Cultural Competent Health Care
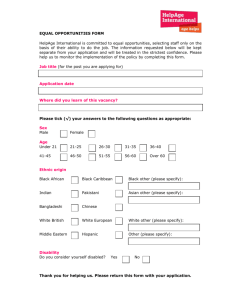
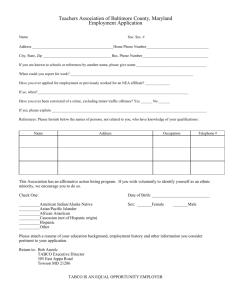
advertisement

Cultural Competent Health Care Agenda • Questions & concerns • Discussion on culture, race, ethnicity, & value • Needs for cultural competent care • Negotiation for dates for individual presentations Shrink the Earth’s Population to 100 • • • • • • 57 Asians 21 Europeans 14 North, Central and South Americans 8 Africans 70 would be non-white, 30 white 70 would be non-Christian, 30 Christian Population in the U.S. Year 2000 • Whites – 69.4% • Black – 12.7% • Hispanic – 12.6% • Asian – 3.8% Year 2050 • Whites – 50% • Black – 14.6% • Hispanic – 24.4% • Asian – 8% US Census Bureau, 2004 Registered Nurses in the U.S. (2000) • 86.6% - non-Hispanic white (US dept of Health & Human Service, 2003) Population in San Jose (2000) • • • • Whites - 47.5% Hispanic - 30.2% Asian - 26.9% Black - 3.5% U.S. Census Bureau (2006) Globalization : Q: How to define globalization? A: Princes Diana’s death Q: How come? A: An English princess with an Egyptian boyfriend crashes in a French tunnel, in a German car with a Dutch engine, driven by a Belgian who was pissed on Scottish whiskey, followed closely by an Italian paparazzi, on Japanese motorcycles, treated by an American doctor, using Brazilian medicines. And this is sent to you by a Israeli, using Bill Gates’ Technology which he stole from the Taiwanese. Minorities Receive Lower Quality Health Care Than Whites • Institute of Medicine, 100 studies reviewed over past 10 yrs. • Full report www.nap.edu/books/030908265X/html • Minorities less likely to receive sophisticated Txs for AIDS • More likely to have leg amputations for diabetes • Poorer relationships with MDs Other Cultural Domains • Folk beliefs/religion - can be confused with “religiosity” • Stereotyping labels - avoid generalizations • Ethnopharmacology - genetic influence, effect, metabolism • Herbal therapies - interactions with meds • Folk healers & treatment approaches, e.g.., hysteria, psychosis Cultural competence & impact on clinical outcomes • Patients fear of being misunderstood or disrespected; • Providers are not familiar with the prevalence of conditions among certain minority groups • Providers may fail to take into account differing responses to medication • Providers may lack knowledge about traditional remedies, leading to harmful drug interactions • Patients may not adhere to medical advice because they do not understand or do not trust the provider; • Providers may order more or fewer diagnostic tests for patients of different cultural backgrounds ethnic disparities in health care • African American women are more likely than European American women to die from breast cancer, despite having a lower incidence of the disease. • Infant mortality rates are 2.5 times greater for African Americans and 1.5times greater for Native Americans than for European Americans. • Influenza death rates are higher for African Americans and American Indian/Alaska Natives/Native Alaskans than they are for European Americans. • Mortality for colorectal cancer is highest for African Americans, followed by Native Alaskans, and then Hawaiians. Needs for cultural competence • American nurses experienced a lack of cultural confidence in caring for culturally diverse populations - Coffman, Shellman, & Bernal (2004) and Hagman (2006) • There were gaps in healthcare providers’ knowledge of other cultures and how to care for them in culturally sensitive ways - Jones, Cason, and Bond (2004) Other evidences • Negative racial stereotypes - rate black patients as more likely to abuse drugs and alcohol, less likely to comply with medical advice, and less likely to participate in cardiac rehab than white patients Van Ryn and Burke (2000) • Less Dx test - physicians were less likely to recommend catheterization procedures for black female patients than white or black male patients if they experienced the same kind of symptoms. Schulman et al. (1999) cultural