endurance athletes to enhance their oxygen-carrying capacity
• Recent evidence:
– Living at altitude and training at sea level produces the greatest endurance performance
– Can increase the oxygen-carrying capacity of the blood by up to 150%
Altitude Training
• Disadvantages:
– Expensive
– Can cause altitude sickness
• Detraining!
– Due to lack of oxygen , training at higher intensities is difficult
– Any benefits are soon lost on return to sea level
Oxyhaemoglobin Dissociation Curve
http://www.bio.davidson.edu/Courses/anphys/
1999/Dickens/Oxygendissociation.htm
Transport of Oxygen
• Each molecule of haemoglobin can combine with
4 molecules of oxygen
• The amount of oxygen that can combine with haemoglobin is determined by the partial pressure of oxygen
• High pO
2
= complete saturation
• Low pO
2
= saturation decreases
Transport of Oxygen and Dissociation
• Hb is totally saturated at the lungs (alveoli)
• As the pO
2 is reduced, Hb saturation decreases accordingly.
– This is largely due to the increased acidity of the blood (decrease in blood pH), caused by an increase in CO
2 or LA and the increase in body temperature, which causes a shift to the right in the haemoglobin saturation curve.
The Release of Oxygen from
Haemoglobin
• At rest
– The pO2 in the alveoli is approx 100mmHg
– 100% saturation
– In resting muscle and tissue the pO2 is 40mmHg
– 75% saturation
– Means that 25% of the oxygen picked up at the lungs is released into the muscle to help in energy production
The Release of Oxygen from
Haemoglobin
• During exercise
– The pO2 in the alveoli remains at approx
100mmHg
– 100% saturation
– In working muscles the pO2 can be greatly reduced, up to 15mmHg
– 25% saturation
– Means that 75% of the oxygen picked up at the lungs is released into the muscle to help meet the extra energy demands
The Bohr Shift
• Increased oxygen released to tissues!
Gas Exchange at Muscles and Tissues
• High pO2 in arterial blood and relatively low pO2 in muscles causes a pressure gradient
• High pCO2 in tissues and low pCO2 in arterial blood causes a movement of CO2 in opposite direction
• Production of CO2 stimulates the dissociation of oxygen from haemoglobin
• Myoglobin has a much higher affinity for oxygen than haemoglobin
a-VO
2
difference
• The arterial-venous oxygen difference is the difference in oxygen content of the blood in the arteries and the veins.
• It is a measure of the amount of oxygen consumed by the muscles
Lung Volumes
LUNG VOLUME DEFINITION
Tidal volume (TV) Volume inspired or expired per breath
Inspiratory reserve volume
Expiratory reserve volume
Maximal volume inspired following end of resting inspiration
Maximal volume expired following end of resting expiration
Residual volume
(RV)
Volume of air remaining in the lungs at the end of maximal expiration
TYPICAL REST
VALUE
500ml
3100ml
1200ml
1200ml
CHANGE DURING
EXERCISE
Increase
Decrease
Decrease
Remains the same
Lung Capacities
LUNG CAPACITIES
Inspiratory capacity
(TV + IRV)
Vital capacity
(TV + IRV + ERV)
Total lung capacity
(VC + RV)
Minute ventilation
(TV * f)
DEFINITION
Maximum volume of air inspired from resting expiratory levels
The maximum volume forcibly expired following maximal inspiration
The volume of air that is in the lungs following maximal inspiration
The volume of air inspired or expired per minute
TYPICAL REST
VALUE
3600ml
5000ml
6000ml
7500ml
CHANGES DURING
EXERCISE
Increase
Slight decrease
Slight decrease
Dramatic increase
REST
MAXIMAL WORK
Minute Ventilation
= MINUTE VENTILATION TIDAL VOLUME (TV) *
FREQUENCY
(BREATHS/MIN)
500ml * 15
4,000ml * 50
= 7.5L / min
= 200L / min
Adaptive Responses of Respiratory
System to Training
1.
SMALL INCREASES IN LUNG VOLUMES
1.
Result from increased strength in respiratory muscles
2.
IMPROVED TRANSPORT OF RESPIRATORY GASES
1.
Increased amount of RBC’s (haemoglobin)
2.
Increased blood plasma reduces viscosity
3.
ENHANCED GASEOUS EXCHANGE AT THE ALVEOLI AND TISSUES
1.
Increased capillary density
4.
GREATER UPTAKE OF OXYGEN BY THE MUSCLES
1.
Increased myoglobin and mitochondrial density
2.
Increase in a-VO
2 difference