Hospital Safety: Do race and ethnicity matter?
advertisement

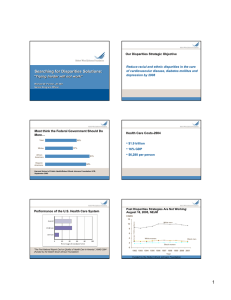
• The NHDR is an annual report to Congress. Hospital Safety: Do race and ethnicity matter? Ernest Moy, MD, MPH Elizabeth Dayton, MA Roxanne Andrews, PhD The Agency for Healthcare Research and Quality The National Healthcare Quality and Disparities Reports Patient Safety Today 44 - 98,000 American lives lost annually Lost incomes, disability, and health care expenditures attributable to medical errors cost a projected $29 billion Institute of Medicine, 2000 Limited research examines racial and ethnic variation in adverse events Romano, Geppert, Davies, et al., Health Affairs, 2003 Coffey, Andrews, Moy, Medical Care, 2005 HCUP SID Disparities Analytic File Patient safety indicators from allall-payer hospital discharge abstract data Adjusted for age, gender, ageage-gender interaction, DRG, and coco-morbidities Sample from 23 HCUPHCUP-SID states* with “good” good” racial/ethnic data Missing data imputed Data weighted to produce national estimates Sample size: about 14.5 million records from about 1700 hospitals • It includes a comprehensive set of measures for healthcare quality and access. • It analyzes disparities by race, ethnicity, and socioeconomic status, and for priority populations. Patient Safety Datasources HCUP SID Disparities Analytic File: Patient Safety Indicators (PSIs) Medicare Patient Safety Monitoring System: Adverse Events Quality Improvement Organization Program: Surgical Infection Prophylaxis Medical Expenditure Panel Survey: Inappropriate Medications Medicare Patient Safety Monitoring System Adverse events from charts RandomlyRandomly-selected, nationwide subset of inpatient medical records of Medicare beneficiaries Data weighted to produce national estimates Sample size: about 26,000 charts – 5,500 surgical cases – 4,000 central venous catheter insertions * AZ, CA, CO, CT, FL, GA, HI, KS, MD, MA, MI, MO, NH, NJ, NY, PA, PA, RI, SC, TN, TX, VA, VT, WI 1 Quality Improvement Organization Program Postoperative Complication Rates Relative to Whites, HCUP 2003 Quality of surgical infection prophylaxis from charts RandomlyRandomly-selected, nationwide subset of inpatient medical records of Medicare beneficiaries Sample size: about 21,000 surgical cases Wound dehiscence 1.50 1.17 Sepsis 1.54 PE/DVT Black Hispanic API 0.83 1.18 1.17 Respiratory failure 1.32 1.38 Metabolic derangement 2.05 1.22 Hemorrhage 1.30 0.0 0.5 1.0 1.5 2.0 2.5 3.0 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance Obstetric Complication Rates Relative to Whites, HCUP 2003 0.85 0.77 OB trauma, vaginal delivery Other Complication Rates Relative to Whites, HCUP 2003 Laceration 1.42 Infections 0.78 0.83 OB trauma, instruments OB trauma, Cesarean 0.79 0.5 1.0 1.54 0.84 0.75 0.75 Anesthesia 1.12 0.86 0.0 Black Hispanic API Foreign body Bedsores 1.44 Birth trauma 0.78 Pneumothorax Black Hispanic API Failure to rescue 1.5 2.0 2.5 3.0 1.17 0.0 0.5 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance Hispanic API Postop 0–1–5 0–3–3 1–3–2 Obstetric 2–1–1 4–0–0 0–3–1 Other 1–4–2 2–5–0 1–5–1 1.5 2.0 3–6–8 6–8–3 2 – 11 – 4 3.0 Black Postoperative Complication Rates Relative to Whites, MPSMS 2003 UTI PE/DVT Pneumonia Composite Total 2.5 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance Summary of PSIs Relative to Whites (Better(Better-SameSame-Worse) Black 1.0 1.66 0.0 0.5 1.0 1.5 2.0 2.5 3.0 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance 2 Black CVCCVC-Associated Complication Rates Relative to Whites, MPSMS 2003 Appropriate Surgical Infection Prophylaxis Relative to Whites, QIO 2004 BSI 1.20 Not received within 1 hr 0.78 Mechanical event Black Hispanic API AI/AN Insertion site infection 1.24 Not stopped within 24 hrs 1.27 Composite 1.22 0.0 0.5 1.0 1.5 2.0 2.5 3.0 0.0 0.5 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance 1.0 1.5 2.0 2.5 3.0 Bars with numbers included meet our statistical (p<0.05) and magnitude (>10% relative difference) criteria for significance Summary: Disparities in Hospital Safety “ComplicationComplication-Related” Related” Death Rates Per 1000 Discharge With Complications by Race/Ethnicity, HCUP 20012001-2003 HCUPHCUP-SID: Disparities exist 180 – Blacks and Hispanics have higher rates of postoperative complications – Hispanics have lower rates of obstetric complications – But fewer disparities related to other complications 170 Total White Black Hispanic API 160 150 140 MPSMS: Blacks have higher rates of postoperative but not CVCCVC-associated complications QIO: Surgical infection prophylaxis varies by race/ethnicity 130 120 2001 2002 2003 Note: “Complication-related” death rate = “failure to rescue” Summary: Trends in Hospital Safety Disparities Postoperative and CVC Complication Rates (%) by Race, MPSMS 20022002-2003 HCUPHCUP-SID: Disparities not narrowing MPSMS: BlackBlack-white differences in 12 10 8 2002 2003 6 4 CVCCVC-associated complications narrowing but not postoperative complications QIO: No data (yet) 2 0 Total White Black Postoperative Composite Total White Black CVC Composite 3 Next Steps: Why do these disparities exist? Minorities go to different hospitals or providers? Minorities are sicker when they are hospitalized? Minorities have more comorbidities? Procedures are harder to perform on minorities? Contact Information Ernest Moy, MD, MPH National Healthcare Quality and Disparities Reports Center for Quality Improvement and Patient Safety Agency for Healthcare Research and Quality 540 Gaither Road Rockville, MD, 20850 301301-427427-1329 (voice) 301301-427427-1341 (fax) Ernest.Moy@ahrq.hhs.gov 4