competence is a process • American Nurses Association published its first guidelines on cultural diversity in nursing curricula in 1986 - understanding the concept of human diversity including cultural and racial variations • The Board of Registered Nursing of California (2006) has required all nursing schools in California to include cultural diversity and competence into their curricula Language barriers and disparity • Utilization of health care services – Fewer doctor visit and less preventive services – More diagnostic test to compensate communication problems • Satisfaction – Less satisfied unless with interpreter • Adherence – Miss the appointment or drop out • Outcomes • Patient education Health Disparities • President Clinton (1998) set the goal – reduce health disparities by the year 2010. • Target areas: (NIH, 2003) – – – – – – Infant mortality, Cancer screening and management, Cardiovascular disease, Diabetes, HIV/AIDS, Immunization Problems with Health Disparities - with cultural factors Flaskerud, J. et al (2002) – a review of 79 articles in the past 5 decades: – Ignorance of certain groups (indigenous peoples) – Inappropriate lump together ie. Hispanic members of disparate groups with their own cultural identity eg., Puerto Ricans, Mexicans, Cubans, Dominicans Aday’s 2010 Priorities Showcase – Needs within vulnerable population • • • • • • • • • High-risk mothers & infants-of-concern Chronically ill & disabled Persons living with HIV/AIDS Mentally ill & disabled Alcohol & other substance abuses Suicide- or homicide-prone behavior Abusive families Homeless persons, Immigrants/refugees Impact of Cultural Competency • • • • • • • More successful patient education Increases in pt’s health care seeking behavior More appropriate testing and screening Fewer diagnostic errors. Avoidance of drug complications Greater adherence to medical advice Expanded choices and access to high-quality clinicians. Culture - Bound Syndromes • A person living within a certain reality • Learned way to interpret the world based on enculturation • Recurrent, locality- specific patterns of aberrant behavior and troubling experiences that may not be linked to a DSM-IV diagnosis Culture Bound Syndromes Group Disorder Explanation Caucasian Anorexia Preoccupied body wt. & image Nervosa Bulimia Binge eating followed by vomiting Low blood Insufficient blood or weakness of blood High blood Blood that is too rich Thin blood Susceptibility to illness African American Culture Bound Syndromes Cont. Group Disorder Chinese/ Koro Southeast Asian Amok Explanation Fear that penis is retracting into body Acute reaction to loss, Culture Bound Syndromes Cont. Hispanic Disorder Explanation Empacho Food clings stomach & intestines: pain Stranger’s attention causes illness in children Mal ojo “evil eye” Susto Anxiety, phobias Culture Bound Syndromes Cont. Group Disorder Explanation Native American Ghost Japanese Wagamama Hallucinations, terror Childish behavior Korean Hwa-Byung Cambodian Koucharang “thinking too much” Multiple somatic & psychological symptoms Headaches, chest pain, palpitations, SOB, insomnia Temporal Relations • Time Orientation • Past, present or future-oriented • Punctuality Negotiation Process • Listen: to the client’s perspective • Teach: from your knowledge in language appropriate for client & family • Compare: similarities & differences, disagree but do not devalue client’s view • Compromise: – if client treatment not harmful, promote – If harmful, explain harm and suggest alternatives The Health Promotion Matrix Gorin, S. & Arnold, J. (1998). Health Promotion Handbook. St Louis: Mosby. P 92 Before Next Class • Take extra care of yourself and your family • Prepare by reading for class: get copies of articles • Decide on group presentation medium for presentation; bring IBM compatible disk one week before if you want to use Power Point for your presentation; limit slides to 30 • Continue work on your group for presentation • Have a great week The End